The combined application of S-adenosine homocysteine, lactic acid and APACHE Ⅱ scores in evaluating the severity of sepsis
-
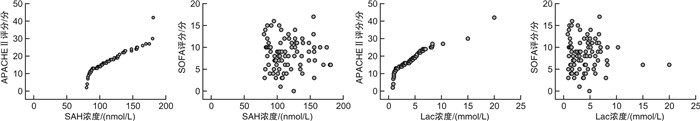
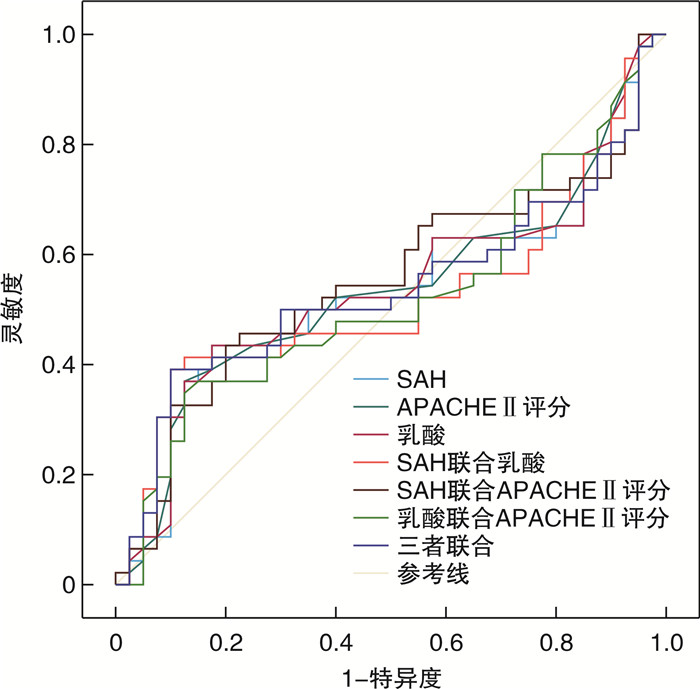
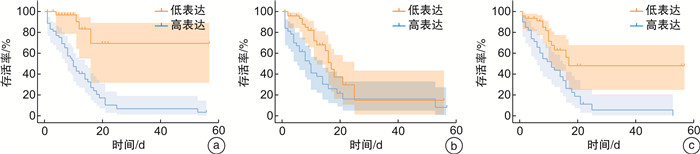
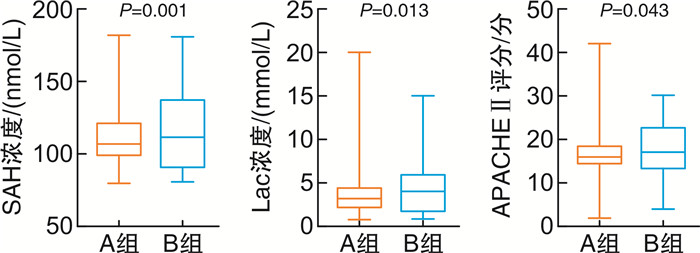
摘要: 目的 评估S-腺苷同型半胱氨酸(S-adenosine homocysteine,SAH)、乳酸(lactic acid,Lac)联合APACHEⅡ评分(acute physiology and chronic health evaluationⅡ,APACHEⅡ)在脓毒症患者不同病情严重程度中的价值。方法 回顾性分析2021年1月-2024年1月入住山西医科大学第二医院急诊科的86例脓毒症患者的临床资料,根据患者入院时是否存在休克分为脓毒症组(40例)和脓毒症休克组(46例)。比较两组患者的基本资料、早期疾病严重程度评分和早期血清学指标,寻找脓毒症病情严重程度的独立危险因素,绘制受试者工作特征曲线(receiver operating characteristic,ROC),探索相关指标评估脓毒症患者病情严重程度的价值。结果 两组患者的基本资料(如年龄、性别、感染部位等)比较差异无统计学意义(P>0.05)。脓毒症休克组SAH[(127.2±25.4) nmol/L]、Lac[(4.8±3.2) mmol/L]、APACHEⅡ评分[(17.5±6.4)分]明显高于脓毒症组[(100.2±17.9) nmol/L、(3.2±2.6) mmol/L、(14.9±5.3)分],且两组差异有统计学意义(P < 0.05);脓毒症患者SAH与APACHEⅡ评分、SOFA评分成正相关(P < 0.001)。SAH(OR=1.059,95%CI:1.032~1.092,P=0.001)、APACHEⅡ评分(OR=1.177,95%CI:1.019~1.360,P=0.027)是脓毒症患者疾病严重程度的独立影响因素。SAH、Lac的最佳截断值分别为102.5 nmol/L、4.1 mmol/L时预测脓毒症患者病情危重的AUC分别为0.833(95%CI:0.745~0.920,P < 0.001)、0.693(95%CI:0.581~0.806,P < 0.001),APACHEⅡ评分预测脓毒症患者病情危重的AUC为0.782(95%CI:0.684~0.881,P < 0.001);三者联合预测脓毒症患者病情危重的AUC为0.875(95%CI:0.803~0.947,P < 0.001)。结论 SAH、Lac、APACHE Ⅱ评分三者联合评估脓毒症疾病严重程度的价值较高,可为临床及时实施有效干预提供指导。
-
关键词:
- 脓毒症 /
- 脓毒症休克 /
- S-腺苷同型半胱氨酸 /
- 乳酸 /
- APACHE Ⅱ评分
Abstract: Objective To evaluate the value of S-adenosine homocysteine (SAH) and lactic acid(Lac) combined with acute physiology and chronic health evaluationⅡ(APACHEⅡ) score in different severity of patients with sepsis.Methods The clinical data of 86 patients with sepsis who were admitted to the emergency department of the Second Hospital of Shanxi Medical University from January 2021 to January 2024 according to sepsis 3.0 criteria were retrospectively analyzed. According to whether the patients had shock at admission, they were divided into sepsis group(40 cases) and septic shock group(46 cases). The basic data, early disease severity score and early serological indicators of the two groups were compared to find independent risk factors for the severity of sepsis, and receiver operating characteristic(ROC) was drawn. To explore the value of relevant indicators in evaluating the severity of sepsis.Results There was no significant difference in the basic information such as age, sex and infection site between the two groups(P>0.05). The scores of SAH([127.2±25.4]nmol/L), Lac([4.8±3.2] mmol/L)and APACHEⅡ([17.5±6.4]points)in septic shock group were significantly higher than those in sepsis group([100.2±17.9]nmol/L, [3.2±2.6]mmol/L, [17.5±6.4]mmol/L, [14.9±5.3] min), and the difference between the two groups was statistically significant(P < 0.05). SAH was positively correlated with APACHEⅡ score and SOFA score in sepsis patients(P < 0.001). SAH(OR=1.059, 95%CI: 1.032-1.092, P=0.001) and APACHEⅡ score(OR=1.177, 95%CI: 1.019-1.360, P=0.027) were independent factors of disease severity in sepsis patients. When the optimal cutoff values of plasma SAH and Lac were 102.5nmol/L and 4.1 mmol/L, respectively, the AUC for predicting critical illness in sepsis patients was 0.833(95%CI: 0.745-0.920, P < 0.001) and 0.693(95%CI: 0.581-0.806, P < 0.001), APACHEⅡ score predicted the AUC of patients with severe sepsis to be 0.782(95%CI: 0.684-0.881, P < 0.001); The combined prediction of AUC for severe sepsis was 0.875(95%CI: 0.803-0.947, P < 0.001).Conclusion SAH, Lac and APACHE Ⅱ are of high value in evaluating the severity of sepsis, which can provide guidance for clinical intervention in time. -

-
表 1 两组间资料比较
项目 脓毒症组(40例) 脓毒症休克组(46例) t/χ2/Z P 年龄/岁 59.9±14.8 62.7±13.5 -0.921 0.360 性别(男)/例(%) 24(60.00) 28(60.86) 0.007 0.935 感染部位/腹腔/例(%) 4(10.00) 17(36.96) 8.424 0.097 合并症/糖尿病/例(%) 13(32.50) 17(36.96) 0.187 0.802 心率/(次/min) 114.7±26.7 110.5±23.8 0.759 0.450 呼吸频率/(次/min) 22.7±3.6 23.0±5.7 -0.282 0.778 血氧饱和度/% 90.9±7.8 90.8±8.2 0.026 0.979 平均动脉压/mmHg 85.6±20.6 75.3±21.8 2.237 0.028 WBC/(×109/L) 12.0±8.0 14.5±10.6 -1.219 0.226 HGB/(g/L) 127.9±32.9 124.8±26.7 0.466 0.642 NEU/(×109/L) 11.2±7.8 12.9±9.3 -0.906 0.367 LYM/(×109/L) 0.9±1.1 0.9±1.5 -0.044 0.965 MON/(×109/L) 0.4±0.4 0.6±0.8 -1.110 0.270 HsC-rp/(mg/L) 144.8±96.6 170.7±82.4 -1.347 0.182 PCT/(ng/mL) 25.3±23.6 26.2±21.0 -0.198 0.843 ALT/(U/L) 94.2±142.2 82.3±127.2 0.410 0.683 AST/(U/L) 105.8±143.4 152.9±261.4 -1.013 0.314 TBil/(μmol/L) 37.2±42.9 31.0±31.0 0.775 0.192 ALB/(g/L) 32.2±8.4 31.1±7.7 0.657 0.513 Cr/(μmol/L) 173.0±203.3 257.7±273.1 -1.609 0.111 Urea/(mmol/L) 12.8±9.6 17.9±13.7 -1.998 0.049 SOFA评分/分 7.2±3.5 9.4±3.4 -2.977 0.004 qSOFA评分/分 1.2±0.9 1.5±0.8 -1.730 0.087 机械通气支持/例(%) 9(22.5) 20(43.5) -2.041 0.041 血液净化/例(%) 15(37.5) 28(60.9) -2.149 0.032 血管活性药物/例(%) 17(42.5) 40(87.0) -4.324 < 0.001 ICU住院时间/d 5.5±6.8 7.0±8.7 -0.846 0.398 28 d死亡率/% 30.00 43.35 2.217 0.137 表 2 两组间SAH、LAC、APACHEⅡ评分比较
指标 脓毒症组(40例) 脓毒症休克组(46例) t P SAH/(nmol/L) 100.2±17.9 127.2±25.4 -5.633 0.001 Lac/(mmol/L) 3.2±2.6 4.8±3.2 -2.537 0.013 APACHEⅡ评分/分 14.9±5.3 17.5±6.4 -2.060 0.043 表 3 SAH、LAC与APACHEⅡ评分、SOFA评分相关性(R)
指标 APACHEⅡ评分 SOFA评分 SAH 0.339 0.225 Lac 0.389 0.181 表 4 SAH、APACHEⅡ评分为脓毒症患者疾病严重程度的独立影响因素
项目 OR 95%CI P 平均动脉压/mmHg 0.976 0.941~1.012 0.182 SAH浓度/(nmol/L) 1.054 1.017~1.092 0.004 Lac浓度/(mmol/L) 1.162 0.937~1.440 0.171 APACHEⅡ评分/分 1.151 1.000~1.325 0.050 SOFA评分/分 1.020 0.820~1.269 0.857 是否机械通气支持 2.350 0.472~11.712 0.297 是否血液净化 1.233 0.354~4.293 0.742 是否使用血管活性药物 1.451 0.226~9.236 0.695 表 5 联合检测对脓毒症病情严重程度的评估价值分析
指标 截断值 AUC SE P 95%CI 灵敏度/% 特异度/% SAH 102.5 nmol/L 0.833 0.045 < 0.001 0.745~0.920 91.3 72.5 Lac 4.1 mmol/L 0.693 0.057 0.002 0.581~0.806 60.9 70.5 APACHEⅡ评分 16.5分 0.782 0.050 < 0.001 0.684~0.881 69.6 67.5 SAH+Lac - 0.862 0.040 < 0.001 0.783~0.941 - - SAH+APACHEⅡ评分 - 0.861 0.040 < 0.001 0.784~0.939 - - Lac+APACHEⅡ评分 - 0.782 0.050 < 0.001 0.684~0.881 - - 三者联合 - 0.875 0.037 < 0.001 0.803~0.947 - - -
[1] 李志军. 脓毒性休克中西医结合诊治专家共识[C]//江西中西医结合学会急救医学专业委员会. 江西省第十次中西医结合危重病、急救医学学术会议论文集. 中国中西医结合学会急救医学专业委员会, 2019: 7.
[2] Protti A, Masson S, Latini R, et al. Persistence of Central Venous Oxygen Desaturation During Early Sepsis Is Associated With Higher Mortality: A Retrospective Analysis of the ALBIOS Trial[J]. Chest, 2018.154(6): 1291-1300. doi: 10.1016/j.chest.2018.04.043
[3] Janotka M, Ostadal P. Biochemical markers for clinical monitoring of tissue perfusion[J]. Mol Cell Biochem, 2021, 476(3): 1313-1326. doi: 10.1007/s11010-020-04019-8
[4] Centner FS, Schoettler JJ, Brohm K, et al. S-Adenosylhomocysteine Is a Useful Metabolic Factor in the Early Prediction of Septic Disease Progression and Death in Critically Ill Patients: A Prospective Cohort Study[J]. Int J Mol Sci, 2023, 24(16): 12600. doi: 10.3390/ijms241612600
[5] 刘珍. 血浆肝素结合蛋白联合降钙素原及C-反应蛋白对脓毒症及脓毒性休克患者诊断价值的研究[J]. 中国卫生检验杂志, 2021, 31(22): 2696-2701. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202122003.htm
[6] You Y, Chen X, Chen Y, et al. Epigenetic modulation of Drp1-mediated mitochondrial fission by inhibition of S-adenosylhomocysteine hydrolase promotes vascular senescence and atherosclerosis[J]. Redox Biol, 2023, 65: 102828. doi: 10.1016/j.redox.2023.102828
[7] 张丹, 李宏飞, 闫梅, 等. 原发性高血压患者血清胱抑素C、同型半胱氨酸与靶器官损害的关系[J]. 岭南心血管病杂志, 2022, 28(6): 540-544. doi: 10.3969/j.issn.1007-9688.2022.06.10
[8] Cao L, Zhu T, Lang X, et al. Inhibiting DNA Methylation Improves Survival in Severe Sepsis by Regulating NF-κB Pathway[J]. Front Immunol, 2020, 11: 1360. doi: 10.3389/fimmu.2020.01360
[9] Semmler A, Prost JC, Smulders Y, et al. Methylation metabolism in sepsis and systemic inflammatory response syndrome[J]. Scand J Clin Lab Invest, 2013, 73(5): 368-372. doi: 10.3109/00365513.2013.785587
[10] Wexler O, Gough MS, Morgan MAM, et al. Methionine Metabolites in Patients With Sepsis[J]. J Intensive Care Med, 2018, 33(1): 37-47. doi: 10.1177/0885066616666002
[11] 邹洋洋, 姚莉. 离子钙水平联合乳酸清除率对心肺复苏后患者近期预后的评估[J]. 临床急诊杂志, 2023, 24(11): 573-577. doi: 10.13201/j.issn.1009-5918.2023.11.004
[12] Levy B, Desebbe O, Montemont C, et al. Increased aerobic glycolysis through beta2 stimulation is a common mechanism involved in lactate formation during shock states[J]. Shock, 2008, 30(4): 417-421. doi: 10.1097/SHK.0b013e318167378f
[13] Sterling SA, Puskarich MA, Jones AE. The effect of liver disease on lactate normalization in severe sepsis and septic shock: a cohort study[J]. Clin Exp Emerg Med, 2015, 2(4): 197-202. doi: 10.15441/ceem.15.025
[14] 许瑞涛, 李双凤, 黄淑雅, 等. 乳酸清除率联合多配体聚糖-1对脓毒性休克并急性呼吸窘迫综合征预后的预测价值[J]. 中华急诊医学杂志, 2023, 32(5): 660-666.
[15] 许镜清, 陈晗, 李俊, 等. 早期乳酸水平监测对血流感染相关脓毒性休克患者预后评价的价值[J]. 福建医科大学学报, 2020, 54(3): 166-170. https://www.cnki.com.cn/Article/CJFDTOTAL-FJYD202003008.htm
[16] 王铭, 吕晓雨, 罗雨青, 等. 早期监测PCT、CAR、D-二聚体结合ISS、APACHE Ⅱ评分对EICU创伤患者预后的评估价值[J]. 临床急诊杂志, 2023, 24(2): 51-57. doi: 10.13201/j.issn.1009-5918.2023.02.001
[17] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[18] 苏爱峰, 李云. 感染性休克患者血浆D-乳酸、肝素结合蛋白水平与APACHEⅡ评分的相关性分析[J]. 医学理论与实践, 2022, 35(18): 3064-3067. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL202218002.htm
-




 下载:
下载: