Construction of short-term prognosis prediction model for sepsis patients caused by pulmonary infection
-
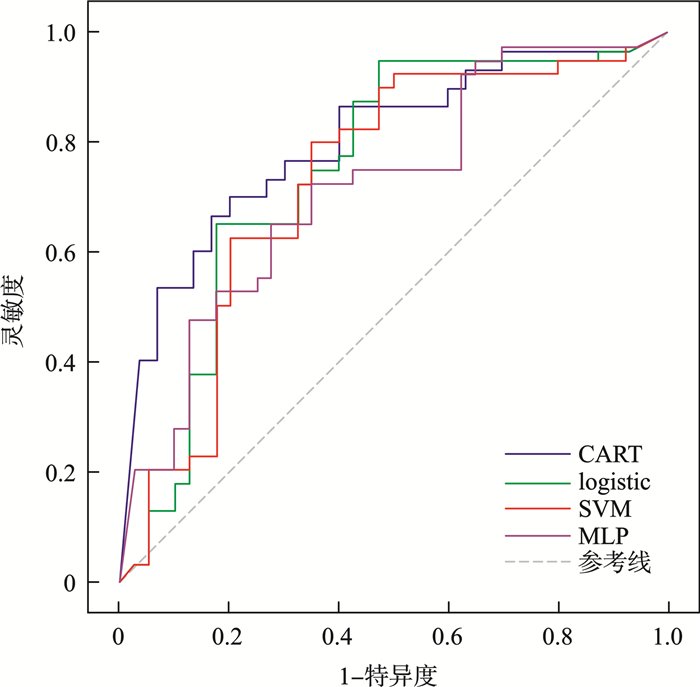
摘要: 目的 构建用于肺部感染导致的脓毒症患者短期预后预测机器学习模型。方法 本研究回顾性收集2020年1月-2024年6月因肺部感染并发脓毒症于西南医科大学附属医院住院治疗的患者192例,根据出院7 d内的临床结局分为存活组(128例)和死亡组(64例),收集患者入院24 h内的血常规及凝血功能结果,基于临床意义和相关研究,以及在初步建立模型时对预后预测的表现筛选出单核细胞率、中性粒细胞率、淋巴细胞率、红细胞体积分布宽度变异系数、红细胞体积分布宽度标准差、血小板数、活化部分凝血酶原时间、凝血酶时间、国际标准化比值、凝血酶原时间等10个相关变量作为预测变量,分别输入回归树节点模型(classification and regression tree,CART)、支持向量机(support vector machine,SVM)、logistic回归模型、多层感知机模型,通过准确率、精确率、召回率、F1-Score和采用受试者工作特征(ROC)曲线计算曲线下面积综合评估模型性能。结果 4个模型各有优势,其中CART模型的ROC曲线下面积为0.842,综合性能最佳;SVM模型的精确率最高,达到0.947;logistic回归模型的召回率及F1值分别为0.745、0.824。结论 基于机器学习构建的肺部感染导致的脓毒症患者短期预后预测模型具有较好的预测性能,为脓毒症患者预后评估提供了数据支持。Abstract: Objective To construct a machine learning model for short-term prognosis prediction of patients with sepsis caused by pulmonary infection.Methods This study used a retrospective case-control study method to collect 192 patients with pulmonary infection and sepsis admitted to the Affiliated Hospital of Southwest Medical University from January 2020 to June 2024, and divided them into survival group(128 cases) and death group(64 cases) based on their clinical outcomes within 7 days after discharge. The research collected the blood routine and coagulation function results within 24 hours after admission of the patients, and selected 10 predictive variables based on clinical significance, relevant studies, and their performance in preliminary model building, including monocyte rate, neutrophil rate, lymphocyte rate, red blood cell volume distribution width coefficient of variation, red blood cell volume distribution width standard deviation, platelet count, activated partial thromboplastin time, thrombin time, international normalized ratio, and prothrombin time. The predictive variables were input into the classification and regression tree(CART), support vector machine(SVM), logistic regression model, and Multilayer Perceptron models respectively, and the model performance was comprehensively evaluated by the accuracy rate, precision, recall rate, F1-Score, and the area under the receiver operating characteristic(ROC) curve.Results The four models had their own advantages, among which the ROC curve area of the CART model was 0.842, with the best overall performance; the precision of the SVM model was the highest, reaching 0.947. The recall rate and F1 value of the logistic regression model were 0.745 and 0.824 respectively.Conclusion The machine learning-based model for short-term prognosis prediction of patients with sepsis caused by pulmonary infection has good predictive performance, providing data support for the prognosis assessment of sepsis patients.
-
Key words:
- pulmonary infection /
- sepsis /
- machine learning /
- prognosis /
- prediction model
-

-
表 1 患者的基本资料比较
M(P25,P75),X±S 基本资料 存活组(128例) 死亡组(64例) χ2/Z/t P 性别/例(%) 2.685 0.101 男 64(50.0) 24(37.5) 女 64(50.0) 40(62.5) 年龄/岁 69.000(56.000,77.000) 72.000(61.000,80.000) -1.623 0.105 白细胞数/(×109/L) 10.660(7.550,15.950) 11.920(7.380,16.790) -0.601 0.549 中性粒细胞数/(×109/L) 8.720(6.150,14.250) 10.810(5.960,14.960) -0.704 0.482 淋巴细胞数/(×109/L) 0.920(0.530,1.300) 0.600(0.410,0.950) 2.948 0.003 单核细胞数/(×109/L) 0.460(0.320,0.770) 0.440(0.240,0.690) 1.273 0.204 嗜酸性粒细胞数/(×109/L) 0.020(0,0.080) 0.010(0,0.020) 2.208 0.020 嗜碱性粒细胞数/(×109/L) 0.020(0.010,0.030) 0.030(0.010,0.040) -1.909 0.053 中性粒细胞率/% 85.800(76.800,91.500) 90.300(82.300,94.200) -2.26 0.024 淋巴细胞率/% 7.200(4.300,13.200) 5.200(3.200,12.300) 2.149 0.032 单核细胞率/% 5.400(3.100,6.900) 3.500(2.000,6.100) 2.552 0.011 嗜酸性粒细胞率/% 0.100(0,0.700) 0.100(0,0.200) 1.831 0.055 嗜碱性粒细胞率/% 0.200(0.100,0.300) 0.200(0.200,0.400) -1.81 0.253 红细胞数/(×1012/L) 3.880(3.520,4.170) 3.770(2.910,4.270) 1.145 0.701 血红蛋白/(g/L) 112.305±22.099 110.719±28.743 0.385 0.931 红细胞压积 0.345±0.063 0.346±0.090 -0.087 0.024 红细胞平均体积/fl 91.100(87.300,94.700) 92.200(89.700,96.600) -2.26 0.329 红细胞平均血红蛋白量/pg 29.700(28.500,31.000) 30.100(29.000,31.100) -0.978 0.004 红细胞平均血红蛋白浓度/(g/L) 325.938±11.710 320.438±13.511 2.896 < 0.001 红细胞体积分布宽度标准差/fl 42.100(40.100,45.300) 45.100(42.300,50.100) -3.991 0.002 红细胞体积分布宽度变异系数/% 13.300(12.900,14.600) 14.100(13.300,15.400) -3.153 0.040 血小板数/(×109/L) 202.000(129.000,278.000) 174.000(88.000,236.000) 2.058 0.204 血小板平均体积/fl 9.700(8.900,10.600) 10.100(9.100,11.000) -1.271 0.131 血小板压积 0.190(0.140,0.260) 0.170(0.100,0.250) 2.043 0.153 血小板体积分布宽度/% 16.200(15.800,16.500) 16.300(16.000,16.500) -1.507 < 0.001 大血小板比例/% 25.300(19.600,31.500) 27.600(20.900,34.300) -1.431 < 0.001 表 2 凝血功能结果比较
M(P25,P75),X±S 实验室检查 存活组(128例) 死亡组(64例) χ2/Z/t P PT/s 13.000(12.100,14.000) 15.400(13.900,17.300) -6.171 < 0.001 国际标准化比值 1.090(1.030,1.160) 1.200(1.110,1.430) -5.423 < 0.001 凝血酶原时间比率 1.090(1.030,1.150) 1.170(1.100,1.340) -4.999 0.002 凝血酶原时间活动度/% 85.187±15.506 70.223±21.328 4.957 < 0.001 APTT/s 29.900(27.100,35.300) 35.000(28.800,41.500) -3.119 < 0.001 TT/s 16.500(15.500,17.200) 17.400(16.400,19.400) -4.225 < 0.001 纤维蛋白原/(g/L) 6.110(4.350,7.370) 4.660(3.000,6.150) 3.431 < 0.001 D二聚体/(μg/mL) 1.900(0.995,3.485) 5.450(2.190,11.730) -4.769 < 0.001 抗凝血活酶Ⅲ/s 78.814±15.335 67.369±20.545 3.914 0.131 纤维蛋白原降解产物/(μg/mL) 7.500(4.050,13.700) 23.790(8.360,57.700) -4.711 0.153 表 3 模型预测结果
模型名称 准确率 精确率 召回率 F1 AUC CART 0.714 0.816 0.738 0.775 0.842 SVM 0.730 0.947 0.706 0.809 0.742 logistic 0.762 0.921 0.745 0.824 0.766 MLP 0.667 0.868 0.673 0.758 0.729 -
[1] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[2] Fleischmann-Struzek C, Mellhammar L, Rose N, et al. Incidence and mortality of hospital-and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis[J]. Intensive Care Med, 2020, 46(8): 1552-1562. doi: 10.1007/s00134-020-06151-x
[3] Giamarellos-Bourboulis EJ, Aschenbrenner AC, Bauer M, et al. The pathophysiology of sepsis and precision-medicine-based immunotherapy[J]. Nat Immunol, 2024, 25: 19-28. doi: 10.1038/s41590-023-01660-5
[4] Chen H, Zhu Z, Zhao CY, et al. Central venous pressure measurement is associated with improved outcomes in septic patients: an analysis of the MIMIC-Ⅲ database[J]. Crit Care, 2020, 24(1): 433. doi: 10.1186/s13054-020-03109-9
[5] 曹钰, 柴艳芬, 邓颖, 等. 中国脓毒症/脓毒性休克急诊治疗指南(2018)[J]. 临床急诊杂志, 2018, 19(9): 567-588. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2018.09.001
[6] 张豹. 基于机器学习算法的数据分类与标准化方法研究[J]. 信息与电脑(理论版), 2024, 36(6): 53-55.
[7] 李萍. 机器学习在急诊医疗服务体系中的应用现状与展望[J]. 临床急诊杂志, 2020, 21(6): 507-511. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.06.018
[8] 夏义琴, 曹钰. 急诊科脓毒症的早期筛检与评估[J]. 华西医学, 2022, 37(11): 1607-1611.
[9] 朱晴, 张逸雪, 刘洋, 等. 脓毒症的病理生理机制研究进展[J]. 中华医院感染学杂志, 2022, 32(16): 2551-2555.
[10] 季孝, 吴跃波, 谢璐涛, 等. 基于logistic回归模型的血常规参数在脓毒症早期诊断的价值[J]. 中国卫生检验杂志, 2022, 32(16): 2001-2004, 2008.
[11] Iba T, Umemura Y, Wada H, et al. Roles of coagulation abnormalities and microthrombosis in sepsis: pathophysiology, diagnosis, and treatment[J]. Arch Med Res, 2021, 52(8): 788-797.
[12] Mohapatra P, Kumar A, Singh RK, et al. The effect of sepsis and septic shock on the viscoelastic properties of clot quality and mass using thromboelastometry: a prospective observational study[J]. Indian J Crit Care Med, 2023, 27(9): 625-634.
[13] 王艳, 曹志新, 于金辉, 等. ICU脓毒症患者凝血相关参数的变化与预后关系的研究[J]. 临床和实验医学杂志, 2022, 21(14): 1519-1523.
[14] Yu S, Ma Y, Li X. The correlation between coagulation function and prognosis in patients with acute respiratory distress syndrome caused by extrapulmonary sepsis or pulmonary infection[J]. 2021.
[15] Chen YW, Li YJ, Deng P, et al. Learning to predict in-hospital mortality risk in the intensive care unit with attention-based temporal convolution network[J]. BMC Anesthesiol, 2022, 22(1): 119.
[16] Taylor RA, Pare JR, Venkatesh AK, et al. Prediction of in-hospital mortality in emergency department patients with sepsis: a local big data-driven, machine learning approach[J]. Acad Emerg Med, 2016, 23(3): 269-278.
-

计量
- 文章访问数: 457
- 施引文献: 0



 下载:
下载: