The evaluation value of Delta-like ligand 1 levels in risk stratification and prognosis of sepsis patients
-
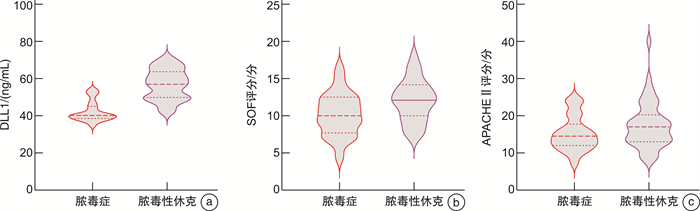
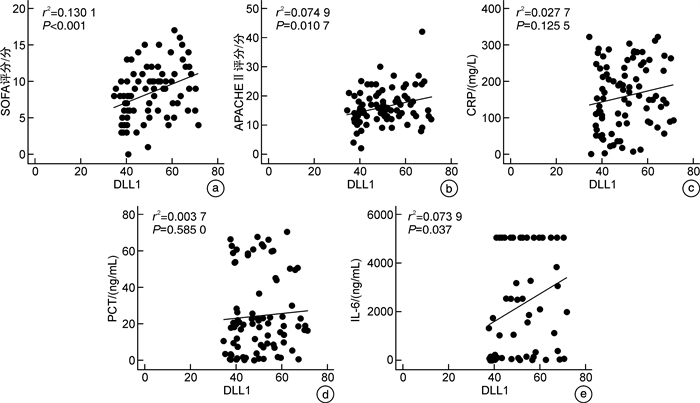
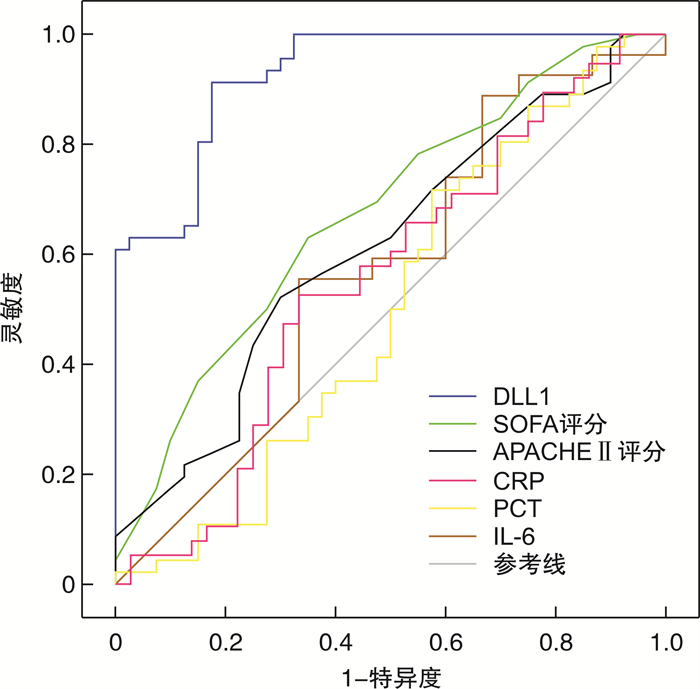
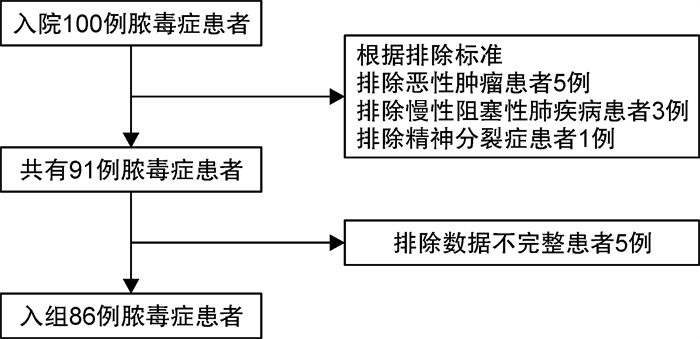
摘要: 目的 探讨血浆Delta样配体1(Delta-like ligand 1,DLL1)水平在判断脓毒症患者疾病严重程度及预后价值中的作用。方法 收集86例脓毒症患者的临床资料,根据入院后患者的病情严重程度分为脓毒症组40例和脓毒性休克组46例,根据28 d后患者的生存状况分为存活组53例和死亡组33例。比较各组基线资料、生化指标、序贯器官衰竭(sequential organ failure assessment,SOFA)评分、急性生理学及慢性健康状况评分系统Ⅱ(acute physiology and chronic health evaluation,APACHEⅡ)评分及血浆DLL1水平差异,分析DLL1与SOFA评分、APACHEⅡ评分、C反应蛋白、降钙素原、白介素6(IL-6)的相关性,ROC曲线分析其对疾病严重程度及预后的价值。结果 与脓毒症患者相比,脓毒性休克组患者血浆DLL1水平明显升高,差异有统计学意义(t=9.819,P < 0.001);死亡患者血浆DLL1水平较生存患者升高,差异有统计学意义(t=1.976,P=0.04);Pearson相关性分析显示,血浆DLL1水平与脓毒症患者SOFA评分、APACHE Ⅱ评分、IL-6呈显著性正相关(r2=0.130 1,P < 0.001;r2=0.074 9,P=0.010 7;r2=0.073 9,P=0.037 0);多因素分析显示DLL1是判断脓毒症病情严重程度的独立危险因素(OR=1.369,95%CI:1.151~1.628),ROC曲线显示血浆DLL1水平判断脓毒症严重程度的AUC为0.928(95%CI:0.877~0.979),cut-off值为47.105 ng/mL,灵敏度为0.913,特异度为0.825;DLL1高水平组死亡率显著高于DLL1低水平组,差异有统计学意义(P=0.002)。结论 DLL1在判断脓毒症病情严重程度及预后中有一定的评估价值。Abstract: Objective To explore the role of plasma Delta-like ligand 1(DLL1) levels in assessing the severity and prognostic value of sepsis in patients.Methods Clinical data of 86 patients with sepsis were collected and divided into sepsis group (n=40) and septic shock group (n=46) based on the severity of their condition after admission.According to the survival status of patients 28 days later, 86 patients were divided them into a survival group (n=53) and a death group (n=33). Baseline data, biochemical index, sequential organ failure assessment(SOFA) score, acute physiology and chronic health score system Ⅱ (APACHEⅡ) score, and plasma DLL1 levels were compared. The correlation between DLL1 and SOFA score, APACHEⅡ score, C-reactive protein (CRP), procalcitonin (PCT), interleukin-6 (IL-6) were analyzed, The ROC curve was used to analyze the value of disease severity and prognosis.Results Compared with sepsis patients, the plasma DLL1 levels in the septic shock group were significantly increased(t=9.819, P < 0.001), and the plasma DLL1 levels in deceased patients were higher than those in surviving patients(t=1.976, P=0.04). Pearson correlation analysis showed that plasma DLL1 levels were significantly positively correlated with SOFA score, APACHE Ⅱ score, and IL-6 in sepsis patients(r2=0.130 1, P < 0.001; r2=0.074 9, P=0.010 7; r2=0.073 9, P=0.037 0), Multivariate analysis showed that DLL1 was an independent risk factor for judging the severity of sepsis, with an OR of 1.369(95%CI: 1.151-1.628). The ROC curve showed that the AUC of plasma DLL1 level for judging the severity of sepsis was 0.928(95%CI: 0.877-0.979), with a cut-off value of 47.105 ng/mL, sensitivity of 0.913, and specificity of 0.825. The mortality of the DLL1 high-level group was significantly higher than that of the DLL1 low-level group, and the difference was statistically significant(P=0.002).Conclusion DLL1 has evaluative value in assessing the severity and prognosis of sepsis.
-
Key words:
- sepsis /
- Delta-like ligand 1 /
- the severity of the condition /
- prognosis
-

-
表 1 脓毒症与脓毒性休克患者的人口学特征
项目 脓毒症(40例) 脓毒性休克(46例) χ2/t/Z P 年龄/岁 59±15 62±14 -0.921 0.360 性别/例(%) 0.007 0.934 男 24(60.00) 28(60.87) 女 16(40.00) 18(39.13) 心率/(次/min) 115±27 110±24 0.759 0.450 呼吸频率/(次/min) 22(3.75) 23(4.00) -7.240 0.469 体温/℃ 37.7(1.8) 36.7(1.7) -2.828 0.005 白细胞计数/(×109/L) 12±8 14±10 -1.219 0.226 中性粒细胞计数(×109/L) 11±7 13±9 -0.906 0.367 淋巴细胞计数/(×109/L) 0.50(0.59) 0.46(0.41) -0.840 0.401 单核细胞计数/(×109/L) 0.23(0.43) 0.39(0.43) -0.195 0.846 CRP/(mg/L) 144±97 170±82 -1.347 0.182 PCT/(ng/mL) 19.19(48.29) 19.20(35.11) -0.476 0.634 IL-6/(ng/mL) 1 742±2 002 2 662±2 134 -1.808 0.077 感染部位数量 0.90±0.59 1.3±0.66 -2.869 0.004 使用白蛋白/例(%) 21(52.50) 31(67.39) 1.985 0.159 使用机械通气/例(%) 9(22.50) 26(56.52) 4.213 0.040 使用血液净化/例(%) 15(37.50) 18(39.13) 4.213 0.040 使用血管药物/例(%) 17(42.50) 40(86.96) 18.920 < 0.001 使用糖皮质激素/例(%) 14(35.00) 22(47.83) 1.446 0.229 合并症/例(%) 糖尿病 13(32.50) 17(36.96) 0.187 0.665 高血压 12(30.00) 21(45.65) 2.217 0.137 心血管疾病 7(17.50) 8(17.39) < 0.001 0.989 肾脏疾病 7(17.50) 11(23.91) 0.532 0.466 肝脏疾病 11(27.50) 8(17.39) 1.270 0.260 呼吸疾病 9(22.50) 14(30.43) 0.688 0.407 感染来源/例(%) 呼吸系统 21(52.50) 32(69.57) 2.635 0.105 腹腔 4(10.00) 17(37.00) 8.424 0.004 泌尿系系统 8(20.00) 5(10.87) 1.390 0.238 其他 7(17.50) 9(19.67) 0.243 0.809 表 2 脓毒症和脓毒性休克患者DLL1水平、SOFA评分、APACHEⅡ评分的比较
因素 脓毒症(40例) 脓毒性休克(46例) χ2/t P DLL1/(ng/mL) 42.27±5.43 56.81±8.20 -9.819 < 0.001 SOFA评分/分 7.23±3.45 9.43±3.42 -2.977 0.004 APACHEⅡ评分/分 14.85±5.31 17.48±6.37 -2.060 0.043 表 3 各指标判断脓毒症严重程度的多因素分析
影响因素 β SE Wald χ2 P OR 95%CI DLL1 0.314 0.088 12.581 < 0.001 1.369 1.151~1.628 SOFA评分 0.088 0.151 0.342 0.559 1.092 0.828~1.229 APACHEⅡ评分 0.009 0.101 0.007 0.931 1.009 0.828~1.229 CRP 0.005 0.006 0.587 0.440 1.005 0.992~1.018 PCT -0.052 0.029 3.108 0.078 0.950 0.887~1.006 IL-6 < 0.001 < 0.001 0.590 0.442 1.000 0.999~1.000 表 4 各指标对脓毒症患者发生脓毒性休克的预测价值
检测指标 AUC 标准误 P 95%CI 灵敏度 特异度 截断值 DLL1 0.928 0.026 < 0.001 0.877~0.979 0.913 0.825 47.105 ng/mL SOFA 0.674 0.058 0.006 0.561~0.788 0.630 0.650 8.500 APACHEⅡ 0.614 0.061 0.070 0.495~0.733 0.522 0.700 16.500 PCT 0.529 0.065 0.640 0.403~0.656 0.717 0.450 13.725 ng/mL CRP 0.530 0.064 0.634 0.405~0.605 0.043 0.850 60.690 ng/mL IL-6 0.536 0.080 0.655 0.380~0.693 0.457 0.750 2 767.000 ng/mL -
[1] 程方园, 吴晓英. 某三甲医院ICU护士对2016年脓毒症与脓毒性休克处理国际指南认知情况的调查分析[J]. 中西医结合心血管病电子杂志, 2019, 7(9): 192-193.
[2] 梁欢, 苗常青, 吴梦茹, 等. 中性粒细胞与淋巴细胞比值对脓毒性休克患者28 d死亡风险的预测价值评估[J]. 临床急诊杂志, 2019, 20(7): 503-508. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2019.07.001
[3] Rudd KE, Johnson SC, AGESA KM, et al. Global, regional, and national sepsis incidence and mortality, 1990—2017: analysis for the Global Burden of Disease Study[J]. Lancet, 2020, 395(10219): 200-211. doi: 10.1016/S0140-6736(19)32989-7
[4] 江伟, 杜斌. 中国脓毒症流行病学现状[J]. 医学研究生学报, 2019, 32(1): 5-8.
[5] 刘峰宇, 李想, 孙同文. 中国脓毒症十年研究回顾及展望[J]. 中华急诊医学杂志, 2023, 32(10): 1291-1295.
[6] 贾亚娟, 李潇风, 高志伟, 等. IL-37、PCT和CRP联合检测对急诊脓毒症患者28天预后的评估价值[J]. 临床急诊杂志, 2024, 25(9): 461-465, 471. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.09.003
[7] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 中国脓毒症早期预防与阻断急诊专家共识[J]. 临床急诊杂志, 2020, 21(7): 517-529. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.07.001
[8] 丁新焕, 彭耀军, 黄晶晶, 等. 急诊科脓毒症患者心脏骤停风险预测模型构建[J]. 中华急诊医学杂志, 2023, 32(12): 1693-1698.
[9] Hölle T, Rehn P, Leventogiannis K, et al. Evaluation of the Novel Sepsis Biomarker Host-Derived Delta-like Canonical Notch Ligand 1-A Secondary Analysis of 405 Patients Suffering from Inflammatory or Infectious Diseases[J]. Int J Mol Sci, 2023, 24(11): 9164. doi: 10.3390/ijms24119164
[10] Hildebrand D, Decker SO, Koch C, et al. Host-Derived Delta-Like Canonical Notch Ligand 1 as a Novel Diagnostic Biomarker for Bacterial Sepsis-Results From a Combinational Secondary Analysis[J]. Front Cell Infect Microbiol, 2019, 9: 267. doi: 10.3389/fcimb.2019.00267
[11] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[12] Liu D, Huang SY, Sun JH, et al. Sepsis-induced immunosuppression: mechanisms, diagnosis and current treatment options[J]. Mil Med Res, 2022, 9(1): 56.
[13] Ruangsomboon O, Panjaikaew P, Monsomboon A, et al. Diagnostic and prognostic utility of presepsin for sepsis in very elderly patients in the emergency department[J]. Clin Chim Acta, 2020, 510: 723-732. doi: 10.1016/j.cca.2020.09.014
[14] Pierrakos C, Velissaris D, Bisdorff M, et al. Biomarkers of sepsis: time for a reappraisal[J]. Crit Care, 2020, 24(1): 287. doi: 10.1186/s13054-020-02993-5
[15] Fox ED, Heffernan DS, Cioffi WG, et al. Neutrophils from critically ill septic patients mediate profound loss of endothelial barrier integrity[J]. Crit Care, 2013, 17(5): R226. doi: 10.1186/cc13049
[16] Zhou B, Lin W, Long Y, et al. Notch signaling pathway: architecture, disease, and therapeutics[J]. Signal Transduct Target Ther, 2022, 7(1): 95. doi: 10.1038/s41392-022-00934-y
[17] Gallenstein N, Tichy L, Weigand MA, et al. Notch Signaling in Acute Inflammation and Sepsis[J]. Int J Mol Sci, 2023, 24(4): 3458. doi: 10.3390/ijms24043458
[18] Bray SJ. Notch signalling in context[J]. Nat Rev Mol Cell Biol, 2016, 17(11): 722-735. doi: 10.1038/nrm.2016.94
[19] 杨小平, 李鑫鹏, 许哲敏, 等, Notch通路在脓毒症多脏器损伤中的研究进展[J]. 新疆医学, 2023, 53(10): 1260-1263.
[20] Moll M, Reichel K, Nurjadi D, et al. Notch Ligand Delta-Like 1 Is Associated With Loss of Vascular Endothelial Barrier Function[J]. Front Physiol, 2021, 12: 766713. doi: 10.3389/fphys.2021.766713
[21] Spyridaki A, Raftogiannis M, Antonopoulou A, et al. Effect of clarithromycin in inflammatory markers of patients with ventilator-associated pneumonia and sepsis caused by Gram-negative bacteria: results from a randomized clinical study[J]. Antimicrob Agents Chemother, 2012, 56(7): 3819-3825.
[22] Chen L, Lu H, Peng D, et al. Activation of NOTCH signaling via DLL1 is mediated by APE1-redox-dependent NF-kappaB activation in oesophageal adenocarcinoma[J]. Gut, 2023, 72(3): 421-432.
[23] O'Connor KW, Liu T, Kim S, et al. Bcl6, Irf2, and Notch2 promote nonclassical monocyte development[J]. Proc Natl Acad Sci U S A, 2023, 120(35): e2220853120.
[24] Gamrekelashvili J, Giagnorio R, Jussofie J, et al. Regulation of monocyte cell fate by blood vessels mediated by Notch signalling[J]. Nat Commun, 2016, 7: 12597.
-

计量
- 文章访问数: 194
- 施引文献: 0



 下载:
下载: