Diagnostic efficacy of dynamic variability of serum markers in predicting the risk of death in sepsis patients
-
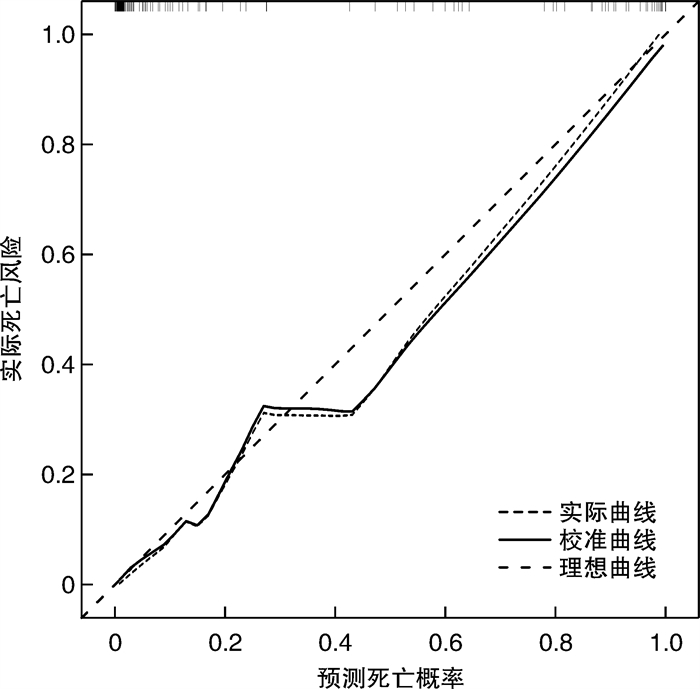
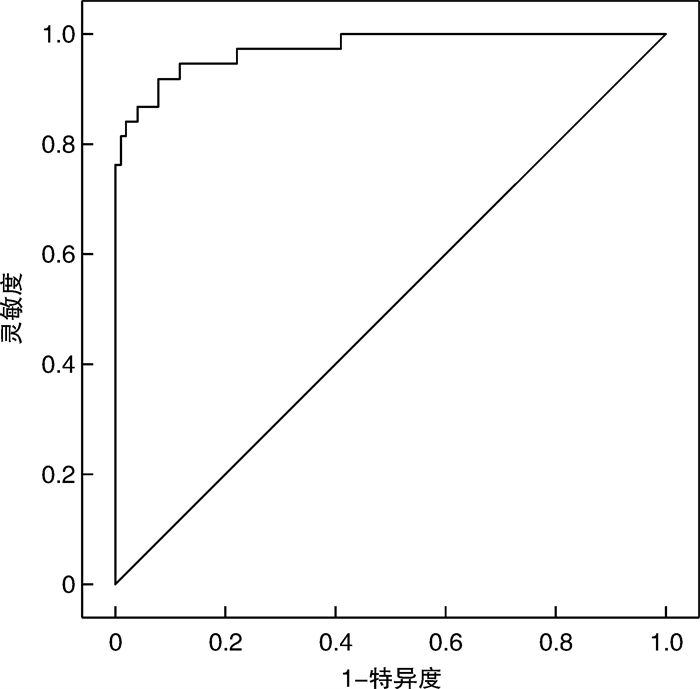
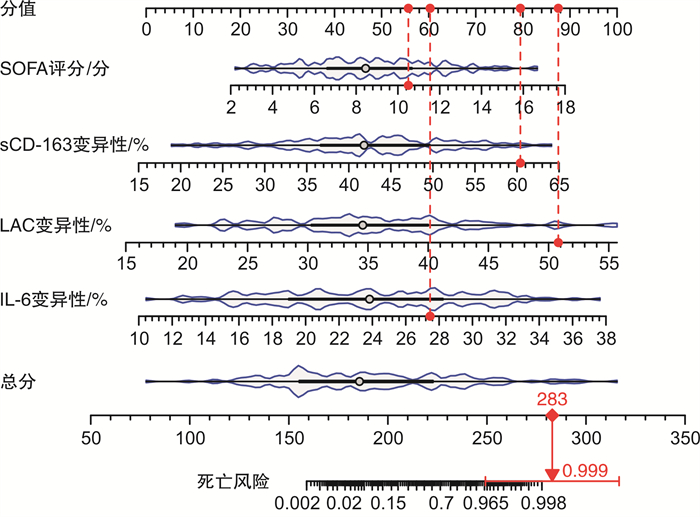
摘要: 目的 探讨血清学生物标志物的动态变异性与脓毒症患者死亡风险的相关性,构建基于血清学生物标志物的预测模型并评估其对脓毒症死亡风险的预测效能。方法 纳入2022年10月—2023年12月在海南医学院第一附属医院接受治疗的脓毒症患者138例,男71例,女67例。收集患者临床基线资料,于确诊第1天、第3天检测患者血清学指标[C-反应蛋白(C-reactive protein,CRP)、降钙素原(procalcitonin,PCT)、血乳酸(lactic acid,LAC)、白介素-6(interleukin-6,IL-6)、IL-8、IL-10、可溶性分化簇163(soluble cluster of differentiation 163,sCD163)、细胞间黏附分子-1(intercellular adhesion molecule-1,ICAM-1)],计算血清学指标变异率;采用序贯器官衰竭评分(sequential organ failure score,SOFA评分)对患者病情严重程度进行评估;随访28 d,根据患者28 d死亡情况分为死亡组(38例)和存活组(100例)。对比两组患者临床实验室资料,logistic回归分析脓毒症死亡风险的独立相关因素。使用R语言构建基于独立相关因素的列线图模型,绘制校正曲线和受试者工作特征曲线,评估模型在早预测脓毒症患者死亡风险的效能。结果 28 d随访结果显示,138例患者中,38例死亡,死亡率为27.54%。据此分组后对比临床资料显示,死亡组SOFA评分、IL-6变异率、IL-8变异率、LAC变异率、sCD163变异率高于存活组,差异有统计学意义(P < 0.05);logistic回归分析显示,IL-6变异率(OR=1.444)、SOFA评分(OR=1.559)、LAC变异率(OR=1.295)、sCD163变异率(OR=1.208)是脓毒症患者28 d死亡的独立相关因素(P < 0.05)。使用R语言基于独立相关因素绘制列线图模型,模型的C-指数为0.979(95%CI:0.965~0.998),校正曲线与理想曲线走形接近;列线图模型在早期预测脓毒症患者死亡的AUC为0.974,灵敏度为92.11%,特异度为92.00%。结论 通过分析血清学标志物的早期变异率能够准确预测脓毒症患者死亡风险,提高临床医生预警能力。Abstract: Objective To explore the correlation between the dynamic variability of serum biomarkers and the risk of mortality in patients with sepsis, to construct a predictive model based on serum biomarkers, and to evaluate its predictive efficacy for the risk of death in sepsis.Methods A total of 138 patients with sepsis treated in our hospital from October 2022 to December 2023 were included. Clinical baseline data of the patients were collected. On the first and third day of diagnosis, the following serum markers were measured: C-reactive protein(CRP), procalcitonin(PCT), lactic acid(LAC), interleukin-6(IL-6), IL-8, IL-10, soluble cluster of differentiation 163(sCD163), and Intercellular adhesion molecule-1(ICAM-1). The variability rate of the serum markers was calculated. The severity of the patients' conditions was assessed using the sequential organ failure score(SOFA). The patients were followed up for 28 days, and based on their 28-day mortality, they were divided into a deceased group(38 cases)and a survival group(100 cases). The clinical and laboratory data of the two groups were compared, and logistic regression analysis was performed to identify independent factors associated with the risk of death from sepsis. A nomogram model based on the independent factors was constructed using the R programming language, and calibration curves and receiver operating characteristic curves were plotted to evaluate the model's efficacy in early prediction of the risk of death in sepsis patients.Results After a 28-day follow-up, 38 out of 138 patients died, resulting in a mortality rate of 27.54%. After grouping, the clinical data showed that the SOFA score, IL-6 variability rate, IL-8 variability rate, LAC variability rate, and sCD163 variability rate were significantly higher in the deceased group compared to the survival group(P < 0.05). logistic regression analysis revealed that the IL-6 variability rate(OR=1.444), SOFA score(OR=1.559), LAC variability rate(OR=1.295), and sCD163 variability rate(OR=1.208) were independent factors associated with 28-day mortality in patients with sepsis(P < 0.05). Based on the independent factors, a nomogram model was constructed using the R programming language. The model's C-index was 0.979(95%CI: 0.965-0.998), and the calibration curve closely resembled the ideal curve. The AUC of the nomogram model for early prediction of death in sepsis patients was 0.974, with a sensitivity of 92.11% and a specificity of 92.00%.Conclusion Analysis of the early variability of serum markers can accurately predict the risk of death in patients with sepsis, enhancing the clinical physician's ability to provide early warnings.
-
Key words:
- serum biomarkers /
- dynamic variability /
- sepsis /
- prognosis
-

-
表 1 两组患者一般临床资料比较
X±S 项目 死亡组(38例) 存活组(100例) t/x2 P 性别/例(%) 0.029 0.864 男 20(52.63) 51(51.00) 女 18(47.37) 49(49.00) 平均年龄/岁 62.49±10.71 62.33±9.75 0.084 0.933 BMI/(kg/m2) 23.12±2.66 23.51±2.79 0.743 0.459 感染部位/例(%) 0.018 0.999 心血管系统 10(26.32) 22(22.00) 呼吸系统 15(39.47) 34(34.00) 泌尿系统 5(13.16) 12(12.00) 消化系统 7(18.42) 16(16.00) 其他 1(2.63) 16(16.00) 基础疾病/例(%) 1.436 0.697 冠心病 7(18.42) 16(16.00) 高血压病 10(26.32) 23(23.00) 糖尿病 8(21.05) 19(19.00) 慢性阻塞性肺疾病 5(13.16) 12(12.00) 无基础疾病 8(21.05) 30(30.00) 体温/℃ 37.85±1.33 37.94±1.47 0.329 0.742 HR/(次/min) 82.46±8.59 81.77±7.35 0.469 0.639 MAP/mmHg 64.22±7.36 65.71±6.88 1.115 0.267 SaO2/% 92.34±2.89 92.71±2.64 0.716 0.475 24 h尿量/mL 655±122 661±139 0.234 0.816 SOFA评分/分 11.62±2.33 8.31±2.97 6.180 < 0.001 AST/(IU/L) 23.33±5.71 23.19±5.38 0.134 0.893 ALT/(IU/L) 20.44±4.95 20.39±4.76 0.055 0.957 Scr/(μmol/L) 83.19±13.27 81.43±14.64 0.647 0.519 Alb/(g/L) 43.66±3.15 43.92±3.84 0.372 0.710 注:1 mmHg=0.133 kPa。 表 2 两组患者不同时间点血清学指标及变异率比较
血清学指标 死亡组(38例) 存活组(100例) t P CRP/(mg/L) 确诊时 87.14±10.33 85.31±10.29 0.932 0.353 确诊72 h 107.31±11.35 105.29±11.84 0.905 0.367 变异率/% 22.44±5.16 21.59±5.34 0.843 0.401 PCT/(ng/mL) 确诊时 0.97±0.11 0.95±0.13 0.840 0.402 确诊72 h 1.12±0.18 1.10±0.14 0.691 0.491 变异率/% 15.44±3.18 15.20±3.07 0.406 0.685 LAC/(mg/L) 确诊时 16.31±3.26 16.29±3.17 0.033 0.974 确诊72 h 23.05±3.16 21.57±3.04 2.527 0.013 变异率/% 41.27±7.88 33.44±6.39 6.019 < 0.001 IL-6/(pg/mL) 确诊时 133.29±14.57 130.54±15.82 0.932 0.353 确诊72 h 174.73±15.64 157.88±13.86 6.155 < 0.001 变异率/% 28.57±4.63 21.22±5.15 7.692 < 0.001 IL-8/(pg/mL) 确诊时 10.28±1.85 10.24±1.76 0.117 0.907 确诊72 h 12.33±2.02 11.74±1.92 1.589 0.114 变异率/% 19.88±3.22 15.31±3.04 7.761 < 0.001 IL-10/(pg/mL) 确诊时 1.34±0.21 1.33±0.19 0.268 0.789 确诊72 h 1.42±0.19 1.40±0.25 0.446 0.656 变异率/% 9.73±2.31 9.65±2.44 0.175 0.862 sCD163/(ng/mL) 确诊时 159.82±33.79 156.39±32.45 0.548 0.584 确诊72 h 242.68±37.28 215.44±30.73 4.379 < 0.001 变异率/% 51.31±9.42 38.57±8.69 7.516 < 0.001 ICAM-1/(μg/mL) 确诊时 189.48±22.77 187.29±23.64 0.491 0.624 确诊72 h 202.36±24.52 200.48±25.69 0.389 0.698 变异率/% 6.58±2.34 6.42±2.76 0.316 0.752 表 3 脓毒症患者死亡的单因素分析
相关变量 β SE Wald χ2 P OR 95%CI SOFA评分 0.348 0.079 19.447 < 0.001 1.417 1.214~1.654 LAC变异率 0.193 0.038 25.451 < 0.001 1.213 1.125~1.308 IL-6变异率 0.293 0.055 28.163 < 0.001 1.341 1.203~1.494 IL-8变异率 0.145 0.064 5.161 0.023 1.156 1.020~1.310 sCD163变异率 0.127 0.028 21.071 < 0.001 1.135 1.075~1.198 LAC 0.051 0.067 0.586 0.444 1.053 0.923~1.201 IL-6 0.070 0.016 20.030 < 0.001 1.073 1.040~1.107 sCD163 0.037 0.007 24.163 < 0.001 1.037 1.022~1.053 表 4 脓毒症患者死亡的logistic回归分析
相关指标 β SE Wald χ2 P OR 95%CI SOFA评分 0.444 0.159 7.859 0.005 1.559 1.143~2.128 LAC变异率 0.259 0.082 9.832 0.002 1.295 1.102~1.522 IL-6变异率 0.368 0.089 17.132 < 0.001 1.444 1.214~1.719 IL-8变异率 0.079 0.115 0.470 0.493 1.082 0.864~1.354 sCD163变异率 0.189 0.054 12.435 < 0.001 1.208 1.088~1.342 常量 -33.870 6.913 24.004 < 0.001 0.000 -
[1] 贺小丽, 李德渊, 乔莉娜, 等. 脓毒症流行病学及预后的研究进展[J]. 中华危重病急救医学, 2018, 30(5): 486-489.
[2] 郑瑞强, 张艺芬, 荣子琪, 等. 《拯救脓毒症运动: 脓毒症与感染性休克治疗国际指南2021版》解读与展望[J]. 中华危重病急救医学, 2021, 33(10): 1159-1164.
[3] 苏晓清, 闫世杰, 徐谦, 等. 创伤性脓毒症患者IL-1β、IL-6、IL-18、TNF-α水平变化分析[J]. 河北医药, 2021, 43(18): 2755-2758.
[4] Seymour CW, Gesten F, Prescott HC, et al. Time to treatment and mortality during mandated emergency care for sepsis[J]. N Engl J Med, 2017, 376(23): 2235-2244. doi: 10.1056/NEJMoa1703058
[5] Wang XS, Guo Z, Chai Y, et al. Application prospect of the SOFA score and related modification research progress in sepsis[J]. J Clin Med, 2023, 12(10): 3493. doi: 10.3390/jcm12103493
[6] 中国医师协会急诊医师分会, 中国研究型医院学会休克与脓毒症专业委员会, 中国人民解放军总医院第一附属医院创伤研究中心, 等. 中国脓毒症/脓毒性休克急诊治疗指南(2018)[J]. 临床急诊杂志, 2018, 19(9): 567-588. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2018.09.001
[7] 王娜, 王丰容, 刘芦姗, 等. eSOFA评分在脓毒症患者28、90天及1年预后评估中的作用[J]. 中国急救医学, 2023, 43(9): 711-715.
[8] Akoumianaki T, Vaporidi K, Diamantaki E, et al. Uncoupling of IL-6 signaling and LC3-associated phagocytosis drives immunoparalysis during sepsis[J]. Cell Host Microbe, 2021, 29(8): 1277-1293. e6.
[9] Kadota N, Yoshida A, Sawamoto A, et al. Ibudilast reduces IL-6 levels and ameliorates symptoms in lipopolysaccharide-induced sepsis mice[J]. Biol Pharm Bull, 2022, 45(8): 1180-1184.
[10] 陈君, 王妮, 陈栩栩, 等. ICU脓毒症患者血清Presepsin、内毒素、IL-6、PCT水平与预后的相关性[J]. 中华医院感染学杂志, 2022, 32(3): 356-359.
[11] Das UN. Infection, inflammation, and immunity in sepsis[J]. Biomolecules, 2023, 13(9): 1332.
[12] Lan L, Zhou MC, Chen XL, et al. Prognostic accuracy of SOFA, MEWS, and SIRS criteria in predicting the mortality rate of patients with sepsis: a meta-analysis[J]. Nurs Crit Care, 2023, Online ahead of print. .
[13] Lu Y, Song L. Clinical significance of procalcitonin, lactic acid, and endotoxin testing for children with severe pneumonia and sepsis[J]. Altern Ther Health Med, 2023, 29(3): 218-223.
[14] 邸晨义, 任炳魁, 陈思莹, 等. 血乳酸参数在老年脓毒症患者中的评估价值和最佳阈值探索[J]. 中华老年医学杂志, 2023, 42(12): 1435-1441.
[15] Jiang MN, Wu WD, Wang XZ, et al. Analysis of the predictive effect of lactic acid combined with cardiac troponin T and 5-hydroxytryptophan on the severity of sepsis in ICU patients and its correlation with prognosis[J]. Contrast Media Mol Imaging, 2022, 2022: 6215282.
[16] Chen T, Liu YJ, Tang Y, et al. Use of cardiac troponin I, lactic acid, procalcitonin, and serum complement C3 as prognostic indicators in patients with sepsis[J]. Medicine, 2023, 102(52): e36724.
[17] Suo SZ, Luo LY, Song YK, et al. Early diagnosis and prediction of death risk in patients with sepsis by combined detection of serum PCT, BNP, lactic acid, and ApacheⅡscore[J]. Contrast Media Mol Imaging, 2022, 2022: 8522842.
[18] Mierzchała-Pasierb M, Lipińska-Gediga M, Lewandowski Ł, et al. Alterations in serum concentration of soluble CD163 within five study days from ICU admission are associated with in-hospital mortality of septic patients-a preliminary study[J]. Int J Environ Res Public Health, 2023, 20(3): 2263.
[19] Qiu X, Lei YP, Zhou RX. SIRS, SOFA, qSOFA, and NEWS in the diagnosis of sepsis and prediction of adverse outcomes: a systematic review and meta-analysis[J]. Expert Rev Anti Infect Ther, 2023, 21(8): 891-900.
[20] Lee HJ, Ko BS, Ryoo SM, et al. Modified cardiovascular SOFA score in sepsis: development and internal and external validation[J]. BMC Med, 2022, 20(1): 263.
-

计量
- 文章访问数: 310
- 施引文献: 0



 下载:
下载: