Predictive value of the prognostic nutritional index for 28-day ICU mortality in patients with septic shock
-
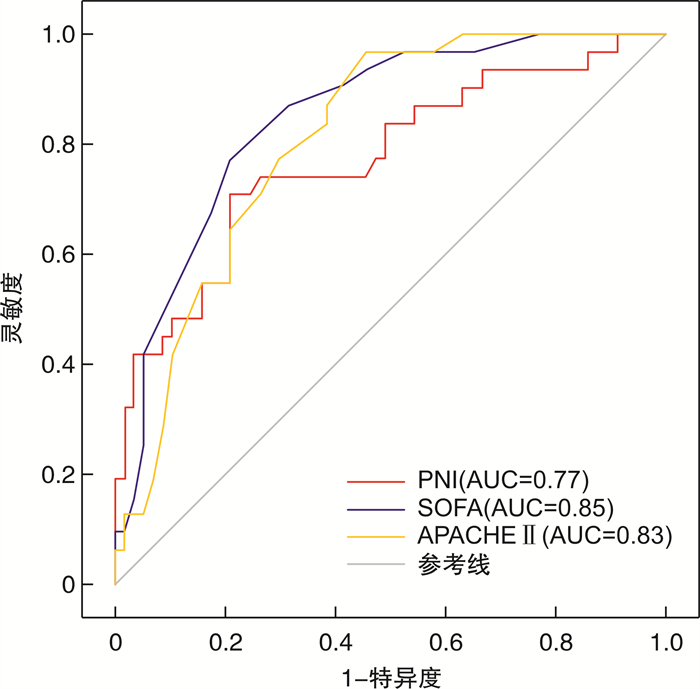
摘要: 目的 探讨预后营养指数(prognostic nutritional index,PNI)与脓毒症休克预后的相关性及其对脓毒症休克患者重症监护病房(intensive care unit,ICU)28 d死亡率的预测价值。方法 采用回顾性分析方法,分析安徽医科大学第二附属医院重症医学科2022年1月—2022年12月收治的脓毒症休克患者。根据患者在ICU入院28 d内的生存状况,将其分为生存组和死亡组,收集并分析相关临床和实验室资料。单因素和多因素logistic回归分析PNI与脓毒症休克预后的关系。受试者工作特征曲线(receiver operating characteristic,ROC)和曲线下面积(area under the curve,AUC)评价PNI对脓毒症休克患者ICU 28 d死亡率的预测价值,使用最大约登指数确定PNI截断值,根据截断值将患者分为两组,采用Kaplan-Meier法绘制生存曲线比较两组患者生存率。结果 共纳入88例脓毒症休克患者,生存组57例,死亡组31例,病死率为35.2%。死亡组的白蛋白、外周血淋巴细胞计数及PNI均低于生存组,差异有统计学意义(P < 0.05)。死亡组的尿素氮、乳酸、SOFA评分、APACHE Ⅱ评分及慢性肾脏病比例均高于生存组,差异有统计学意义(P < 0.05)。单因素和多因素logistic回归显示PNI与ICU 28 d死亡率独立相关(OR=0.84,95%CI:0.74~0.95,P < 0.01)。ROC分析显示PNI预测脓毒症休克患者ICU 28 d死亡率的AUC为0.77(95%CI:0.67~0.88,P < 0.01)。Kaplan-Meier生存曲线分析显示PNI>30.7组ICU 28 d生存率显著高于PNI ≤ 30.7组,差异有统计学意义(P < 0.01)。结论 PNI与脓毒症休克患者的预后存在独立相关性,且对脓毒症休克患者ICU 28 d死亡率有一定的预测价值。
-
关键词:
- 脓毒症休克 /
- 预后营养指数 /
- ICU 28 d死亡率 /
- 预测价值
Abstract: Objective To investigate the relationship between the prognostic nutritional index(PNI) and prognosis in septic shock, and its predictive value for 28-day intensive care unit(ICU) mortality in patients with septic shock.Methods A retrospective analysis was conducted on patients with septic shock admitted to the ICU of the Second Affiliated Hospital of Anhui Medical University from January to December 2022. Based on the survival status within 28 days after ICU admission, patients were divided into survival and death groups. Clinical and laboratory data were collected and analyzed. Univariate and multivariate logistic regression analyses were used to assess the association between PNI and prognosis in septic shock. The predictive value of PNI for 28-day ICU mortality in patients with septic shock was evaluated using the receiver operating characteristic(ROC) curve and area under the curve(AUC). The optimal PNI cut-off value was determined using the maximum Youden index, and patients were divided into two groups based on this threshold. The Kaplan-Meier method was used to plot survival curves and compare the survival rates between the two groups.Results A total of 88 patients with septic shock were included, with 57 cases in the survival group and 31 cases in the death group(35.2%). The death group had significantly lower peripheral blood lymphocyte count, albumin level, and PNI compared to the survival group(P < 0.05). In addition, blood urea nitrogen, lactate, SOFA scores, APACHE Ⅱ scores, and the proportion with chronic kidney disease were significantly higher in the death group(P < 0.05). Both univariate and multivariate logistic regression analyses showed that PNI was independently associated with 28-day ICU mortality(OR=0.84, 95%CI: 0.74-0.95, P < 0.01). ROC analysis revealed that PNI had an AUC of 0.77(95%CI: 0.67-0.88, P < 0.01) in predicting 28-day ICU mortality in patients with septic shock. Kaplan-Meier survival analysis indicated that the 28-day ICU survival rate was significantly higher in the group with PNI>30.7 compared with the group with PNI ≤ 30.7(P < 0.01).Conclusion PNI is independently associated with the prognosis of patients with septic shock and has a significant predictive value for 28-day ICU mortality.-
Key words:
- septic shock /
- prognostic nutritional index /
- 28-day ICU mortality /
- predictive value
-

-
表 1 两组患者临床资料比较
X±S,M(P25,P75) 变量 生存组(57例) 死亡组(31例) Z/t/χ2 P 年龄/岁 64.2±14.7 66.9±14.1 -0.84 0.40 性别/例(%) 0.04 0.83 女 23(40.4) 14(45.2) 男 34(59.6) 17(54.8) 白细胞计数/(×109/L) 14.5(8.1,25.3) 13.3(9.2,20.9) 0.97 0.34 血红蛋白/(g/L) 114.1±26.3 106.0±35.0 1.12 0.27 血小板计数/(×109/L) 165.3±100.0 143.1±96.8 1.02 0.31 淋巴细胞计数/(×109/L) 0.7(0.5,1.0) 0.5(0.2,0.9) 2.54 0.01 中性粒细胞计数/(×109/L) 13.2(6.5,23.8) 12.1(7.8,19.0) 0.92 0.36 白蛋白/(g/L) 31.0±5.0 26.7±5.1 3.80 < 0.01 总胆红素/(μmol/L) 18.5(12.4,33.1) 19.8(8.6,40.8) 0.14 0.89 肌酐/(μmol/L) 161(115,252) 190(127,374) -0.76 0.45 尿素氮/(mmol/L) 13.4(9.1,18.0) 22.4(15.9,29.8) -2.67 < 0.01 乳酸/(mmol/L) 2.8(1.8,4.8) 4.2(3.0,6.2) -2.46 0.01 高敏C反应蛋白/(mg/L) 197.2±122.9 200.0±124.6 -0.10 0.92 充血性心力衰竭/例(%) 12(21.1) 6(19.4) < 0.01 1.00 慢性肾脏病/例(%) 6(10.5) 11(35.5) 6.50 0.01 糖尿病/例(%) 21(36.8) 10(32.3) 0.04 0.84 高血压病/例(%) 19(33.3) 12(38.7) 0.07 0.79 脑卒中/例(%) 8(14.0) 7(22.6) 0.52 0.47 SOFA/分 9(7.0,12.0) 14(13.0,15.5) -5.39 < 0.01 APACHE Ⅱ/分 20.4±7.2 29.5±6.4 -6.04 < 0.01 PNI 35.4±5.9 29.7±5.7 4.40 < 0.01 表 2 多因素logistic回归分析结果
变量 SE OR 95%CI P PNI 0.07 0.84 0.74~0.95 < 0.01 SOFA 0.12 1.28 1.02~1.60 0.03 APACHEⅡ 0.06 1.16 1.03~1.32 0.02 乳酸 0.13 1.14 0.89~1.47 0.30 慢性肾脏病 0.84 2.31 0.44~12.02 0.32 表 3 ROC分析结果
变量 AUC 灵敏度/% 特异度/% 95%CI P PNI 0.77 71.0 78.9 0.67~0.88 < 0.01 SOFA 0.85 77.4 78.9 0.77~0.93 < 0.01 APACHE Ⅱ 0.83 96.8 54.4 0.75~0.92 < 0.01 白蛋白 0.74 61.3 82.3 0.62~0.85 < 0.01 外周血淋巴细胞计数 0.66 58.1 75.4 0.54~0.79 < 0.01 -
[1] Jarczak D, Kluge S, Nierhaus A. Sepsis-pathophysiology and therapeutic concepts[J]. Front Med, 2021, 8: 628302. doi: 10.3389/fmed.2021.628302
[2] Bauer M, Gerlach H, Vogelmann T, et al. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019-results from a systematic review and meta-analysis[J]. Crit Care, 2020, 24(1): 239. doi: 10.1186/s13054-020-02950-2
[3] Shao Y, Lai QC, Duan Q, et al. Nutritional indices at admission are associated with mortality rates of patients in the intensive care unit[J]. Eur J Clin Nutr, 2022, 76: 557-563. doi: 10.1038/s41430-021-00994-3
[4] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[5] Daud M, Ullah F, Uzair M, et al. Malnutrition and its influence on sepsis outcomes in elderly patients[J]. Cureus, 2024, 16(6): e63433.
[6] 林婷, 吕琦, 杨小玲, 等. 不同营养状态的老年住院患者医院感染特点[J]. 吉林医学, 2022, 43(11): 3026-3029.
[7] Liu Y, Zhao W, Chen WX, et al. Effects of early enteral nutrition on immune function and prognosis of patients with sepsis on mechanical ventilation[J]. J Intensive Care Med, 2020, 35(10): 1053-1061. doi: 10.1177/0885066618809893
[8] 朱铭钰, 朱静, 方兴超, 等. 预后营养指数与癌症预后的关联研究: 一项伞状评价[J]. 实用预防医学, 2023, 30(10): 1204-1210.
[9] Yuan K, Zhu SG, Wang HM, et al. Association between malnutrition and long-term mortality in older adults with ischemic stroke[J]. Clin Nutr, 2021, 40(5): 2535-2542. doi: 10.1016/j.clnu.2021.04.018
[10] Huang YK, Zhang QH, Li PF, et al. The prognostic nutritional index predicts all-cause mortality in critically ill patients with acute myocardial infarction[J]. BMC Cardiovasc Disord, 2023, 23(1): 339. doi: 10.1186/s12872-023-03350-4
[11] Akkuzu MZ, Altıntaş E, Yaraş S, et al. Controlling nutritional status (CONUT) score and prognostic nutritional index (PNI) are good candidates for prognostic markers for acute pancreatitis[J]. Medicina, 2022, 59(1): 70. doi: 10.3390/medicina59010070
[12] Wu H, Zhou CJ, Kong WQ, et al. Prognostic nutrition index is associated with the all-cause mortality in sepsis patients: a retrospective cohort study[J]. J Clin Lab Anal, 2022, 36(4): e24297. doi: 10.1002/jcla.24297
[13] Xie T, Xin Q, Chen R, et al. Clinical value of prognostic nutritional index and neutrophil-to-lymphocyte ratio in prediction of the development of sepsis-induced kidney injury[J]. Dis Markers, 2022, 2022: 1449758.
[14] Hu J, Lv CW, Hu XX, et al. Effect of hypoproteinemia on the mortality of sepsis patients in the ICU: a retrospective cohort study[J]. Sci Rep, 2021, 11: 24379. doi: 10.1038/s41598-021-03865-w
[15] Cao Y, Su YJ, Guo CR, et al. Albumin level is associated with short-term and long-term outcomes in sepsis patients admitted in the ICU: a large public database retrospective research[J]. Clin Epidemiol, 2023, 15: 263-273. doi: 10.2147/CLEP.S396247
[16] Cilloniz C, Peroni HJ, Gabarrús A, et al. Lymphopenia is associated with poor outcomes of patients with community-acquired pneumonia and sepsis[J]. Open Forum Infect Dis, 2021, 8(6): ofab169. doi: 10.1093/ofid/ofab169
[17] Hai PD, Viet Hoa LT. The prognostic accuracy evaluation of mNUTRIC, APACHEⅡ, SOFA, and SAPS 2 scores for mortality prediction in patients with sepsis[J]. Crit Care Res Pract, 2022, 2022: 4666594.
-

计量
- 文章访问数: 371
- 施引文献: 0



 下载:
下载:
