Predictive value of serum blood urea nitrogen levels for in-hospital mortality risk among sepsis patients in the intensive care unit
-
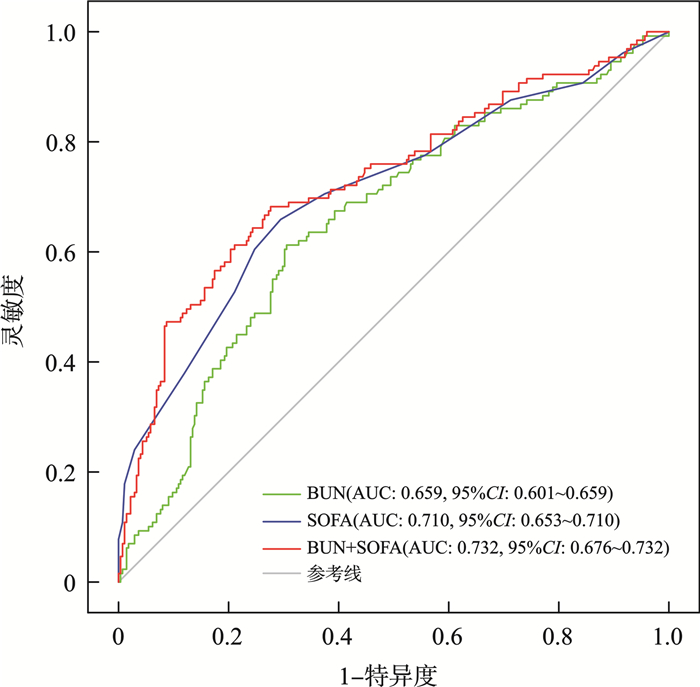
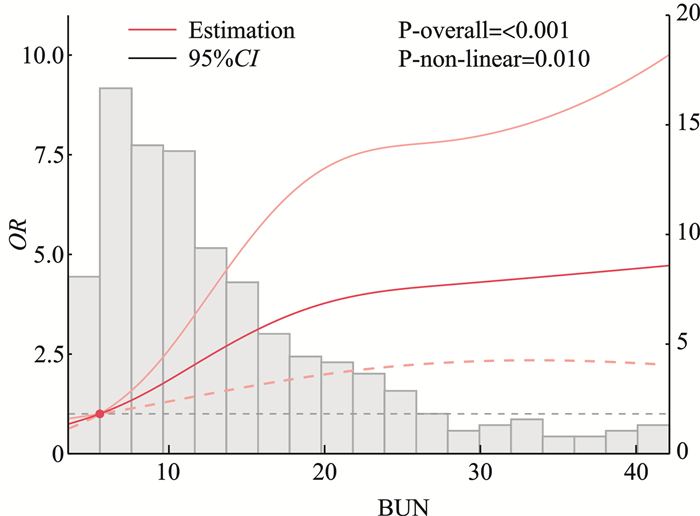
摘要: 目的 探讨血清尿素氮(blood urea nitrogen,BUN)水平对重症监护室脓毒症患者住院期间死亡风险的预测价值。方法 本研究为单中心、回顾性研究,纳入2018-2023年自贡市第四人民医院重症监护室收治的符合纳入标准的404例脓毒症患者。收集人口学特征、评分、实验室检查及干预措施等资料。将患者按入院时BUN中位数分为高、低BUN组,分析基线资料差异,并以住院期间死亡为终点,采用logistic回归分析探讨BUN与死亡风险的关系。利用限制性立方样条探讨BUN与住院期间全因死亡的剂量反应关系,绘制ROC曲线评估BUN、序贯性器官衰竭(sequential organ failure assessment,SOFA)评分及两者联合预测效果。结果 404例患者中,男性占63.12%,平均年龄为74.5岁,住院期间病死率为31.93%。高BUN组住院期间病死率(43.84%)显著高于低BUN组(19.90%)。多因素logistic回归分析显示,BUN(OR=1.045, 95%CI: 1.014~1.077,P=0.004)和SOFA评分(OR=1.267, 95%CI: 1.176~1.365,P < 0.001) 是住院期间死亡的独立危险因素。限制性立方样条分析表明,BUN与死亡风险呈非线性关系:当BUN < 5.563 mmol/L时具有保护作用,BUN高于该值后,死亡风险随之增加。BUN联合SOFA的AUC为0.732(0.676,0.732),高于单独的BUN、SOFA评分的预测效能。结论 BUN水平与ICU脓毒症患者住院期间死亡风险存在显著关联,BUN有助于提升SOFA评分对ICU脓毒症院内死亡的预测效能,为临床决策提供依据。Abstract: Objective To investigate the predictive value of serum blood urea nitrogen(BUN) levels for in-hospital mortality risk among sepsis patients in the intensive care unit(ICU).Methods This single-center, retrospective study included sepsis patients who met the inclusion criteria and were admitted to the ICU of Zigong Fourth People's Hospital between 2018 and 2023. Demographic data, clinical scores, laboratory tests, and interventions were collected. Patients were divided into high and low BUN groups based on the median BUN level at admission. Baseline differences between the groups were analyzed. In-hospital mortality was used as the endpoint. logistic regression analysis was employed to investigate the relationship between BUN levels and mortality risk. Restricted cubic spline models were applied to explore the dose-response relationship between BUN and all-cause in-hospital mortality. ROC curves were constructed to evaluate the predictive performance of BUN, sequential organ failure assessment(SOFA)score and their combination.Results A total of 404 patients were included, of whom 63.12% were male, with a mean age of 74.5 years. The in-hospital mortality was 31.93%. The high BUN group had a significantly higher in-hospital mortality than the low BUN group(43.84% vs. 19.90%). Multivariate logistic regression analysis revealed that BUN(OR=1.045, 95%CI: 1.014-1.077; P=0.004) and SOFA score(OR=1.267, 95%CI: 1.176-1.365; P < 0.001) were independent risk factors for mortality. Restricted cubic spline analysis demonstrated a nonlinear relationship between BUN and mortality risk: BUN levels below 5.563 mmol/L exhibited a protective effect, whereas higher BUN levels were associated with increased mortality risk. The combined area under the ROC curve for BUN and SOFA score was 0.732(95%CI: 0.676-0.732), significantly higher than that of BUN or SOFA score alone.Conclusion Serum BUN levels are significantly associated with the risk of in-hospital mortality in ICU patients with sepsis. Incorporating BUN enhances the predictive performance of the SOFA score for in-hospital mortality in septic ICU patients, thereby providing a basis for clinical decision-making.
-
Key words:
- sepsis /
- blood urea nitrogen /
- mortality risk /
- intensive care unit
-

-
表 1 患者基线特征分析
变量 总体(404例) 低BUN组(201例) 高BUN组(203例) 统计量 P 性别/例(%) χ2=2.163 0.141 男 255(63.12) 134(66.67) 121(59.61) 女 149(36.88) 67(33.33) 82(40.39) 年龄/岁 74.5(67.0,83.0) 73.0(66.0,81.0) 77.0(67.0,85.0) Z=-2.397 0.016 BUN/(mmol/L) 11.3(7.5,18.3) 7.5(5.8,9.2) 18.3(14.1,25.3) Z=-17.38 < 0.001 胱抑素C/(mg/L) 2.09(1.39,3.18) 1.43(1.09,1.78) 3.08(2.39,4.07) Z=-14.42 < 0.001 肌酐/(μmol/L) 118.1(76.2,198.5) 78.9(58.9,105.5) 182.5(125.9,273.6) Z=-12.87 < 0.001 UA/(μmol/L) 425.0(297.5,581.5) 327.0(245.0,437.0) 547.0(415.0,697.0) Z=-10.39 < 0.001 白细胞计数/(×109/L) 10.5(6.6,16.9) 9.5(6.4,14.7) 12.1(7.2,20.4) Z=-3.074 0.002 淋巴细胞计数/(×109/L) 0.500(0.290,0.925) 0.490(0.290,0.880) 0.520(0.300,0.930) Z=-0.263 0.792 中性粒细胞计数/(×109/L) 10.2(6.3,16.3) 9.5(5.9,14.6) 10.8(6.7,18.3) Z=-2.495 0.012 单核细胞数计数/(×109/L) 0.390(0.190,0.675) 0.360(0.190,0.590) 0.460(0.190,0.750) Z=-1.557 0.119 血红蛋白/(g/L) 111.0(89.0,130.0) 113.0(96.0,130.0) 108.0(83.0,128.0) Z=2.370 0.017 红细胞比容 0.342±0.080 0.349±0.074 0.334±0.086 t=1.972 0.049 血小板计数/(×109/L) 162.0(107.0,236.0) 162.0(108.0,237.0) 162.0(100.0,227.0) Z=0.411 0.680 D-二聚体/(mg/L) 4.72(2.09,10.41) 4.05(1.66,9.33) 5.63(2.66,11.59) Z=-3.016 0.002 凝血酶原时间/s 14.5(13.2,16.4) 13.9(12.7,15.6) 15.1(13.8,17.2) Z=-5.048 < 0.001 国际标准化比值 1.29(1.15,1.46) 1.22(1.12,1.37) 1.34(1.23,1.52) Z=-5.353 < 0.001 APTT/s 31.7(27.7,37.3) 30.9(26.8,34.9) 32.4(28.6,39.0) Z=-3.186 0.001 纤维蛋白原/(g/L) 4.27(3.16,5.78) 4.08(2.98,5.60) 4.50(3.26,5.88) Z=-1.330 0.183 钾/(mmol/L) 3.93(3.36,4.51) 3.62(3.19,4.13) 4.27(3.55,5.02) Z=-7.147 < 0.001 钠/(mmol/L) 138.0(133.7,142.5) 137.1(132.9,140.2) 139.7(134.3,145.0) Z=-4.442 < 0.001 氯/(mmol/L) 101.6(96.3,106.6) 100.0(95.6,104.2) 104.3(97.5,108.2) Z=-4.621 < 0.001 CRP/(mg/L) 113.9(55.8,159.1) 95.4(45.7,151.8) 130.2(68.2,168.4) Z=-3.014 0.002 丙氨酸氨基转移酶/(U/L) 27.0(17.4,54.0) 24.9(15.5,49.3) 29.5(18.1,70.9) Z=-2.673 0.007 天门冬氨酸氨基转移酶/(U/L) 43.4(26.1,97.1) 39.4(23.9,74.5) 51.5(27.8,111.2) Z=-2.768 0.005 白蛋白/(g/L) 29.2±6.0 29.8±6.3 28.5±5.6 t=2.277 0.023 球蛋白/(g/L) 29.1(24.9,33.2) 29.0(25.2,32.4) 29.5(24.5,33.9) Z=-0.452 0.651 SOFA评分/分 7.00(6.00,11.00) 7.00(5.00,9.00) 9.00(6.00,12.00) Z=-6.202 < 0.001 CCI指数 3.00(2.00,4.00) 2.00(1.00,4.00) 3.00(2.00,5.00) Z=-2.634 0.008 是否血液净化/例(%) χ2=2.942 0.086 否 540(93.75) 188(93.53) 180(88.67) 是 36(6.25) 13(6.47) 23(11.33) 住院期间死亡/例(%) χ2=26.636 < 0.001 死亡 129(31.93) 40(19.90) 89(43.84) 存活 275(68.07) 161(80.10) 114(56.16) 表 2 单因素和多因素logistic回归分析
因素 单因素分析 多因素分析 OR(95%CI) P OR(95%CI) P BUN 1.045(1.024~1.067) < 0.001 1.045(1.014~1.077) 0.004 UA 1.001(1.000~1.002) 0.077 0.999(0.997~1.000) 0.087 APTT 1.014(1.000~1.027) 0.051 0.995(0.980~1.011) 0.538 CRP 1.004(1.002~1.007) 0.003 1.003(1.000~1.006) 0.056 SOFA评分 1.283(1.196~1.376) < 0.001 1.267(1.176~1.365) < 0.001 是否血液净化 2.045(1.025~4.081) 0.042 1.373(0.613~3.073) 0.441 表 3 BUN联合SOFA评分与单因素比较的NRI、IDI值
项目 NRI(95%CI) P IDI(95%CI) P BUN+SOFA评分vs.BUN 0.650(0.451~0.849) < 0.001 0.115(0.081~0.150) < 0.001 BUN+SOFA评分vs.SOFA评分 0.400(0.198~0.602) < 0.001 0.018(0.003~0.032) 0.017 -
[1] Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med, 2021, 47(11): 1181-1247. doi: 10.1007/s00134-021-06506-y
[2] Vandewalle J, Libert C. Sepsis: a failing starvation response[J]. Trends Endocrinol Metab, 2022, 33(4): 292-304. doi: 10.1016/j.tem.2022.01.006
[3] Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the global burden of disease study[J]. Lancet, 2020, 395(10219): 200-211. doi: 10.1016/S0140-6736(19)32989-7
[4] 叶志澄, 李敏, 江慧琳, 等. SOFA、qSOFA、MEWS和SIRS四种危险评分对急诊监护室疑似感染患者28 d死亡的评估价值比较研究[J]. 中国急救医学, 2019, 39(11): 1084-1088. doi: 10.3969/j.issn.1002-1949.2019.11.015
[5] Nunnally ME, Ferrer R, Martin GS, et al. The Surviving Sepsis Campaign: research priorities for the administration, epidemiology, scoring and identification of sepsis[J]. Intensive Care Med Exp, 2021, 9(1): 34. doi: 10.1186/s40635-021-00400-z
[6] Haines RW, Zolfaghari P, Wan YZ, et al. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma[J]. Intensive Care Med, 2019, 45(12): 1718-1731. doi: 10.1007/s00134-019-05760-5
[7] Klaude M, Mori M, Tjäder I, et al. Protein metabolism and gene expression in skeletal muscle of critically ill patients with sepsis[J]. Clin Sci, 2012, 122(3): 133-142. doi: 10.1042/CS20110233
[8] Peerapornratana S, Manrique-Caballero CL, Gómez H, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment[J]. Kidney Int, 2019, 96(5): 1083-1099. doi: 10.1016/j.kint.2019.05.026
[9] Wernly B, Lichtenauer M, Vellinga NAR, et al. Blood urea nitrogen independently predicts mortality in critically ill patients admitted to ICU: a multicenter study[J]. Clin Hemorheol Microcirc, 2018, 69(1-2): 123-131. doi: 10.3233/CH-189111
[10] Arihan O, Wernly B, Lichtenauer M, et al. Blood urea nitrogen is independently associated with mortality in critically ill patients admitted to ICU[J]. PLoS One, 2018, 13(1): e0191697. doi: 10.1371/journal.pone.0191697
[11] Li XJ, Li TW, Wang JJ, et al. Higher blood urea nitrogen level is independently linked with the presence and severity of neonatal sepsis[J]. Ann Med, 2021, 53(1): 2192-2198.
[12] Beesley LJ, Bondarenko I, Elliot MR, et al. Multiple imputation with missing data indicators[J]. Stat Methods Med Res, 2021, 30(12): 2685-2700. doi: 10.1177/09622802211047346
[13] Zhang GY, Shao F, Yuan W, et al. Predicting sepsis in-hospital mortality with machine learning: a multi-center study using clinical and inflammatory biomarkers[J]. Eur J Med Res, 2024, 29(1): 156. doi: 10.1186/s40001-024-01756-0
[14] Harazim M, Tan KQ, Nalos M, et al. Blood urea nitrogen-independent marker of mortality in sepsis[J]. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 2023, 167(1): 24-29. doi: 10.5507/bp.2022.015
[15] Li X, Zheng RX, Zhang T, et al. Association between blood urea nitrogen and 30-day mortality in patients with sepsis: a retrospective analysis[J]. Ann Palliat Med, 2021, 10(11): 11653-11663. doi: 10.21037/apm-21-2937
[16] Min J, Lu JH, Zhong L, et al. The correlation study between blood urea nitrogen to serum albumin ratio and prognosis of patients with sepsis during hospitalization[J]. BMC Anesthesiol, 2022, 22(1): 404. doi: 10.1186/s12871-022-01947-4
[17] Garibotto G, Sofia A, Saffioti S, et al. Amino acid and protein metabolism in the human kidney and in patients with chronic kidney disease[J]. Clin Nutr, 2010, 29(4): 424-433. doi: 10.1016/j.clnu.2010.02.005
[18] Ou SM, Lee KH, Tsai MT, et al. Sepsis and the risks of long-term renal adverse outcomes in patients with chronic kidney disease[J]. Front Med, 2022, 9: 809292. doi: 10.3389/fmed.2022.809292
[19] Shi Y, Duan HY, Liu J, et al. Blood urea nitrogen to serum albumin ratio is associated with all-cause mortality in patients with AKI: a cohort study[J]. Front Nutr, 2024, 11: 1353956. doi: 10.3389/fnut.2024.1353956
[20] Weyker PD, Pérez XL, Liu KD. Management of acute kidney injury and acid-base balance in the septic patient[J]. Clin Chest Med, 2016, 37(2): 277-288. doi: 10.1016/j.ccm.2016.01.012
[21] Loyrion E, Agier L, Trouve-Buisson T, et al. Dynamic SOFA score assessments to predict outcomes after acute admission of octogenarians to the intensive care unit[J]. PLoS One, 2021, 16(8): e0253077. doi: 10.1371/journal.pone.0253077
[22] Kumar S, Gattani SC, Baheti AH, et al. Comparison of the performance of APACHE Ⅱ, SOFA, and mNUTRIC scoring systems in critically ill patients: a 2-year cross-sectional study[J]. Indian J Crit Care Med, 2020, 24(11): 1057-1061. doi: 10.5005/jp-journals-10071-23549
[23] Weng J, Hou RN, Zhou XM, et al. Development and validation of a score to predict mortality in ICU patients with sepsis: a multicenter retrospective study[J]. J Transl Med, 2021, 19(1): 322. doi: 10.1186/s12967-021-03005-y
[24] Wang YH, Gao S, Hong L, et al. Prognostic impact of blood urea nitrogen to albumin ratio on patients with sepsis: a retrospective cohort study[J]. Sci Rep, 2023, 13(1): 10013. doi: 10.1038/s41598-023-37127-8
-

计量
- 文章访问数: 81
- 施引文献: 0



 下载:
下载: