Microcirculation monitoring and management of sepsis: from a clinical practice perspective
-
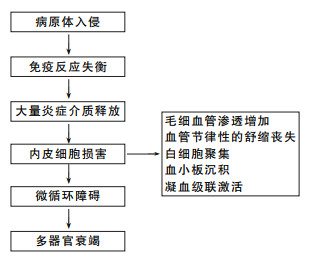
摘要: 脓毒症是重症监护治疗病房患者死亡的主要原因之一,多年来为解决这一难题研究人员提出了多种治疗方法,但脓毒症尤其是脓毒性休克患者的预后并未得到改善。随着对脓毒症研究的不断深入,发现微循环障碍是脓毒症导致多器官衰竭的关键,而脓毒症病死率与器官衰竭密切相关,因此在脓毒症治疗过程中微循环的监测和管理尤为重要。本文就临床实践中可用的微循环监测手段与管理方法进行综述,供应用参考。Abstract: Sepsis is one of the main causes of death in intensive care unit patients. Over the years, researchers have proposed a variety of treatment methods to solve this problem, but the prognosis of patients with sepsis, especially septic shock, has not improved. With the deepening of research on sepsis, it has been found that microcirculation disorder is the key to multiple organ failure caused by sepsis, and the mortality rate of sepsis is closely related to organ failure. Therefore, monitoring and management of microcirculation is particularly important in the course of sepsis treatment. This article reviews the microcirculation monitoring tools and management methods available in clinical practice for reference.
-
Key words:
- sepsis /
- microcirculation /
- capacity to monitor /
- bundle
-

-
表 1 微循环临床的监测
分类 名称 临床表现间接评估 中心静脉血氧饱和度或混合中心静脉血氧饱和度 动静脉二氧化碳分压差 血乳酸 皮肤情况 尿量 意识程度和精神状态 脑氧饱和度 可视化手段直接监测 手持式电子显微镜 激光多普勒成像 近红外光谱成像 以超声为基础评估 超声心动图 各器官多普勒超声 表 2 微循环的临床管理
方法或药物 作用 大循环复苏 保证足够的灌注压 乳酸水平管理 反映组织缺氧和功能障碍的重要标志 保障内皮细胞屏障功能 减少液体渗漏和组织液淤积,防止组织缺氧 微血管自律运动恢复 调控各个器官和组织的血流分布情况和灌注水平 早期使用抗生素 病因治疗 -
[1] Bauer M, Gerlach H, Vogelmann T, et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019-results from a systematic review and meta-analysis[J]. Crit Care, 2020, 24(1): 239. doi: 10.1186/s13054-020-02950-2
[2] Buchman TG, Simpson SQ, Sciarretta KL, et al. Sepsis Among Medicare Beneficiaries: 1. The Burdens of Sepsis, 2012-2018[J]. Crit Care Med, 2020, 48(3): 276-288. doi: 10.1097/CCM.0000000000004224
[3] Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study[J]. Lancet, 2020, 395(10219): 200-211. doi: 10.1016/S0140-6736(19)32989-7
[4] Dellinger RP, Levy MM, Schorr CA, et al. 50 Years of Sepsis Investigation/Enlightenment Among Adults-The Long and Winding Road[J]. Crit Care Med, 2021, 49(10): 1606-1625. doi: 10.1097/CCM.0000000000005203
[5] Peerapornratana S, Manrique-Caballero CL, Gómez H, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment[J]. Kidney Int, 2019, 96(5): 1083-1099. doi: 10.1016/j.kint.2019.05.026
[6] Igiebor O, Nakeshbandi M, Mehta N, et al. Impact of Sepsis Intervention Protocol(SIP)on Adherence to Three-hour and Six-hour Bundles and Mortality Outcomes in the Emergency Department[J]. Int J Clin Res Trials, 2020, 5(2): 280-284.
[7] Ko BS, Choi SH, Shin TG, et al. Impact of 1-Hour Bundle Achievement in Septic Shock[J]. J Clin Med, 2021, 10(3): 527. doi: 10.3390/jcm10030527
[8] 王仲, 魏捷, 朱华栋, 等. 中国脓毒症早期预防与阻断急诊专家共识[J]. 临床急诊杂志, 2020, 21(7): 517-529. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.07.001
[9] Yajnik V, Maarouf R. Sepsis and the microcirculation: the impact on outcomes[J]. Curr Opin Anaesthesiol, 2022, 35(2): 230-235. doi: 10.1097/ACO.0000000000001098
[10] Lupu F, Kinasewitz G, Dormer K. The role of endothelial shear stress on haemodynamics, inflammation, coagulation and glycocalyx during sepsis[J]. J Cell Mol Med, 2020, 24(21): 12258-12271. doi: 10.1111/jcmm.15895
[11] Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med, 2021, 47(11): 1181-1247. doi: 10.1007/s00134-021-06506-y
[12] Corradi F, Via G, Tavazzi G. What's new in ultrasound-based assessment of organ perfusion in the critically ill: expanding the bedside clinical monitoring window for hypoperfusion in shock[J]. Intensive Care Med, 2020, 46(4): 775-779. doi: 10.1007/s00134-019-05791-y
[13] 陈瑞, 王仲, 谢志毅. 毛细血管再充盈及其在急重症患者外周循环监测中的应用进展[J]. 中华急诊医学杂志, 2018, 27(9): 1062-1066. doi: 10.3760/cma.j.issn.1671-0282.2018.09.026
[14] Hariri G, Joffre J, Leblanc G, et al. Narrative review: clinical assessment of peripheral tissue perfusion in septic shock[J]. Ann Intensive Care, 2019, 9(1): 37. doi: 10.1186/s13613-019-0511-1
[15] 唐瑞明. ICU脓毒症休克皮肤花斑的研究进展[J]. 护理学, 2021, 10(6): 666-671.
[16] Hernández G, Ospina-Tascón GA, Damiani LP, et al. Effect of a Resuscitation Strategy Targeting Peripheral Perfusion Status vs Serum Lactate Levels on 28-Day Mortality Among Patients With Septic Shock: The ANDROMEDA-SHOCK Randomized Clinical Trial[J]. JAMA, 2019, 321(7): 654-664. doi: 10.1001/jama.2019.0071
[17] Pulido-Perez A, Bergon-Sendin M, Suarez-Fernandez R, et al. Skin and sepsis: contribution of dermatology to a rapid diagnosis[J]. Infection, 2021, 49(4): 617-629. doi: 10.1007/s15010-021-01608-7
[18] 刘强, 韩如泉. 脑氧饱和度监测方法及其应用进展[J]. 国际麻醉学与复苏杂志, 2018, 39(3): 234-238. doi: 10.3760/cma.j.issn.1673-4378.2018.03.009
[19] Dubin A, Kanoore EV, Caminos EJ, et al. Monitoring Microcirculation: Utility and Barriers-A Point-of-View Review[J]. Vasc Health Risk Manag, 2020, 16: 577-589. doi: 10.2147/VHRM.S242635
[20] Rovas A, Sackarnd J, Rossaint J, et al. Identification of novel sublingual parameters to analyze and diagnose microvascular dysfunction in sepsis: the NOSTRADAMUS study[J]. Crit Care, 2021, 25(1): 112. doi: 10.1186/s13054-021-03520-w
[21] Chen SH, Chan WS, Liu CM, et al. Effects of endotoxin adsorber hemoperfusion on sublingual microcirculation in patients with septic shock: a randomized controlled trial[J]. Ann Intensive Care, 2020, 10(1): 80. doi: 10.1186/s13613-020-00699-z
[22] 李文涛, 陈莹, 靳小静, 等. 肾阻力指数及生物标志物对脓毒症患者发生急性肾损伤的早期预测价值[J]. 临床急诊杂志, 2022, 23(3): 209-213. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.03.009
[23] Robba C, Goffi A, Geeraerts T, et al. Brain ultrasonography: methodology, basic and advanced principles and clinical applications. A narrative review[J]. Intensive Care Med, 2019, 45(7): 913-927. doi: 10.1007/s00134-019-05610-4
[24] Levy MM, Evans LE, Rhodes A. The Surviving Sepsis Campaign Bundle: 2018 update[J]. Intensive Care Med, 2018, 44(6): 925-928. doi: 10.1007/s00134-018-5085-0
[25] 吴淼, 杜贤进, 魏捷, 等. 华中地区79家医院急诊脓毒症诊治现状调查分析[J]. 临床急诊杂志, 2021, 22(4): 291-296. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2021.04.015
[26] Kamath S, Hammad AH, Abdo T. Management of Sepsis and Septic Shock: What Have We Learned in the Last Two Decades?[J]. Microorganisms, 2023, 11(9): 2231. doi: 10.3390/microorganisms11092231
[27] Potter EK, Hodgson L, Creagh-Brown B, et al. Manipulating the Microcirculation in Sepsis-the Impact of Vasoactive Medications on Microcirculatory Blood Flow: A Systematic Review[J]. Shock, 2019, 52(1): 5-12. doi: 10.1097/SHK.0000000000001239
[28] Wan F, Du X, Liu H, et al. Protective effect of anisodamine hydrobromide on lipopolysaccharide-induced acute kidney injury[J]. Biosci Rep, 2020, 40(7): SR20201812. doi: 10.1042/BSR20201812
[29] Iba T, Levy JH. Derangement of the endothelial glycocalyx in sepsis[J]. J Thromb Haemost, 2019, 17(2): 283-294. doi: 10.1111/jth.14371
[30] Du X, Liu H, Yue Y, et al. Anisodamine Hydrobromide Protects Glycocalyx and Against the Lipopolysaccharide-Induced Increases in Microvascular Endothelial Layer Permeability and Nitric Oxide Production[J]. Cardiovasc Eng Technol, 2021, 12(1): 91-100. doi: 10.1007/s13239-020-00486-8
[31] Li T, Ji X, Liu J, et al. Ulinastatin Improves Renal Microcirculation by Protecting Endothelial Cells and Inhibiting Autophagy in a Septic Rat Model[J]. Kidney Blood Press Res, 2022, 47(4): 256-269. doi: 10.1159/000521648
[32] Scholz SS, Borgstedt R, Ebeling N, et al. Mortality in septic patients treated with vitamin C: a systematic meta-analysis[J]. Crit Care, 2021, 25(1): 17. doi: 10.1186/s13054-020-03438-9
[33] Liu S, Zhao L, Liu Y. The Origin of Vasomotion and Stochastic Resonance in Vasomotion[J]. Front Bioeng Biotechnol, 2022, 10: 819716. doi: 10.3389/fbioe.2022.819716
[34] Im Y, Kang D, Ko RE, et al. Time-to-antibiotics and clinical outcomes in patients with sepsis and septic shock: a prospective nationwide multicenter cohort study[J]. Crit Care, 2022, 26(1): 19. doi: 10.1186/s13054-021-03883-0
-




 下载:
下载: