Effect of PI combined with Pv-aCO2/Ca-vO2 on prognosis and lactic acid clearance in patients with septic shock
-
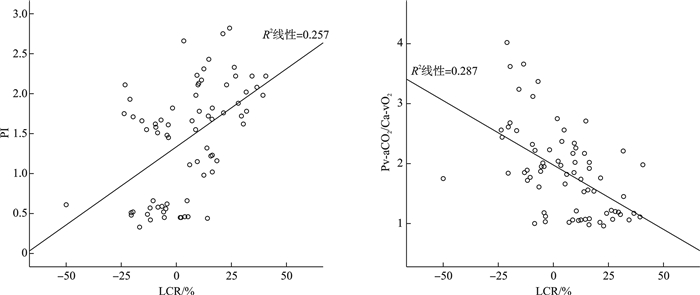
摘要: 目的 探索外周灌注指数(perfusion index,PI)联合中心静脉-动脉二氧化碳分压差与动脉-中心静脉氧含量差比值(Pv-aCO2/Ca-vO2)在脓毒性休克患者病情评估中的作用。方法 河北医科大学哈励逊国际和平医院EICU 2021年8月—2024年8月72例脓毒性休克患者,根据初始复苏3 h PI将患者分为两组:A组PI≥1.4,B组PIx 1.4;A组患者依据Pv-aCO2/Ca-vO2再分为A1和A2两个亚组:A1组Pv-aCO2/Ca-vO2≤1.23,A2组Pv-aCO2/Ca-vO2>1.23。比较3组患者血流动力学参数、氧代谢参数、乳酸清除率(lactate clearance group,LCR)、入ICU时及第3天急性生理与慢性健康状况评分Ⅱ(acute physiology and chronic health evaluation Ⅱ,APACHEⅡ)、序贯器官衰竭评分(sequential organ failure assessmentin,SOFA)及28 d病死率。结果 B组第3天APACHEⅡ评分和SOFA评分、28 d病死率均高于A1组,差异有统计学意义(P < 0.05);A2组T3 d APACHEⅡ评分、T3 d SOFA评分、28 d病死率均高于A1组,差异有统计学意义(均P < 0.05)。A1组3 h LCR高于A2组和B组,差异有统计学意义(P < 0.05)。Spearman相关分析显示PI与LCR呈正相关(r=0.507,P < 0.001),Pv-aCO2/Ca-vO2与LCR呈负相关(r=-0.536,P < 0.001)。结论 脓毒性休克患者初始液体复苏3 h PI、Pv-aCO2/Ca-vO2与乳酸清除率相关,PI联合Pv-aCO2/Ca-vO2可初步评估预后,复苏3 h PI≥1.4,Pv-aCO2/Ca-vO2≤1.23预后最佳。
-
关键词:
- 脓毒性休克 /
- 外周灌注指数 /
- 中心静脉-动脉二氧化碳分压差与动脉-中心静脉氧含量差比值 /
- 评估
Abstract: Objective The role of peripheral perfusion index(PI) combined with central venous arterial carbon dioxide partial pressure difference/arterial central venous oxygen content difference(Pv-aCO2/Ca-vO2) in the assessment of septic shock patients.Methods From August 2021 to August 2024, there were 72 patients with septic shock at the Harbin International Peace Hospital EICU of Hebei Medical University, According to the initial 3-hour recovery PI, patients were divided into two groups: group A had a PI ≥ 1.4, while group B had a PI < 1.4. Group A patients were further divided into two subgroups, A1 and A2, based on Pv-aCO2/Ca-vO2: group A1 had Pv-aCO2/Ca-vO2 ≤ 1.23, while group A2 had Pv-aCO2/Ca-vO2>1.23. Hemodynamic parameters, oxygen metabolism, lactate clearance rate, acute physiology and chronic health evaluation Ⅱ(APACHE Ⅱ) and the sequential organ failure assessmentin(SOFA) scores at the time of admission and 3 days, and 28-day mortality rate were compared among the three groups. and then two groups were divided according to the lactic acid clearance rate: the lactate clearance group(LCR≥10%) and the lactate non-clearance group(LCR < 10%). The influencing factors of lactate clearance < 10% were analyzed by binary logistic regression model, and the correlation between PI, Pv-aCO2/Ca-vO2 and LCR was analyzed by Spearman correlation analysis.Results The LCR in group A1 was higher than that in group A2 and group B, and the difference was statistically significant(P < 0.05). APACHE Ⅱand SOFA at 3 d and 28-day mortality rate in group B were higher than in group A1(P < 0.05). APACHE Ⅱ and SOFA at 3 d and 28-day mortality rate in group A2 were higher than in group A1(P < 0.05). Binary logistic regression model analysis showed that PI(OR=0.169, 95%CI: 0.043-0.668, P=0.011), Pv-aCO2/Ca-vO2(OR=7.666, 95%CI: 1.760-33.386, P=0.007) were the independent risk factors for lactic acid clearance < 10%. Spearman correlation analysis showed that PI was positively correlated with LCR(r=0.507, P < 0.001), and Pv-aCO2/Ca-vO2was negatively correlated with LCR(r=-0.536, P < 0.001).Conclusion PI and Pv-aCO2/Ca-vO2is correlated with LCR in patients with septic shock, and the combination of PI and Pv-aCO2/Ca-vO2 is helpful to evaluate the prognosis. Patients with PI≥1.4, Pv-aCO2/Ca-vO2≤1.23 had the best prognosis. -

-
表 1 一般资料比较 X±S
指标 A1组(23例) A2组(20例) B组(29例) F/χ2 P 年龄/岁 64.70±7.42 66.25±9.37 66.72±6.68 0.463 0.632 男性/例(%) 14(60.87) 10(50) 15(51.72) 0.390 0.532 感染部位/例(%) 0.334 0.563 肺部 10(43.48) 9(45) 14(48.28) 腹腔 8(34.78) 7(35) 10(34.48) 尿路 2(8.70) 2(10) 3(10.34) 血流 3(13.04) 2(10) 2(6.90) 去甲肾上腺素/(μg/kg/min) 0.54±0.11 0.60±0.15 0.56±0.10 1.589 0.212 APACHEⅡ评分/分 18.39±2.35 20.20±3.27 22.10±3.791)2) 8.431 0.001 SOFA评分/分 8.61±2.27 10.30±1.751) 10.31±2.421) 4.632 0.013 机械通气/例(%) 11(47.8) 9(45.0) 14(48.3) 0.222 0.637 机械通气参数 吸入氧浓度/% 46.22±4.63 47.25±5.31 52.43±6.76 0.183 1.036 潮气量/(mL/kg) 6.83±1.57 6.49±1.53 6.17±1.35 0.298 0.778 呼气末正压/mmHg 6.64±1.92 6.81±2.06 7.10±1.98 0.207 0.832 PCT/(ng/mL) 8.16±3.04 15.58±8.241) 16.83±8.121) 10.970 < 0.001 WBC/(×109/L) 13.34±4.37 14.28±3.21 13.69±3.75 0.230 0.795 初步复苏液量/(mL/kg) 32.1±1.0 31.6±1.0 31.5±0.9 1.958 0.149 与A1组相比,1)P < 0.05;与A2组相比,2)P < 0.05。 表 2 初始复苏时血流动力学与氧代谢指标比较
X±S 指标 A1组(23例) A2组(20例) B组(29例) F P MAP/mmHg 74.48±6.22 78.70±8.19 76.38±6.30 2.032 0.139 CVP/mmHg 8.48±1.97 7.40±1.98 7.86±2.31 1.410 0.251 HR/(次/min) 91.39±10.02 95.25±10.28 102.93±11.771)2) 8.107 0.001 ScvO2/% 69.74±3.14 68.55±3.83 67.90±3.62 1.758 0.180 Lac/(mmol/L) T0 4.81±1.40 4.75±1.29 5.15±1.70 0.945 0.394 T3 h 3.02±1.623) 4.54±1.391) 5.34±1.691) 3.552 0.034 LCR3 h/% 27.21±13.73 2.89±19.521) -2.37±15.221) 10.089 < 0.001 PI 1.93±0.39 1.94±0.30 0.69±0.311)2) 122.700 < 0.001 P(v-a)CO2/C(a-v)O2 1.09±0.08 2.55±0.721) 2.01±0.361)2) 59.970 < 0.001 与A1组相比,1)P < 0.05;与A2组相比,2)P < 0.05;与T0相比,3)P < 0.05。 表 3 各组预后指标比较
X±S 指标 A1组(23例) A2组(20例) B组(29例) F/χ2 P T3 d APACHEⅡ评分/分 12.16±3.39 16.23±3.981) 19.62±5.771) 7.782 0.024 T3 d SOFA评分/分 4.41±2.53 6.73±2.091) 9.94±4.511) 4.526 0.018 28 d病死率/例(%) 5(21.74) 11(55.00)1) 21(72.41)1) 13.330 0.001 与A1组相比,1)P < 0.05。 -
[1] Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children[J]. Intensive Care Med, 2020, 46(1): 10-67. http://doc.paperpass.com/foreign/rgArti20206778581.html
[2] 刘炳炜, 徐燕平, 席绍松, 等. SOFA评分联合PCT检测对脓毒症患者病情及其预后的临床评估价值[J]. 中华全科医学, 2021, 19(3): 391-393.
[3] 严颜, 魏捷, 吴淼, 等. 脓毒症的微循环监测与管理: 从临床实践出发[J]. 临床急诊杂志, 2024, 25(2): 99-104. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.02.009
[4] Desposito L, Bascara C. Review: sepsis guidelines and core measure bundles[J]. Postgrad Med, 2024, 136(7): 702-711. doi: 10.1080/00325481.2024.2388021
[5] 顾晓蕾, 庾胜, 龚菊, 等. 基于中心静脉-动脉血二氧化碳分压差及乳酸清除率的早期个体化液体复苏策略在脓毒性休克患者中的疗效研究[J]. 临床急诊杂志, 2024, 25(7): 343-347. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.07.004
[6] Chi C, Gong H, Yang K, et al. Early peripheral perfusion index predicts 28-day outcome in patients with septic shock[J]. World J Emerg Med, 2024, 15(5): 372-378. doi: 10.5847/wjem.j.1920-8642.2024.081
[7] 钱雅君, 虞竹溪, 李静, 等. 脓毒性休克患者脑氧饱和度监测对患者转归的预测价值[J]. 临床急诊杂志, 2023, 24(5): 225-229, 236. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.05.001
[8] Zhou XF, Yu RG, Chen Q, et al. Performance of lactate and CO2-derived parameters in predicting major postoperative complications after cardiac surgery with cardiopulmonary bypass: protocol of a diagnostic accuracy study[J]. Front Cardiovasc Med, 2021, 8: 724713. doi: 10.3389/fcvm.2021.724713
[9] Schlapbach LJ, Watson RS, Sorce LR, et al. International consensus criteria for pediatric sepsis and septic shock[J]. JAMA, 2024, 331(8): 665-674. doi: 10.1001/jama.2024.0179
[10] Sun XT, He HW, Xu MR, et al. Peripheral perfusion index of pulse oximetry in adult patients: a narrative review[J]. Eur J Med Res, 2024, 29(1): 457. doi: 10.1186/s40001-024-02048-3
[11] He HW, Liu DW, Long Y, et al. High central venous-to-arterial CO2 difference/arterial-central venous O2 difference ratio is associated with poor lactate clearance in septic patients after resuscitation[J]. J Crit Care, 2016, 31(1): 76-81. doi: 10.1016/j.jcrc.2015.10.017
[12] 任娜, 刘名胜, 周森. 液体复苏前后外周灌注指数水平对脓毒性休克患者28 d死亡风险预测价值的研究[J]. 临床急诊杂志, 2021, 22(6): 377-382. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2021.06.003
[13] de Miranda AC, De Stefani FDC, Dal Vesco BC, et al. Peripheral ischemic reserve in sepsis and septic shock as a new bedside prognostic enrichment tool: a Brazilian cohort study[J]. PLoS One, 2023, 18(7): e0288249. doi: 10.1371/journal.pone.0288249
[14] Porizka M, Kopecky P, Dvorakova H, et al. Methylene blue administration in patients with refractory distributive shock-a retrospective study[J]. Sci Rep, 2020, 10: 1828. doi: 10.1038/s41598-020-58828-4
[15] Wang C, Wang XT, Zhang HM, et al. Association between Doppler snuffbox resistive index and tissue perfusion in septic patients[J]. Shock, 2020, 54(6): 723-730. doi: 10.1097/SHK.0000000000001547
[16] Toledo-Salinas O, Pereyra-Guzmán E. Correlation between the shock index and the anaerobic index[J]. Rev Med Inst Mex Seguro Soc, 2023, 61(3): 307-313.
[17] Taiana M, Tomasella I, Russo A, et al. Analysis of P(v-a)CO2/C(a-v)O2 ratio and other perfusion markers in a population of 98 pediatric patients undergoing cardiac surgery[J]. J Clin Med, 2023, 12(17): 5700.
[18] 马乐, 田家豪, 李艺佩, 等. Pv-aCO2/Ca-vO2联合血乳酸对儿童原发性腹膜炎相关脓毒性休克预后的预测价值[J]. 中华危重病急救医学, 2023, 35(1): 77-81.
[19] Sindhu K, Malviya D, Parashar S, et al. Correlation of central venous-to-arterial carbon dioxide difference to arterial-central venous oxygen difference ratio to lactate clearance and prognosis in patients with septic shock: a prospective observational cohort study[J]. Int J Crit Illn Inj Sci, 2022, 12(3): 146-154.
[20] Ferrara G, Kanoore Edul VS, Caminos Eguillor JF, et al. Effects of fluid and norepinephrine resuscitation in a sheep model of endotoxin shock and acute kidney injury[J]. J Appl Physiol, 2019, 127(3): 788-797. http://www.zhangqiaokeyan.com/journal-foreign-detail/0704025347614.html
[21] Conner J, Lammers D, Holtestaul T, et al. Combatting ischemia reperfusion injury from resuscitative endovascular balloon occlusion of the aorta using adenosine, lidocaine and magnesium: a pilot study[J]. J Trauma Acute Care Surg, 2021, 91(6): 995-1001. http://pubmed.ncbi.nlm.nih.gov/34446655/
[22] Huber W, Zanner R, Schneider G, et al. Assessment of regional perfusion and organ function: less and non-invasive techniques[J]. Front Med, 2019, 6: 50. http://www.xueshufan.com/publication/2922666335
[23] 邹洋洋, 姚莉. 离子钙水平联合乳酸清除率对心肺复苏后患者近期预后的评估[J]. 临床急诊杂志, 2023, 24(11): 573-577. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.11.004
[24] 刘先, 弋佳君, 范秋宏. 去甲肾上腺素超早期使用对感染伴低血压的老年患者的预后影响[J]. 临床急诊杂志, 2023, 24(11): 578-582, 589. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.11.005
[25] 何招辉, 杨小刚, 杨春丽, 等. 下腔静脉变异度联合中心静脉-动脉血二氧化碳分压差指导脓毒性休克患者液体复苏的疗效分析[J]. 中华危重病急救医学, 2022, 34(1): 18-22.
-

计量
- 文章访问数: 90
- 施引文献: 0



 下载:
下载: