Prognostic effect of ultra-early use of norepinephrine in elderly patients with infection and hypotension
-
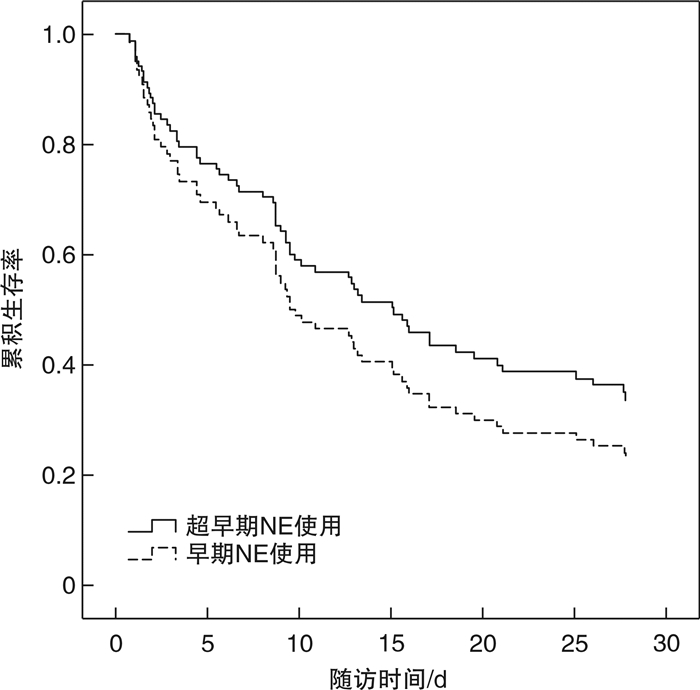
摘要: 目的 探讨去甲肾上腺素(norepinephrine,NE)超早期使用对感染伴低血压的老年患者的预后影响。方法 收集2020年1月—2023年1月ICU收治的感染伴低血压的老年患者,比较超早期(液体复苏的伊始)NE使用组与早期(开始液体复苏后0.5~1.0 h)NE使用组24 h乳酸清除率(lactic acid clearance,LCR)、24 h尿量的差异;以早期NE使用为参照,Cox比例风险分析超早期NE使用对28 d死亡率的影响。结果 超早期NE使用组与早期NE使用组LCR、尿量差异无统计学意义(P>0.05)。当LCR<3.5 mmol/L时,超早期NE使用组LCR升高(P<0.05),两组间尿量差异无统计学意义(P>0.05)。当LCR≥3.5 mmol/L时,超早期NE使用组尿量有增加趋势(P=0.05),两组间LCR差异无统计学意义(P>0.05)。对28 d死亡率的Cox比例风险分析,两组间差异无统计学意义(P>0.05)。结论 NE超早期使用对感染伴低血压的老年患者的预后无劣性影响。Abstract: Objective To investigate the effect of ultra-early use of norepinephrine(NE) on the prognosis of elderly patients with infection and hypotension.Methods Elderly patients with infection and hypotension admitted to ICU from January 2020 to January 2023 were collected, and the differences of 24 h lactic acid clearance(LCR) and 24 h urine volume were compared between the ultra-early(at the beginning of fluid resuscitation) NE group and the early(0.5-1.0 h after starting fluid resuscitation) NE group. Using early NE use as reference, Cox proportional risk analysis was conducted to analyze the effect of ultra-early NE use on 28-day mortality.Results There was no significant difference in LCR and urine volume between the ultra-early NE use group and the early NE use group. When LCR < 3.5 mmol/L, LCR was increased in the ultra-early NE use group(P < 0.05), and there was no significant difference in urine volume between the two groups. When LCR≥3.5 mmol/L, the urine volume of the ultra-early NE use group tended to increase(P=0.05), and there was no significant difference in LCR between the two groups. Cox proportional risk analysis of 28-day mortality showed no significant difference between the two groups.Conclusion The early use of NE has no adverse effect on the prognosis of infected elderly patients with hypotension.
-
Key words:
- infection /
- hypotension /
- elderly /
- norepinephrine
-

-
表 1 超早期NE使用组与早期NE使用组的基线资料比较
X±S 资料 超早期NE使用(28例) 早期NE使用(78例) t/χ2 P 性别/例(%) 1.363 >0.05 男 21(75.0) 49(62.8) 女 7(25.0) 29(37.2) 年龄/例(%) 75.63±6.32 79.96±7.20 -2.177 <0.05 高血压病/例(%) 8(28.6) 32(41.0) 1.360 >0.05 CCI/分 3.43±1.86 4.63±2.75 -1.870 >0.05 肺源性感染灶/例(%) 23(82.1) 62(79.5) 0.091 >0.05 SOFA/分 6.90±2.78 7.34±2.46 -1.459 >0.05 胆红素/(μmol/L) 13.10±9.22 18.21±17.43 -1.688 >0.05 肌酐/(μmol/L) 144.76±102.59 153.26±108.11 -0.320 >0.05 SI 1.39±0.31 1.38±0.43 0.115 >0.05 DSI 2.48±0.70 2.34±0.81 0.718 >0.05 MSI 1.96±0.49 1.90±0.63 0.386 >0.05 NEWS/分 12.45±2.56 13.38±3.10 -1.259 >0.05 Lac/(mmol/L) 3.51±2.71 5.83±4.79 -2.778 <0.05 NLR 17.89±12.36 19.82±15.44 -0.519 >0.05 PLR 246.92±153.25 308.14±248.37 -1.061 >0.05 PCT/(ng/mL) 9.66±13.24 12.85±19.21 -0.768 >0.05 表 2 超早期NE使用组与早期NE使用组的次要结局比较
X±S 项目 例数 超早期NE使用组 例数 早期NE使用组 P 总体 LCR/% 28 15.51±43.80 78 0.09±72.68 >0.05 尿量/mL 1 585.71±1 017.95 1 423.85±1 164.36 >0.05 Lac<3.5 mmol/L LCR/% 16 4.55±45.80 36 -43.79±79.47 <0.05 尿量/mL 1 608.33±1 180.18 2 033.04±1 222.97 >0.05 Lac≥3.5 mmol/L LCR/% 12 31.33±37.58 42 34.95±42.43 >0.05 尿量/mL 1 555.56±820.75 922.18±841.51 =0.05 表 3 28 d死亡组与幸存组的基线资料比较
X±S 资料 死亡组(78例) 幸存组(28例) t/χ2 P 男/例(%) 49(62.8) 21(75.0) 1.363 >0.05 年龄/岁 74.94±11.01 76.48±11.69 -0.546 >0.05 高血压病/例(%) 29(37.2) 11(39.3) 0.039 >0.05 CCI/分 4.42±2.64 4.09±2.52 0.507 >0.05 肺源性感染灶/例(%) 64(82.1) 21(75.0) 0.645 >0.05 SOFA/分 7.61±2.28 5.87±2.80 2.340 <0.05 胆红素/(μmol/L) 18.87±17.76 11.78±7.34 2.554 <0.05 肌酐/(μmol/L) 154.69±113.61 140.22±81.84 0.537 >0.05 SI 1.41±0.41 1.30±0.38 1.117 >0.05 DSI 2.40±0.78 2.29±0.81 0.545 >0.05 MSI 1.94±0.58 1.86±0.64 0.534 >0.05 NEWS/分 13.32±2.78 12.64±3.51 0.922 >0.05 Lac/(mmol/L) 5.66±4.58 4.02±3.92 1.499 >0.05 NLR 19.44±14.46 19.02±15.60 0.115 >0.05 PLR 281.85±223.63 322.59±245.34 -0.714 >0.05 PCT/(ng/mL) 12.31±19.59 10.81±12.09 0.281 >0.05 表 4 Cox比例风险多因素分析
因素 回归系数 标准误 Wald P OR SOFA 0.086 0.078 1.203 0.273 1.089 胆红素 0.007 0.008 0.746 0.388 1.007 超早期NE使用 -0.216 0.504 0.183 0.668 0.806 -
[1] 曹照龙. 老年社区获得性肺炎患者的诊疗策略[J]. 中华医学信息导报, 2020, 35(13): 1. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCW202108026.htm
[2] Cao JD, Wang ZC, Wang YL, et al. Risk factors for progression of Urolith Associated with Obstructive Urosepsis to severe sepsis or septic shock[J]. BMC Urol, 2022, 22(1): 46. doi: 10.1186/s12894-022-00988-8
[3] Edel A, Schaller SJ. Septic Shock and Vasopressor Initiation: Why Earlier is Better[J]. ICU Manag Pract, 2022, 22(2): 60-61.
[4] Carlos Sanchez E, Pinsky MR, Sinha S, et al. Fluids and Early Vasopressors in the Management of Septic Shock: Do We Have the Right Answers Yet?[J]. J Crit Care Med(Targu Mures), 2023, 9(3): 138-147. doi: 10.2478/jccm-2023-0022
[5] 刘岩, 高翔, 朱玉琴, 等. 早期动态监测肝素结合蛋白对老年脓毒症患者预后的预测价值[J]. 临床急诊杂志, 2023, 4(24): 173-184. doi: 10.13201/j.issn.1009-5918.2023.04.001
[6] Weng L, Xu Y, Yin P, et al. National incidence and mortality of hospitalized sepsis in China[J]. Crit Care, 2023, 27(1): 84. doi: 10.1186/s13054-023-04385-x
[7] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 中国脓毒症早期预防与阻断急诊专家共识[J]. 临床急诊杂志, 2020, 21(7): 517-529. doi: 10.13201/j.issn.1009-5918.2020.07.001
[8] Scheeren T, Bakker J, De Backer D, et al. Current use of vasopressors in septic shock[J]. Ann Intensive Care, 2019, 9(1): 20. doi: 10.1186/s13613-019-0498-7
[9] 杨光, 李小刚. 脓毒症休克的1 h集束化治疗的挑战[J]. 临床急诊杂志, 2019, 9(20): 676-678. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2019.09.003
[10] Shi R, Hamzaoui O, De Vita N, et al. Vasopressors in septic shock: which, when, and how much?[J]. Ann Transl Med, 2020, 8(12): 794. doi: 10.21037/atm.2020.04.24
[11] Elbouhy MA, Soliman M, Gaber A, et al. Early Use of Norepinephrine Improves Survival in Septic Shock: Earlier than Early[J]. Arch Med Res, 2019, 50(6): 325-332. doi: 10.1016/j.arcmed.2019.10.003
[12] Bakker J, Kattan E, Annane D, et al. Current practice and evolving concepts in septic shock resuscitation[J]. Intensive Care Med, 2022, 48(2): 148-163. doi: 10.1007/s00134-021-06595-9
[13] 中国医师协会急诊医师分会, 中华医学会急诊医学分会, 中国医疗保健国际交流促进会急诊分会. 血管加压药物在急诊休克中的应用专家共识[J]. 中华急诊医学杂志, 2021, 30(8): 929-936. https://www.cnki.com.cn/Article/CJFDTOTAL-SYYW202203010.htm
[14] 李国强, 孙亮. 脓毒性休克如何使用血管活性药物[J]. 中华结核和呼吸杂志, 2019, 42(9): 5.
[15] 李真玉, 齐颖, 陈兵. 脓毒性休克液体复苏策略的共识与争议[J]. 医学综述, 2022(12): 28. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZS202212022.htm
[16] Ospina-Tascón GA, Hernandez G, Alvarez I, et al. Effects of very early start of norepinephrine in patients with septic shock: a propensity score-based analysis[J]. Crit Care, 2020, 24(1): 52. doi: 10.1186/s13054-020-2756-3
[17] Waechter J, Kumar A, Lapinsky SE, et al. Interaction between fluids and vasoactive agents on mortality in septic shock: a multicenter, observational study[J]. Crit Care Med, 2014, 42(10): 2158-2168. doi: 10.1097/CCM.0000000000000520
[18] Ravi C, Johnson DW. Optimizing Fluid Resuscitation and Preventing Fluid Overload in Patients with Septic Shock[J]. Semin Respir Crit Care Med, 2021, 42(5): 698-705. doi: 10.1055/s-0041-1733898
[19] Shapiro NI, Douglas IS, Brower RG, et al. Early Restrictive or Liberal Fluid Management for Sepsis-Induced Hypotension[J]. N Engl J Med, 2023, 388(6): 499-510. doi: 10.1056/NEJMoa2212663
[20] Ryoo SM, Han KS, Ahn S, et al. The usefulness of C-reactive protein and procalcitonin to predict prognosis in septic shock patients: A multicenter prospective registry-based observational study[J]. Sci Rep, 2019, 9(1): 6579.
[21] 白郑海, 时雨, 王海, 等. 急诊脓毒症患者入院时肝功能特征分析[J]. 临床急诊杂志, 2018, 19(11): 771-774. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2018.11.011
[22] 修欣欣, 马利, 翟颖, 等. 降钙素原及APACHE-Ⅱ, SOFA评估复杂腹腔感染后脓毒性休克预后的价值[J]. 临床血液学杂志: 输血与检验, 2019, (4): 4. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ201908005.htm
[23] 梁欢, 苗常青, 吴梦茹, 等. 中性粒细胞与淋巴细胞比值对脓毒性休克患者28 d死亡风险的预测价值评估[J]. 临床急诊杂志, 2019, 20(7): 503-508. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2019.07.001
[24] Weinberger J, Klompas M, Rhee C. What Is the Utility of Measuring Lactate Levels in Patients with Sepsis and Septic Shock?[J]. Semin Respir Crit Care Med, 2021, 42(5): 650-661.
[25] Cardenas-Garcia J, Feller-Kopman D. Rebuttal From Drs Cardenas-Garcia and Feller-Kopman[J]. Chest, 2018, 153(2): 307-308.
-




 下载:
下载: