Clinical study of early qSOFA combined with serum indicators to predict infection source of sepsis
-
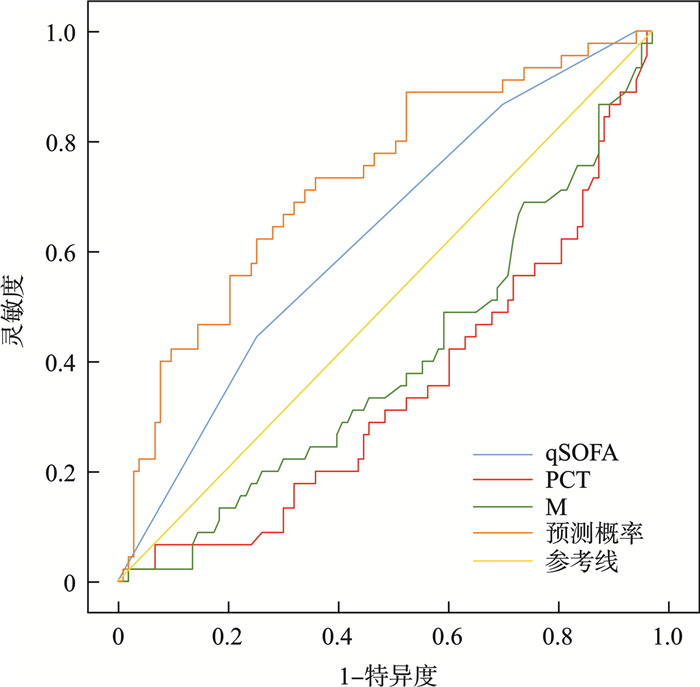
摘要: 目的 探讨快速序贯器官衰竭评分(quick sequential organ failure assessment,qSOFA)评分联合血清学指标预测脓毒症患者感染源的临床应用价值。方法 回顾性收集2022年1月—2023年12月收治的148例脓毒症患者的临床资料,根据感染源不同分为两组:肺部感染组(46例)和肺外感染组(102例),肺外感染组包括泌尿系统(32例),肠道(18例),腹膜炎(22例),肝胆系统(21例),其他(9例),肺外感染以腹腔内感染为主。统计两组入院时首次qSOFA评分和血清学指标,比较两组间qSOFA评分和血清学指标的差异,采用受试者工作特征(ROC)曲线分析各项指标及联合检测对感染源的预测价值。结果 肺部感染组和肺外感染组的qSOFA评分差异有统计学意义(P < 0.05),且qSOFA评分≥2是预测肺源性脓毒症的危险因素。在血清学指标中,两组患者的C-反应蛋白、白介素-6、中性粒细胞与淋巴细胞比率、血小板计数和D-二聚体的差异均无统计学意义(P>0.05),但降钙素原(procalcitonin,PCT)和单核细胞计数(monocyte count,MONO)的差异有统计学意义(P < 0.05)。肺部感染组和肺外感染组PCT的中位数分别是18.38(2.42,51.53) ng/mL和44.22(12.49,103.15) ng/mL,PCT明显升高是预测肺外脓毒症的危险因素;MONO的中位数分别是0.29(0.11,0.64)×109/L和0.50(0.22,0.87)×109/L,MONO明显降低是肺部感染的预测因素。ROC曲线分析结果显示,qSOFA评分、PCT、MONO及三项联合检测对肺部感染和肺外感染的评估概率曲线下面积依次为0.573(95%CI:0.476~0.671)、0.34(95%CI:0.244~0.436)、0.392(95%CI:0.292~0.491)、0.713(95%CI:0.622~0.803),单一指标中qSOFA评分预测价值最高,但所有单一指标AUC均低于联合预测。结论 早期qSOFA评分联合PCT和MONO对脓毒症患者感染源的预测有一定参考价值。
-
关键词:
- 脓毒症 /
- 感染源 /
- 快速序贯器官衰竭评分 /
- 降钙素原 /
- 单核细胞计数
Abstract: Objective To investigate the value of quick sequential organ failure assessment(qSOFA) combined with serum indicators in predicting the source of sepsis infection.Methods Clinical data of 148 patients with sepsis admitted from January 2022 to December 2023 were retrospectively collected and divided into two groups according to different sources of infection: pulmonary infection group(n=46) and extrapulmonary infection group(n=102). The extrapulmonary infection group include durinary system(n=32), intestinal tract(n=18), peritonitis(n=22), hepatobiliary system(n=21), and other(n=9), extrapulmonary infection was mainly intraperitoneal infection. The first qSOFA score and serological index of the two groups were counted, and the differences of qSOFA score and serum indicators between the two groups were discussed. The predictive value of each index and the combined detection on the source of infection was analyzed using receiver operating characteristic(ROC) curve.Results There was significant difference in qSOFA score between pulmonary infection group and extrapulmonary infection group(P < 0.05), and qSOFA score ≥2 was the predicted factor of pulmonary sepsis. There were no significant differences in C-reactive protein, interleukin-6, neutrophil to lymphocyte ratio, platelet and D-dimer among serological indexes(P>0.05), but there were significant differences in procalcitonin(PCT) and monocyte count(MONO)(P < 0.05). The median PCT of pulmonary infection group and extrapulmonary infection group were 18.38(2.42, 51.53) ng/mL and 44.22(12.49, 103.15) ng/mL, respectively. The significant increase of PCT was a related factor of extrapulmonary sepsis. The median values of MONO were 0.29(0.11, 0.64) ×109/L and 0.50(0.22, 0.87) ×109/L, respectively. MONO was significantly reduced as a factor associated with pulmonary infection. ROC curve analysis results showed that the area under the curve(AUC) of qSOFA score, PCT, MONO and the three combined tests for pulmonary infection and extrapulmonary infection were 0.573(95%CI: 0.476-0.671) and 0.34(95%CI: 0.244-0.436), 0.392(95%CI: 0.292-0.491), 0.713(95%CI: 0.622-0.803), respectively, qSOFA score had the highest predictive value among single indicators, but AUC of all single indicators was lower than that of combined prediction.Conclusion Early qSOFA score combined with PCT and MONO has a certain reference value for predicting the source of infection in sepsis patients. -

-
表 1 两组基本资料比较
项目 肺外感染组(102例) 肺部感染组(46例) χ2/t P 性别/例 3.202 0.074 男 55 32 女 47 14 年龄/岁 63.03±17.62 70.35±16.69 -2.376 0.019 慢性肾功不全/例 0.968 0.325 无 6 1 有 96 45 吸烟史/例 0.016 0.800 无 30 14 有 72 32 慢性阻塞性肺疾病或哮喘/例 9.868 0.002 无 5 10 有 97 36 糖尿病/例 0.141 0.707 无 41 20 有 61 26 高血压/例 1.385 0.238 无 32 19 有 70 27 冠心病/例 1.344 0.246 无 9 7 有 93 39 表 2 两组间qSOFA评分比较
分组 肺外感染/例 肺部感染/例 χ2 P qSOFA < 2分 29 6 4.157 0.041 qSOFA≥2分 73 40 表 3 两组间血清学指标比较
M(P25,P75),X±S 项目 肺外感染 肺部感染 t/Z P PCT/(ng/mL) 44.22(12.49,103.15) 18.38(2.42,51.53) -3.142 0.002 IL-6/(pg/mL) 708.86(185.60,3328.93) 455.88(160.07,5143.47) -0.416 0.677 D-D/(μg/mL) 5.22(2.97,10.27) 5.11(2.78,19.15) -0.061 0.952 MONO/(×109/L) 0.50(0.22,0.87) 0.29(0.11,0.64) -2.151 0.031 NLR 23.48(12.27,42.81) 17.92(6.94,30.66) -1.782 0.075 PLT/(×109/L) 142.50(75.75,221.75) 169.00(98.00,244.00) -1.388 0.165 CRP/(mg/L) 135.66±73.13 118.69±75.22 1.291 0.199 表 4 qSOFA、PCT、MONO在两组中的相关性
因素 B 标准误差 瓦尔德 显著性 Exp(B) 95%CI qSOFA 1.198 0.509 5.534 0.019 3.313 1.221~8.987 PCT -0.005 0.002 5.102 0.024 0.995 0.991~0.999 MONO -1.202 0.485 6.141 0.013 0.301 0.116~0.778 常量 -0.787 0.512 2.365 0.124 0.455 表 5 qSOFA联合血清学指标预测脓毒症感染源的AUC
检验结果变量 AUC区域 标准误差a 渐近显著性b 95%CI 灵敏度/% 特异度/% 约登指数 联合预测概率 0.713 0.046 < 0.001 0.622~0.803 73.30 63.00 0.363 PCT 0.340 0.049 0.001 0.244~0.436 100.00 1.00 0.010 MONO 0.392 0.051 0.032 0.292~0.491 2.20 98.00 0.002 qSOFA 0.573 0.050 0.140 0.476~0.671 44.40 74.00 0.184 -
[1] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[2] Huang M, Cai S, Su J. The pathogenesis of sepsis and potential therapeutic targets[J]. Int J Mol Sci, 2019, 20(21): E5376. doi: 10.3390/ijms20215376
[3] Ackerman MH, Ahrens T, Kelly J, et al. Sepsis[J]. Crit Care Nurs Clin North Am, 2021, 33(4): 407-418. doi: 10.1016/j.cnc.2021.08.003
[4] Pierrakos C, Velissaris D, Bisdorff M, et al. Biomarkers of sepsis: time for a reappraisal[J]. Crit Care, 2020, 24(1): 287. doi: 10.1186/s13054-020-02993-5
[5] Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the global burden of disease study[J]. Lancet, 2020, 395(10219): 200-211. doi: 10.1016/S0140-6736(19)32989-7
[6] 刘善收, 李琳, 代铮, 等. 脓毒症早期单核细胞减少与预后相关性的分析[J]. 现代医学, 2023, 51(7): 885-895. doi: 10.3969/j.issn.1671-7562.2023.07.002
[7] Liu B, Du HM, Zhang J, et al. Developing a new sepsis screening tool based on lymphocyte count, international normalized ratio and procalcitonin(LIP score)[J]. Sci Rep, 2022, 12(1): 20002. doi: 10.1038/s41598-022-16744-9
[8] Tusgul S, Carron PN, Yersin B, et al. Low sensitivity of qSOFA, SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage[J]. Scand J Trauma Resusc Emerg Med, 2017, 25(1): 108. doi: 10.1186/s13049-017-0449-y
[9] Siddiqui S, Chua M, Kumaresh V, et al. A comparison of pre ICU admission SIRS, EWS and q SOFA scores for predicting mortality and length of stay in ICU[J]. J Crit Care, 2017, 41: 191-193. doi: 10.1016/j.jcrc.2017.05.017
[10] Peake SL, Delaney A, Bailey M, et al. Potential impact of the 2016 consensus definitions of sepsis and septic shock on future sepsis research[J]. Ann Emerg Med, 2017, 70(4): 553-561. e1. doi: 10.1016/j.annemergmed.2017.04.007
[11] 张健峰, 顾晓蕾, 李斌, 等. 血乳酸联合qSOFA评分对早期筛选诊断脓毒症患者的价值[J]. 临床急诊杂志, 2021, 22(5): 344-347. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2021.05.011
[12] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 中国脓毒症早期预防与阻断急诊专家共识[J]. 临床急诊杂志, 2020, 21(7): 517-529. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.07.001
[13] Li SH, Rong HM, Guo QL, et al. Serum procalcitonin levels distinguish Gram-negative bacterial sepsis from Gram-positive bacterial and fungal sepsis[J]. J Res Med Sci, 2016, 21: 39. doi: 10.4103/1735-1995.183996
[14] Cnota W, Mucha D, Mucha J. The usefulness of determination of the procalcitonin (PCT) concentration in GBS piositive pregnant womens blood serum for anticipations of infections in newborns[J]. Przegl Epidemiol, 2018, 72(1): 25-32.
[15] Vallés PG, Gil Lorenzo AF, Garcia RD, et al. Toll-like receptor 4 in acute kidney injury[J]. Int J Mol Sci, 2023, 24(2): 1415. doi: 10.3390/ijms24021415
[16] 陈国昇, 文大林, 种慧敏, 等. 外周血单核细胞亚群及CD64表达水平对脓毒症诊断和预后评估的价值[J]. 中华危重病急救医学, 2022, 34(9): 921-926. doi: 10.3760/cma.j.cn121430-20220711-00647
[17] Chung H, Lee JH, Jo YH, et al. Circulating monocyte counts and its impact on outcomes in patients with severe sepsis including septic shock[J]. Shock, 2019, 51(4): 423-429. doi: 10.1097/SHK.0000000000001193
[18] Chiu C, Legrand M. Epidemiology of sepsis and septic shock[J]. Curr Opin Anaesthesiol, 2021, 34(2): 71-76. doi: 10.1097/ACO.0000000000000958
[19] 汪颖, 王迪芬, 付江泉, 等. SOFA、qSOFA评分和传统指标对脓毒症预后的判断价值[J]. 中华危重病急救医学, 2017, 29(8): 700-704. doi: 10.3760/cma.j.issn.2095-4352.2017.08.006
[20] 唐高骏, 何依婷, 简立建. 全身性感染新定义: 有助于ICU外的医护人员快速筛选出脓毒症患者[J]. 中华重症医学电子杂志(网络版), 2016, 2(3): 175-179.
[21] 戴佳文, 吴健, 顾彬, 等. TCC清单与qSOFA评分对严重创伤合并脓毒症的早期诊治价值[J]. 中华急诊医学杂志, 2019, 28(2): 185-189.
-

计量
- 文章访问数: 94
- 施引文献: 0



 下载:
下载: