Study on D-dimer-to-albumin ratio combined with lactate in the short-term prognosis of sepsis patients in EICU
-
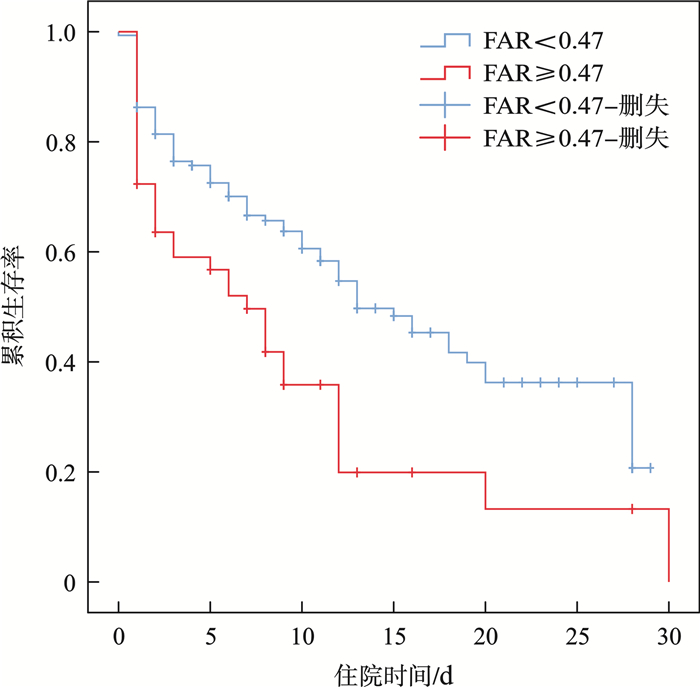
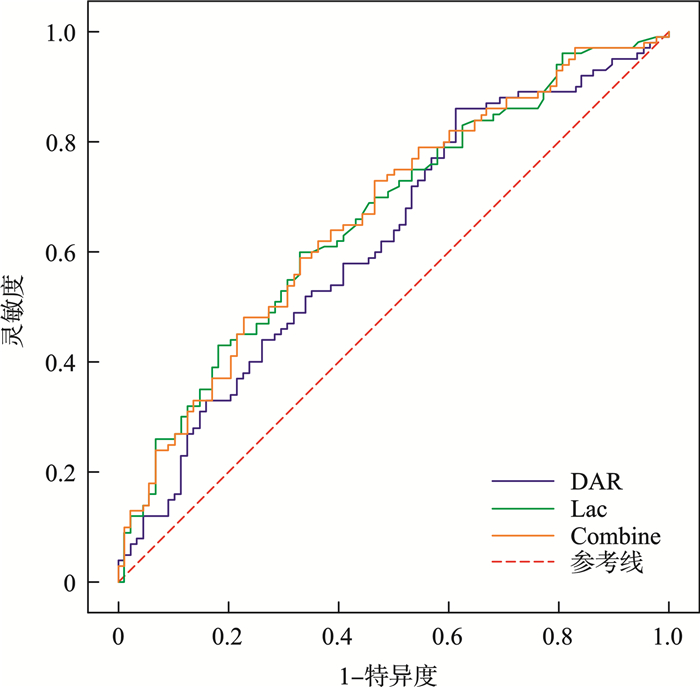
摘要: 目的 探讨D-二聚体(D-dimer,D-D)与白蛋白(albumin,ALB)比值(D-dimer to albumin ratio,DAR)联合乳酸(lactic acid,Lac)与EICU脓毒症患者严重程度和预后的相关性。方法 选择2018年8月—2024年6月入住河北医科大学哈励逊国际和平医院急救医学部EICU的符合脓毒症诊断条件的患者202例,记录患者性别、年龄、个人史及既往病史等情况,收集患者入院24 h内的序贯器官衰竭估计评分(sequential organ failure assessment,SOFA)及实验室常规检测指标:血常规、D-D、ALB、Lac、降钙素原(procalcitonin,PCT)等。根据2016年美国重症医学会(SCCM)与欧洲重症医学会(ESICM)联合发布脓毒症3.0定义及诊断标准将患者分为脓毒症组(97例)和脓毒性休克组(105例),比较两组患者的一般情况、炎性指标、组织灌注指标以及DAR,分析各指标间的相关性;随访28 d,根据存活与否分为存活组和死亡组,采用多因素logistic回归分析筛选脓毒症患者28 d死亡的危险因素;采用受试者工作特征曲线(ROC曲线)分析DAR对该类患者群的28 d死亡的预测价值。采用MedCalc软件比较常规观察指标与DAR评估的差异性。结果 与脓毒性休克组比较,脓毒症组患者中男性患者更多见(79.4%,P < 0.01);与脓毒症非休克组相比,脓毒性休克患者的DAR、Lac、PCT、以及SOFA评分均明显升高;脓毒症患者入EICU 24 h内的DAR与Lac、PCT均有一定的正相关,其中与SOFA评分相关性最强(r=0.512,P < 0.001)。绘制DAR及Lac预测脓毒症患者死亡预后的ROC曲线,结果显示,DAR对脓毒症患者28 d死亡预测价值较高(AUCDAR=0.660,AUCLac=0.618);经MedCalc软件分析,DAR评价脓毒症患者预后的灵敏度为85.5%,特异度为47.4%,最佳界值为0.47(Youden index=0.229);与Lac联合检测并未发现预测价值有明显提高(AUC联合=0.663,P>0.05)。Kaplan-Meier生存曲线显示,DAR≥0.47的脓毒症患者28 d病死率明显高于DAR < 0.47组(χ2=9.503,P=0.002),且EICU住院时间、接受机械通气比例与时间也明显增高(P < 0.05)。结论 DAR对EICU脓毒症患者的病情严重程度和预后评估有一定价值,联合Lac并未发现评估效能有更明显的增高。Abstract: Objective To investigate the correlation between the D-dimer(D-D) to albumin(ALB) ratio(DAR) combined with lactic acid(Lac) and the severity and prognosis of patients with sepsis in EICU.Methods A total of 202 patients in EICU admitted to Harrison International Peace Hospital Emergency Medicine Department of Hebei Medical University from August 2018 to June 2024 and qualified for the diagnosis of sepsis were selected. The patients'gender, age, personal history and past medical history were recorded, SOFA scores and laboratory routine test indexes including blood routine, D-D, ALB, Lac, procalcitonin(PCT) were collected within 24 h of admission. According to the sepsis 3.0 definition and diagnostic criteria jointly issued by SCCM and ESICM in 2016, patients were divided into sepsis group(97 cases)and septic shock group(105 cases), the general condition, inflammatory index and joint test index DAR were compared between the two groups. The correlation between inflammatory index and combination index was analyzed. The patients were followed up for 28 days and divided into survival group and death group according to survival, multivariate logistic regression analysis was used to screen the risk factors of death at 28 days in patients with sepsis. Receiver operating characteristic curve(ROC curve) was used to analyze the death prediction value of DAR for 28-day prognosis in this group of patients. MedCalc software was used to compare the difference between conventional inflammatory markers and combined markers in prognosis assessment.Results Compared with septic shock group, male patients with sepsis were more common(P < 0.01). Patients in sepsis group had longer length of stay in EICU(P < 0.01). The levels of DAR, Lac, PCT and SOFA score in septic shock group were significantly higher than those in non-septic shock group. DAR was positively correlated with infectious indexes(Lac, PCT) in sepsis patients within 24 hours of EICU admission. The correlation with SOFA was strongest(R=0.512, P < 0.001). The ROC curve of DAR and Lac for predicting the death prognosis of patients with sepsis was drawn. The results showed that DAR had a high predictive value for 28 d death in patients with EICU sepsis(AUCDAR=0.660, AUCLac=0.618). The sensitivity and specificity of DAR for the prognosis of sepsis patients were 85.5% and 47.4%, respectively, and the optimal boundary value was 0.47(Youden index=0.229). No higher predictive value was found in combination with Lac(AUCCombine=0.663, P>0.05). Kaplan-Meier survival curve showed that the 28 d mortality of sepsis patients with DAR≥0.47 was significantly higher than that of patients with DAR < 0.47, with statistical significance(χ2=9.503, P=0.002). The length of stay in EICU and mechanical ventilation in DAR≥0.47 group were significantly higher than those in DAR < 0.47 group, with statistical significance(P < 0.05).Conclusion DAR is useful in assessing the severity and prognosis of patients with EICU sepsis, the combined Lac is not found to be of higher application value.
-

-
表 1 脓毒症和脓毒性休克两组患者一般临床资料及入院24 h内DAR、感染指标比较
M(Q1,Q3),X±S 临床资料 脓毒症组(97例) 脓毒性休克组(105例) Z/χ2 P 男/% 79.4(77/97) 58.1(61/105) 10.555 0.001 年龄/岁 73.45±15.05 73.48±12.63 -0.012 0.991 EICU住院时间/d 4.0(1.0,12.0) 8.0(4.0,13.5) -2.956 0.003 微生物培养阳性检出率/% 27.8(27/97) 32.4(34/105) 0.494 0.482 28 d病死率/% 43.3(42/97) 65.4(68/105) 9.881 0.002 DAR 0.13(0.06,0.28) 0.28(0.11,0.72) -3.861 < 0.001 PCT/(μg/L) 1.76(25.82,155.83) 24.67(4.54,66.85) -5.988 < 0.001 Lac/(mmol/L) 2.40(1.59,3.86) 4.84(3.20,7.80) -5.024 < 0.001 SOFA评分/分 4.22±2.04 8.49±4.98 -20.790 < 0.001 表 2 入院24 h内DAR与Lac、PCT及SOFA评分相关性分析
指标 DAR r P PCT 0.308 < 0.001 Lac 0.387 < 0.001 SOFA评分 0.512 < 0.001 表 3 入院24 h内DAR与Lac及二者联合检测对28 d死亡预测价值分析
指标 AUC P 95%CI DAR 0.660 0.003 0.588~0.728 Lac 0.618 < 0.001 0.544~0.688 DAR联合Lac 0.663 < 0.001 0.591~0.731 表 4 不同DAR水平EICU脓毒症患者28 d结局比较
M(Q1,Q3),X±S 组别 例数 EICU住院时间/d SOFA评分/分 机械通气/% 28d病死率/% DAR < 0.47组 154 7(2.75,13.25) 9(4,13) 46.1(71/154) 49.4(76/154) DAR≥0.47组 48 6(1,9) 11(6,14) 70.8(34/48) 70.8(34/48) Z/χ2 -1.992 -1.680 -8.966 6.809 P 0.046 0.213 0.003 0.009 -
[1] Perner A, Cecconi M, Cronhjort M, et al. Expert statement for the management of hypovolemiain sepsis[J]. Intensive Care Med, 2018, 44(6): 791-798. doi: 10.1007/s00134-018-5177-x
[2] Prescott HC, Angus DC. Postsepsis morbidity[J]. JAMA, 2018, 319(1): 91. doi: 10.1001/jama.2017.19809
[3] Reinhart K, Daniels R, Kissoon N, et al. Recognizing Sepsis as a Global Health Priority-A WHO Resolution[J]. N Engl J Med, 2017, 377(5): 414-417. doi: 10.1056/NEJMp1707170
[4] Fleischmann-Struzek C, Schwarzkopf D, Reinhart K. Sepsis incidence in Germany and worldwide: Current knowledge and limitations of research using health claims data[J]. Med Klin Intensivmed Notfmed, 2022, 117(4): 264-268. doi: 10.1007/s00063-021-00777-5
[5] 郑瑞强, 张艺芬, 荣子琪, 等. 《拯救脓毒症运动: 脓毒症与感染性休克治疗国际指南2021版》解读与展望[J]. 中华危重病急救医学, 2021, 33(10): 1159-1164. doi: 10.3760/cma.j.cn121430-20211009-01442
[6] 钟铨, 钟雅, 吴清薇, 等. 血清标志物动态变异性预测脓毒症患者死亡风险的诊断效能[J]. 临床急诊杂志, 2024, 25(10): 509-515. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.10.001
[7] Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference[J]. Crit Care Med, 31(4): 1250-1256.
[8] Singer M, Deutschman Clifford S, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[9] Wang W, Liu CF. Sepsis heterogeneity[J]. World J Pediatr, 2023, 19(10): 919-927. doi: 10.1007/s12519-023-00689-8
[10] Vandewalle J, Libert C. Sepsis: a failing starvation response[J]. Trends Endocrinol Metab, 2022, 33(4): 292-304. doi: 10.1016/j.tem.2022.01.006
[11] Martín S, Pérez A, Aldecoa C. Sepsis and Immunosenescence in the Elderly Patient: A Review[J]. Front Med (Lausanne), 2017, 28, 4: 20. doi: 10.3389/fmed.2017.00020/pdf
[12] 蔡国龙, 童洪杰, 郝雪景, 等. 早期目标导向治疗对严重脓毒症/脓毒性休克患者病死率的影响: 系统文献回顾与Meta分析[J]. 中华危重病急救医学, 2015, (6): 439-442.
[13] Liang SY. Sepsis and Other Infectious Disease Emergencies in the Elderly[J]. Emerg Med Clin North Am, 2016, 34(3): 501-522. doi: 10.1016/j.emc.2016.04.005
[14] Casserly B, Phillips GS, Schorr C, et al. Lactate measurements in Sepsis-Induced tissue hypoperfusion: results from the surviving sepsis campaign database[J]. Crit Care Med, 2015, 43(3): 567-573. doi: 10.1097/CCM.0000000000000742
[15] Alobaidi R, Basu RK, Goldstein SL, et al. Sepsis-associated acute kidney injury[J]. Semin Nephrol, 2015, 35(1): 2-11. doi: 10.1016/j.semnephrol.2015.01.002
[16] 尹小燕, 徐兵, 吴莘, 洪二春, 王伟. D-二聚体联合血清白蛋白对急诊科老年脓毒症患者预后的评估[J]. 中国临床保健杂志, 2022, 25(1): 62-65.
[17] Protti A, Masson S, Latini R, et al. PersistenceofCen-tralVenous Oxygen Desaturation During Early SepsisIs Associated With Higher Mortality: A Retrospective Analysisofthe ALBIOS Trial[J]. Chest, 2018, 154(6): 1291-1300. doi: 10.1016/j.chest.2018.04.043
[18] 乔淑斐, 刘梦梦, 崔业惠, 等. S-腺苷同型半胱氨酸、乳酸和APACHEⅡ评分在脓毒症病情评估中的联合应用[J]. 临床急诊杂志, 2024, 25(9): 472-477. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.09.005
[19] Luo Y, Li L, Chen X, et al. Effects of lactate in immunosup-pression and inflammation: progress and prospects[J]. Int Rev Immunol, 2022, 41(1): 19-29. doi: 10.1080/08830185.2021.1974856
[20] Alataby H, Nfonoyim J, Diaz K, et al. The levels of lactate, troponin, and N-terminal pro-B-type natriuretic peptide are predictors of mortality in patients with sepsis and septic shock: a retrospective cohort study[J]. Med Sci Monit Basic Res, 2021, 27: e927834.
[21] 贾亚娟, 李潇风, 高志伟, 等. IL-37、PCT和CRP联合检测对急诊脓毒症患者28天预后的评估价值[J]. 临床急诊杂志, 2024, 25(9): 461-465, 471. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.09.003
[22] 赵刚, 单思阳, 何月月, 等HNL、PCT、sCD163及IL-6联合检测在老年患者脓毒症诊断中的应用价值[J]. 四川医学, 2024, 45(6): 582-586.
[23] 王军宇, 王宏伟, 刘温馨, 等. 降钙素原和血乳酸及病情严重程度评分对脓毒症患者预后的评估价值[J]. 中华危重病急救医学, 2019, 31(8): 938-941.
[24] 赵佳慧. 脓毒症与急性肾损伤[J]. 中国临床保健杂志, 2020, 23(6): 749-752.
[25] 杨志伟, 宋昆, 丁, 等. 血流感染患者死亡危险因素和血清白蛋白及感染部位对预后预测的临床研究[J]. 临床急诊杂志, 2023, 24(9): 464-469. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.09.005
-

计量
- 文章访问数: 151
- 施引文献: 0



 下载:
下载: