Clinical value of sublingual microcirculation index, APACHEⅡ, NGAL and PCT for predicting sepsis-associated acute kidney injury
-
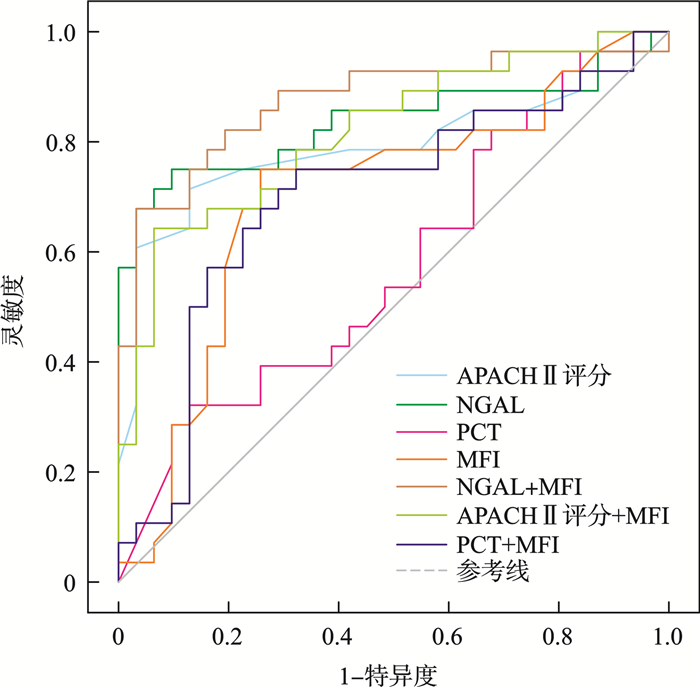
摘要: 目的 探讨舌下微循环[微血管流动指数(microvascular flow index, MFI)]、急性生理学与慢性健康状况评分Ⅱ(acute physiological and chronic health evaluation Ⅱ,APACHEⅡ)、中性粒细胞明胶酶相关脂钙蛋白(neutrophil gelatinase-associated lipocalin,NGAL)和降钙素原(procalcitonin,PCT)对预测脓毒症相关性急性肾损伤(sepsis-associated acute kidney injury,SA-AKI)的临床价值。方法 本研究采用单中心前瞻性纵向观察研究,纳入2023年10月-2024年6月在川北医学院附属医院重症监护病房住院的60例脓毒症患者。根据是否发展为继发性急性肾损伤(acute kidney injury,AKI)分为非AKI组(31例)和AKI组(29例)。收集患者一般资料(年龄、性别、体重指数、基础疾病)、在ICU入院的前24 h实验室检查结果、APACHEⅡ评分、舌下微循环参数。采用logistic分析SA-AKI的危险因素,进一步利用受试者工作特征曲线(ROC)进行深入分析各指标对SA-AKI的发生预测价值。结果 ①AKI组APACHE Ⅱ评分、白介素-6、D-二聚体、NGAL显著高于非AKI组(P < 0.05)。在AKI组中,MFI的数值显著低于非AKI组,差异有统计学意义(P < 0.05)。②NGAL(OR=0.003,95%CI:1.003~1.103)和APACHE Ⅱ(OR=0.012,95%CI:1.055~1.545)是识别SA-AKI的独立危险因素。③ROC曲线分析显示,PCT、NGAL、APACHEⅡ评分、MFI与SA-AKI发生具有相关性,曲线下面积(AUC)分别为0.574(95%CI:0.427~0.722)、0.836(95%CI:0.722~0.951)、0.798(95%CI:0.675~0.921)、0.702(95%CI:0.562~0.841)。上述指标分别与MFI联合检测AUC分别为0.700(95%CI:0.561~0.84)、0.876(95%CI:0.78~0.971)、0.817(95%CI:0.708~0.927)。结论 NGAL、APACHEⅡ评分、MFI与SA-AKI发生具有相关性,联合检测NGAL和MFI与SA-AKI相关性最好,对SA-AKI发生有一定预测价值。
-
关键词:
- 脓毒症 /
- 舌下微循环 /
- 急性肾损伤 /
- 中性粒细胞明胶酶相关脂钙蛋白
Abstract: Objective To investigate the clinical value of the sublingual microcirculation index(microvascular flow index, MFI), acute physiological and chronic health evaluation Ⅱ(APACHE Ⅱ) score, neutrophil gelatinase-associated lipocalin(NGAL), and procalcitonin(PCT) in the early identification of sepsis-associated acute kidney injury(SA-AKI).Methods A single-center, prospective, longitudinal observational study was conducted, involving sepsis patients admitted to the Critical Care Units of the Hospital Affiliated with North Sichuan Medical College between October 2023 and June 2024. Patients were categorized into two groups: non-AKI group(n=31) and AKI group(n=29), based on the development of secondary AKI. Demographic data(including age, sex, body mass index and fundamental diseases), laboratory tests, and the APACHE Ⅱ score were collected within the first 24 hours of admission. Logistic regression analysis was conducted to identify the risk factors for SA-AKI, and the predictive value of indicators was further evaluated using receiver operating characteristic(ROC) curves.Results ① Interleukin-6, D-dimer, NGAL, and APACHE Ⅱ score were higher in the AKI group compared to the non-AKI group(P < 0.05). The MFI in the AKI group was significantly lower than that in the non-AKI group(P < 0.05). ②NGAL(OR=0.003, 95%CI: 1.003-1.103) and APACHE Ⅱ(OR=0.012, 95%CI: 1.055-1.545) were identified as independent risk predictors for SA-AKI. ③ROC curve analysis suggested that PCT, NGAL, APACHE Ⅱ score and MFI had predictive value for sepsis-associated acute kidney injury, with AUCs of 0.574(95%CI: 0.427-0.722), 0.836(95%CI: 0.722-0.951), 0.798(95%CI: 0.675-0.921), and 0.702(95%CI: 0.562-0.841), respectively. Additionally, combined detection of the above indicators (PCT, NGAL and APACHE Ⅱscore) and MFI yielded AUCs were 0.700(95%CI: 0.561-0.840), 0.876(95%CI: 0.780-0.971), and 0.817(95%CI: 0.708-0.927).Conclusion NGAL, APACHE Ⅱscore and MFI exhibit a significant correlation in the context of SA-AKI, and the combined detection of NGAL and MFI holds predictive value for the development of SA-AKI. -

-
表 1 各组患者的一般资料
M(P25,P75) 项目 非AKI组(31例) AKI组(29例) t/z/χ2 P 年龄/岁 73.00(69.00,78.50) 73.00(69.00,78.00) -0.141 0.888 BMI/(kg/m2) 21.23(19.71,22.91) 22.04(20.60,24.21) -1.490 0.136 性别/例(%) 0.100 0.752 男 18(58.06) 18(62.07) 女 13(41.94) 11(37.93) 基础疾病/例(%) 冠心病 1.541 0.214 无 29(93.55) 23(79.31) 有 2(6.45) 6(20.69) 高血压 1.045 0.307 无 24(77.42) 19(65.52) 有 7(22.58) 10(34.48) 糖尿病 0.184 0.668 无 22(70.97) 22(75.86) 有 9(29.03) 7(24.14) 慢性阻塞性肺疾病 0.267 0.605 无 29(93.55) 25(86.21) 有 2(6.45) 4(13.79) 表 2 实验室检查结果
M(P25,P75),X±S 项目 非AKI组(31例) AKI组(29例) t/z/χ2 P IL-6/(pg/mL) 76.64(21.25,682.15) 703.00(131.66,1617.25) -2.280 0.023 D-D/(μg/mL) 2.90(1.65,15.05) 15.92(4.65,31.50) -2.934 0.003 PCT/(ng/mL) 4.45(0.61,12.25) 10.22(2.07,50.00) -1.743 0.081 NGAL/(ng/mL) 145.70(103.25,207.70) 605.00(283.70,836.50) -4.797 < 0.001 Scr/(mmol/L) 62.30(51.80,78.20) 72.10(56.30,88.50) 1.698 0.071 APACHEⅡ评分/分 20.03±5.59 26.50±6.37 -4.151 < 0.001 表 3 舌下微循环检查参数
M(P25,P75),X±S 项目 非AKI组(31例) AKI组(29例) t/z/χ2 P TVD/(mm/mm2) 16.81(15.99,17.88) 16.77(16.14,17.21) -0.259 0.796 PVD /(mm/mm2) 15.37±1.88 15.24±1.38 0.306 0.761 PPV/% 83.72±5.82 84.76±4.80 -0.753 0.454 MFI/au 2.53±0.19 2.39±0.19 2.760 0.008 HI/au 0.18(0.15,0.22) 0.17(0.14,0.21) -0.972 0.331 表 4 单因素logistic回归分析
因素 β SE P OR 95%CI 年龄 -0.014 0.024 0.542 0.986 0.941~1.032 BMI 0.180 0.105 0.087 1.197 0.975~1.469 性别 0.167 0.528 0.752 1.182 0.420~3.327 是否有冠心病 1.330 0.863 0.123 3.783 0.697~20.526 是否高血压 0.590 0.581 0.309 1.805 0.578~5.631 是否糖尿病 -0.251 0.587 0.669 0.778 0.246~2.459 是否慢性阻塞性肺疾病 0.842 0.908 0.354 2.320 0.391~13.753 IL-6 0 0 0.245 1.000 1.000~1.001 D-D 0.014 0.011 0.228 1.014 0.992~1.036 PCT 0.032 0.015 0.036 1.032 1.002~1.063 NGAL 0.007 0.002 <.001 1.007 1.003~1.011 Scr 0.024 0.015 0.098 1.025 0.996~1.054 APACHE Ⅱ评分 0.207 0.065 0.001 1.231 1.083~1.398 TVD -0.046 0.173 0.789 0.955 0.680~1.340 PVD -0.049 0.159 0.756 0.952 0.697~1.299 PPV 0.038 0.050 0.448 1.038 0.942~1.144 MFI -3.741 1.483 0.012 0.024 0.001~0.434 HI -2.661 4.690 0.570 0.070 0~685.747 表 5 多因素logistic回归分析
因素 β SE P OR 95%CI PCT -0.015 0.028 0.588 0.985 0.932~1.041 NGAL 0.008 0.003 0.003 1.008 1.003~1.013 APACHE Ⅱ评分 0.244 0.097 0.012 1.277 1.055~1.545 MFI -3.080 2.119 0.146 0.046 0.001~2.924 表 6 PCT、NGAL、APACHEⅡ评分、MFI对SA-AKI的预测价值
因素 AUC 截断点 灵敏度/% 特异度/% P 95%CI PCT 0.574 24.00 ng/mL 31.03 87.10 0.328 0.427~0.722 NGAL 0.836 267.09 ng/mL 75.86 90.32 < 0.001 0.722~0.951 APACHE Ⅱ评分 0.798 24.00分 71.43 87.10 < 0.001 0.675~0.921 MFI 0.702 2.49 au 75.86 74.19 0.008 0.562~0.841 PCT+MFI 0.700 0.43 75.86 67.74 0.008 0.561~0.840 NGAL+MFI 0.876 0.49 68.97 96.77 < 0.001 0.780~0.971 APACHEⅡ+MFI 0.817 0.59 64.29 93.55 < 0.001 0.708~0.927 -
[1] Zarbock A, Koyner JL, Gomez H, et al. Sepsis-associated acute kidney injury-treatment standard[J]. Nephrol Dial Transplant, 2023, 39(1): 26-35. doi: 10.1093/ndt/gfad142
[2] Neyra JA, Ortiz-Soriano V, Liu LJ, et al. Prediction of mortality and major adverse kidney events in critically ill patients with acute kidney injury[J]. Am J Kidney Dis, 2023, 81(1): 36-47. doi: 10.1053/j.ajkd.2022.06.004
[3] White KC, Serpa-Neto A, Hurford R, et al. Sepsis-associated acute kidney injury in the intensive care unit: incidence, patient characteristics, timing, trajectory, treatment, and associated outcomes. A multicenter, observational study[J]. Intensive Care Med, 2023, 49(9): 1079-1089. doi: 10.1007/s00134-023-07138-0
[4] Balkrishna A, Sinha S, Kumar A, et al. Sepsis-mediated renal dysfunction: pathophysiology, biomarkers and role of phytoconstituents in its management[J]. Biomed Pharmacother, 2023, 165: 115183. doi: 10.1016/j.biopha.2023.115183
[5] Zhou HS, Liu LP, Zhao QY, et al. Machine learning for the prediction of all-cause mortality in patients with sepsis-associated acute kidney injury during hospitalization[J]. Front Immunol, 2023, 14: 1140755. doi: 10.3389/fimmu.2023.1140755
[6] Pais T, Jorge S, Lopes JA. Acute kidney injury in sepsis[J]. Int J Mol Sci, 2024, 25(11): 5924. doi: 10.3390/ijms25115924
[7] Huang WP, Xiang H, Hu C, et al. Association of sublingual microcirculation parameters and capillary refill time in the early phase of ICU admission[J]. Crit Care Med, 2023, 51(7): 913-923. doi: 10.1097/CCM.0000000000005851
[8] Kuwabara S, Goggins E, Okusa MD. The pathophysiology of sepsis-associated AKI[J]. Clin J Am Soc Nephrol, 2022, 17(7): 1050-1069. doi: 10.2215/CJN.00850122
[9] Duranteau J, De Backer D, Donadello K, et al. The future of intensive care: the study of the microcirculation will help to guide our therapies[J]. Crit Care, 2023, 27(1): 190. doi: 10.1186/s13054-023-04474-x
[10] Lu Y, Yang J, Li P, et al. Sublingual microcirculation and internal environment changes as early indications of sepsis: a prospective observational study[J]. Microcirculation, 2023, 30(4): e12801. doi: 10.1111/micc.12801
[11] 杨敬辉, 贾凌, 赵炜, 等. 舌下微循环对老年重症肺炎机械通气患者预后的评价[J]. 中国呼吸与危重监护杂志, 2023, 22(1): 18-23.
[12] Damiani E, Carsetti A, Casarotta E, et al. Microcirculation-guided resuscitation in sepsis: the next frontier?[J]. Front Med, 2023, 10: 1212321. doi: 10.3389/fmed.2023.1212321
[13] Poston JT, Koyner JL. Sepsis associated acute kidney injury[J]. BMJ, 2019, 364: k4891.
[14] Husain-Syed F, Reis T, Kashani K, et al. Advances in laboratory detection of acute kidney injury[J]. Pract Lab Med, 2022, 31: e00283. doi: 10.1016/j.plabm.2022.e00283
[15] Romejko K, Markowska M, Niemczyk S. The review of current knowledge on neutrophil gelatinase-associated lipocalin(NGAL)[J]. Int J Mol Sci, 2023, 24(13): 10470. doi: 10.3390/ijms241310470
[16] Stanski NL, Rodrigues CE, Strader M, et al. Precision management of acute kidney injury in the intensive care unit: current state of the art[J]. Intensive Care Med, 2023, 49(9): 1049-1061. doi: 10.1007/s00134-023-07171-z
[17] Wang QQ, Yang JL, Guo ZG, et al. The predictive role of neutrophil gelatinase-associated lipocalin in coronary artery disease[J]. Am J Med Sci, 2024, 368(5): 424-431. doi: 10.1016/j.amjms.2024.06.015
[18] Petrova I, Alexandrov A, Vladimirov G, et al. NGAL as biomarker of clinical and subclinical damage of kidney function after coronary angiography[J]. Diagnostics, 2023, 13(6): 1180. doi: 10.3390/diagnostics13061180
[19] Sun QL, Kang ZJ, Li ZH, et al. Urinary NGAL, IGFBP-7, and TIMP-2: novel biomarkers to predict contrast medium-induced acute kidney injury in children[J]. Ren Fail, 2022, 44(1): 1201-1206.
[20] Zaitoun T, Megahed M, Elghoneimy H, et al. Renal arterial resistive index versus novel biomarkers for the early prediction of sepsis-associated acute kidney injury[J]. Intern Emerg Med, 2024, 19(4): 971-981. doi: 10.1007/s11739-024-03558-y
[21] Kan WC, Huang YT, Wu VC, et al. Predictive ability of procalcitonin for acute kidney injury: a narrative review focusing on the interference of infection[J]. Int J Mol Sci, 2021, 22(13): 6903. doi: 10.3390/ijms22136903
[22] Fu G, Zhan HC, Li HL, et al. Association between procalcitonin and acute kidney injury in patients with bacterial septic shock[J]. Blood Purif, 2021, 50(6): 790-799. doi: 10.1159/000512351
[23] Xin Q, Xie TH, Chen R, et al. Construction and validation of an early warning model for predicting the acute kidney injury in elderly patients with sepsis[J]. Aging Clin Exp Res, 2022, 34(12): 2993-3004. doi: 10.1007/s40520-022-02236-3
[24] García AF, Manzano-Nunez R, Bayona JG, et al. Acute kidney injury in severely injured patients admitted to the intensive care unit[J]. Mil Med Res, 2020, 7(1): 47.
[25] Shen YZ, Yu JY, Zhou F, et al. The predictive performance of the lactate clearance rate combined with the APACHE Ⅱ score in the prediction of sepsis-associated acute kidney injury in 7 days[J]. Transl Androl Urol, 2022, 11(4): 543-553. doi: 10.21037/tau-22-225
[26] 何力, 苏连久, 张婧, 等. ICU内脓毒性休克急性肾损伤患者肾功能恢复的影响因素分析[J]. 中华危重病急救医学, 2020, 32(2): 199-203.
[27] Bruno RR, Hernandez G, Thiele H, et al. A microcirculation-guided trial: never trying is worse than failing[J]. Intensive Care Med, 2023, 49(12): 1555-1556. doi: 10.1007/s00134-023-07245-y
[28] Homes RAP, Giddens F, Francis RS, et al. The sublingual microcirculation and frailty index in chronic kidney disease patients[J]. Microcirculation, 2023, 30(5-6): e12819. doi: 10.1111/micc.12819
[29] Greenwood JC, Talebi FM, Jang DH, et al. Low postoperative perfused vessel density is associated with increased soluble endothelial cell adhesion molecules during circulatory shock after cardiac surgery[J]. Microvasc Res, 2023, 150: 104595. doi: 10.1016/j.mvr.2023.104595
[30] Watchorn J, Huang DA, Bramham K, et al. Decreased renal cortical perfusion, independent of changes in renal blood flow and sublingual microcirculatory impairment, is associated with the severity of acute kidney injury in patients with septic shock[J]. Crit Care, 2022, 26(1): 261. doi: 10.1186/s13054-022-04134-6
-

计量
- 文章访问数: 126
- 施引文献: 0



 下载:
下载: