-
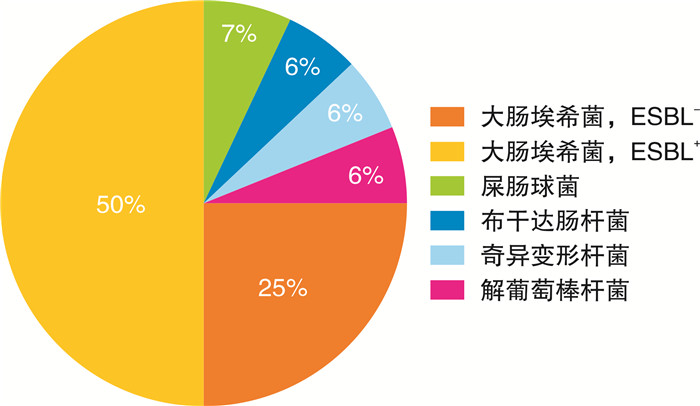
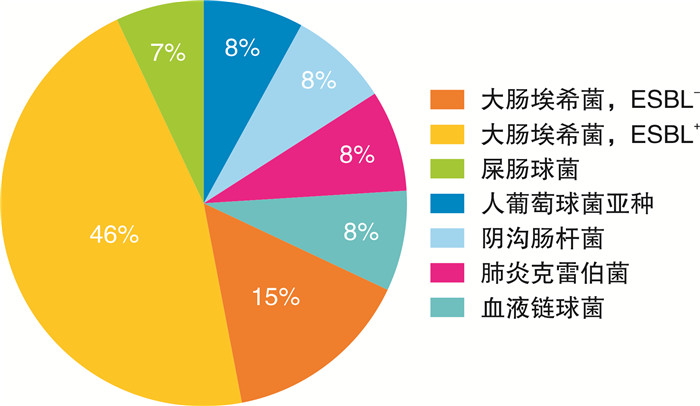
摘要: 目的 探讨重症监护病房(intensive care unit,ICU)收治的尿源性脓毒症患者临床特征的性别差异,为尿源性脓毒症的诊治提供参考。方法 回顾性分析2021年1月—2023年12月医院重症医学二科收治的尿源性脓毒症患者41例为研究对象,男17例,女24例,对不同性别患者的一般资料、干预措施、实验室检查、微生物学培养及临床结局进行分析。结果 两组患者超广谱β-内酰胺酶阳性大肠埃希菌检出率均较高。两组患者的合并症及入ICU时的序贯器官衰竭评分比较,差异无统计学意义(P>0.05)。与男性尿源性脓毒症患者相比,女性患者白细胞计数、体温较高,血红蛋白水平较低;脏器功能方面,女性患者BNP水平较高,血肌酐水平低于男性;女性患者血乳酸水平高于男性;男性患者间羟胺需求量高于女性,均差异有统计学意义(P < 0.05)。结论 在尿源性脓毒症状态下,不同性别ICU患者的临床特征存在一定差异,主要表现在炎症反应、心脏和肾脏器官功能状态、间羟胺等血管活性药物需求等方面。临床医生应关注这种异质性并给予个体化治疗。Abstract: Objective To investigate sex differences in clinical characteristics of intensive care unit (ICU) patients with urosepsis, and to provide reference for the diagnosis and treatment of urosepsis.Methods A retrospective cohort study was conducted on forty-one ICU patients with urosepsis from January 2021 to December 2023. The patients were divided into two groups based on the physiological sex, and the general information, interventional measures, laboratory tests, microbiological culture, and clinical outcomes of the two groups were compared.Results The proportion of female patients with urosepsis in the ICU was higher than that of males. The detection rate of ultra-broad spectrum β-lactamase positive Escherichia coli was higher in both groups. There were no significant differences between the two groups on the comorbidities and sequential organ failure scores on ICU admission. Compared with male patients with urosepsis, female patients had higher white blood cell count, body temperature, and lower hemoglobin levels (P < 0.05). Female patients also had higher BNP and blood lactate levels, and lower blood creatinine levels than male patients (P < 0.05). The use of hydroxylamine was higher in male patients than that in female patients (P < 0.05).Conclusion In the state of urosepsis, there are some differences in clinical characteristics of patients between different genders in ICU, mainly manifested in the inflammatory response, functional status of cardiac and renal organs, and the need for vasoactive drugs such as hydroxylamine. Clinicians should be aware of this heterogeneity and provide individualized treatment.
-
Key words:
- urosepsis /
- sex difference /
- intensive care unit /
- heterogeneity /
- clinical characteristics
-

-
表 1 尿源性脓毒症患者一般临床资料比较
项目 总数(41例) 女(24例) 男(17例) t/χ2 P 年龄/岁 66.73±12.10 67.29±11.40 65.94±13.33 0.339 0.737 泌尿系结石/例(%) 33(80) 20(83) 13(76) Fisher=0.698 高血压病/例(%) 21(51) 10(42) 11(65) 1.293 0.256 糖尿病/例(%) 9(22) 3(12) 6(35) Fisher=0.128 冠心病/例(%) 3(7) 2(8) 1(6) Fisher=1 慢性心力衰竭/例(%) 3(7) 2(8) 1(6) Fisher=1 慢性肾脏病/例(%) 5(12) 2(8) 3(18) Fisher=0.633 脑血管病/例(%) 8(20) 4(17) 4(24) Fisher=0.698 恶性肿瘤/例(%) 4(10) 3(12) 1(6) Fisher=0.629 SOFA评分/分 8.66±3.50 8.17±4.03 9.35±2.55 -1.153 0.256 表 2 两组患者实验室检查结果比较
项目 总数(41例) 女(24例) 男(17例) t/U P 尿白细胞/(个/μL) 758(150,2 445) 641.5(144.38,1 495.1) 1 346(488,3898) 152 0.173 白细胞计数/(×109/L) 23.10±10.06 26.33±10.62 18.54±7.31 2.783 0.008 中性粒细胞百分比/% 92.3(89.0,94.5) 93.5(90.7,95.1) 92.0(87.5,93.0) 263.5 0.118 血红蛋白/(mg/dL) 9.5(8.7,10.9) 9.2(8.3,9.8) 10.1(9.3,11.5) 118.5 0.024 血小板计数/(×109/L) 84.0(37.0,129.0) 96.5(54.3,130.5) 81.0(37.0,129.0) 209.5 0.895 降钙素原/(ng/mL) 74.90(20.70,100.00) 79.53(20.40,100.00) 38.15(24.97,100.00) 240 0.340 高敏C反应蛋白/(mg/L) 212.29±107.05 203.81±115.80 224.27±95.47 -0.618 0.540 血清钙离子/(mmol/L) 1.94±0.08 1.94±0.08 1.95±0.08 -0.297 0.768 碱剩余/(mmol/L) -6.04±4.34 -5.84±4.38 -6.32±4.40 0.346 0.731 体温/℃ 38.40±0.98 38.70±0.90 37.97±0.95 2.476 0.019 收缩压/mmHg 92.41±14.97 89.38±13.80 96.71±15.91 -1.534 0.135 舒张压/mmHg 50.63±9.62 49.62±10.05 52.06±9.09 -0.808 0.424 呼吸频率/(次/min) 27(25,30) 27.5(25,30) 27(24,28) 237 0.388 心率/(次/min) 111.66±20.25 114.12±21.64 108.18±18.17 0.953 0.346 氧分压/mmHg 85.0(70.8,98.0) 87.5(63.9,111.8) 82.3(73.2,93.0) 210.5 0.874 血乳酸/(mmol/L) 2.84(2.19,4.47) 2.99(2.40,4.53) 2.27(1.88,4.07) 281.5 0.042 白蛋白/(g/L) 28.04±4.08 27.79±4.21 28.38±3.98 -0.457 0.650 总胆红素/(μmol/L) 19.6(10.2,38.0) 14.8(10.1,29.8) 24.4(12.6,41.9) 159 0.239 BNP/(pg/mL) 704(439,1 031) 960(637,1 402) 472(357,563) 310 0.004 血肌酐/(μmol/L) 166.0(109.0,292.0) 119.5(95.0,252.5) 192.0(133.0,292.0) 137 0.048 尿素氮/(mmol/L) 12.41(8.54,17.93) 11.38(6.77,16.43) 14.17(10.21,18.38) 141 0.098 PT/S 14.2(12.9,15.4) 14.3(13.1,15.8) 14.2(12.8,15.0) 224 0.606 APTT/S 30.8(27.6,34.5) 31.1(27.1,35.9) 30.8(28.6,32.6) 219.5 0.691 INR 1.23(1.11,1.33) 1.23(1.12,1.37) 1.23(1.10,1.30) 218.5 0.711 注:1 mmHg=0.133 kPa。 表 3 两组患者微生物培养比较
项目 总数(41例) 女(24例) 男(17例) U/χ2 P 任意标本阳性/例(%) 23(56) 12(50) 11(65) 0.379 0.538 血培养阳性/例(%) 13(32) 7(29) 6(35) 0.006 0.940 尿培养阳性/例(%) 16(39) 8(33) 8(47) 0.317 0.574 尿细菌数/(个/μL) 243.0(43.5,673.0) 174.6(34.2,416.6) 474.7(102.3,1 096.0) 156.0 0.209 表 4 两组患者住院期间干预措施比较
项目 总数(41例) 女(24例) 男(17例) U/χ2 P 外科手术干预/例(%) 36(88) 23(96) 13(76) Fisher=0.141 肾脏替代治疗/例(%) 5(12) 3(12) 2(12) Fisher=1.000 深静脉穿刺/例(%) 17(41) 12(50) 5(29) 0.993 0.319 血管活性药物使用/例(%) 32(78) 17(71) 15(88) Fisher=0.262 间羟胺消耗量/mg 50(0,110) 50(0,50) 100(50,150) 112.0 0.011 NEE 12.50(6.25,43.75) 6.25(0,30.69) 18.75(6.25,43.75) 168.5 0.350 碳青霉烯类药物消耗量/g 7.0(5.0,10.0) 7.3(4.6,9.1) 7.0(5.0,10.5) 196.5 0.853 前48 h液体正平衡/例(%) 24(59) 15(62) 9(53) 0.084 0.772 输血治疗/例(%) 10(24) 6(25) 4(24) Fisher=1.000 表 5 两组患者临床结局比较
项目 总数(41例) 女(24例) 男(17例) U/χ2 P ICU停留时间/d 2.75(1.88,3.62) 2.81(1.77,3.68) 2.67(1.92,3.50) 213.5 0.812 住院时间/d 9.0(6.0,13.0) 8.5(6.0,12.3) 9.0(7.0,13.0) 186.5 0.651 总住院费用/元 36 258.84(25 763.66,43 701.80) 36 449.18(27 489.89,43 057.22) 31 678.67(22 262.21,45 486.49) 228.0 0.538 生存率/例(%) 38(93) 22(92) 16(94) Fisher=1.000 -
[1] Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 762-774. doi: 10.1001/jama.2016.0288
[2] Peters-Sengers H, Butler JM, Uhel F, et al. MARS consortium. Source-specific host response and outcomes in critically ill patients with sepsis: a prospective cohort study[J]. Intensive Care Med, 2022, 48(1): 92-102. doi: 10.1007/s00134-021-06574-0
[3] 汪雨贺, 王雪, 高山, 等. 基于MIMIC-Ⅲ的脓毒症患者临床特点与预后相关性分析[J]. 临床急诊杂志, 2022, 23(12): 863-869. doi: 10.13201/j.issn.1009-5918.2022.12.012
[4] Guliciuc M, Maier AC, Maier IM, et al. The Urosepsis-A Literature Review[J]. Medicina(Kaunas), 2021, 57(9): 872.
[5] Tandogdu Z, Koves B, Ristovski S, et al. SERPENS Investigators. Urosepsis 30-day mortality, morbidity, and their risk factors: SERPENS study, a prospective, observational multi-center study[J]. World J Urol, 2024, 42(1): 314. doi: 10.1007/s00345-024-04979-2
[6] Merdji H, Long MT, Ostermann M, et al. Sex and gender differences in intensive care medicine[J]. Intensive Care Med, 2023, 49(10): 1155-1167. doi: 10.1007/s00134-023-07194-6
[7] Zimmermann T, Kaufmann P, Amacher SA, et al. Swiss ICU Trial group. Sex differences in the SOFA score of ICU patients with sepsis or septic shock: a nationwide analysis[J]. Crit Care, 2024, 28(1): 209. doi: 10.1186/s13054-024-04996-y
[8] Modra LJ, Higgins AM, Pilcher DV, et al. Sex Differences in Mortality of ICU Patients According to Diagnosis-related Sex Balance[J]. Am J Respir Crit Care Med, 2022, 206(11): 1353-1360. doi: 10.1164/rccm.202203-0539OC
[9] Mewes C, Runzheimer J, Böhnke C, et al. Association of Sex Differences with Mortality and Organ Dysfunction in Patients with Sepsis and Septic Shock[J]. J Pers Med, 2023, 13(5): 836. doi: 10.3390/jpm13050836
[10] Ko RE, Kang D, Cho J, et al. Korean Sepsis Alliance(KSA)investigators. Influence of gender on age-associated in-hospital mortality in patients with sepsis and septic shock: a prospective nationwide multicenter cohort study[J]. Crit Care, 2023, 27(1): 229. doi: 10.1186/s13054-023-04515-5
[11] Sunden-Cullberg J, Nilsson A, Inghammar M. Sex-based differences in ED management of critically ill patients with sepsis: a nationwide cohort study[J]. Intensive Care Med, 2020, 46(4): 727-736. doi: 10.1007/s00134-019-05910-9
[12] Dickson K, Zhou J, Lehmann C. Lower Urinary Tract Inflammation and Infection: Key Microbiological and Immunological Aspects[J]. J Clin Med, 2024, 13(2): 315. doi: 10.3390/jcm13020315
[13] Kotani Y, Di Gioia A, Landoni G, et al. An updated "norepinephrine equivalent" score in intensive care as a marker of shock severity[J]. Crit Care, 2023, 27(1): 29. doi: 10.1186/s13054-023-04322-y
[14] 陈正钢, 刘励军. 急诊脓毒症患者早期筛查生物标志物的研究现状与展望[J]. 临床急诊杂志, 2023, 24(2): 99-104. doi: 10.13201/j.issn.1009-5918.2023.02.010
[15] 姚咏明, 杜晓辉. 浅析脓毒症发病的性别差异及其机制[J]. 中华危重病急救医学, 2009, 21(3): 129-130.
[16] Ferreira FL, Bota DP, Bross A, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients[J]. JAMA, 2001, 286(14): 1754-1758. doi: 10.1001/jama.286.14.1754
[17] 陈卫, 石齐芳, 陈嵩, 等. qSOFA评分联合休克指数评估脓毒症患者预后的价值[J]. 临床急诊杂志, 2023, 24(3): 126-130. doi: 10.13201/j.issn.1009-5918.2023.03.004
[18] Dominguez JM, Kippin TE. Introduction to Special Issue: Hormones, Sex Differences, and Drug Response[J]. Physiol Behav, 2019, 203: 1-2. doi: 10.1016/j.physbeh.2019.02.039
[19] Bonkat G, Cai T, Veeratterapillay R, et al. Management of Urosepsis in 2018[J]. Eur Urol Focus, 2019, 5(1): 5-9. doi: 10.1016/j.euf.2018.11.003
-

| 引用本文: | 张金, 张洋, 肖文艳, 等. 重症监护病房尿源性脓毒症患者临床特征的性别差异[J]. 临床急诊杂志, 2024, 25(9): 456-460. doi: 10.13201/j.issn.1009-5918.2024.09.002 |
| Citation: | ZHANG Jin, ZHANG Yang, XIAO Wenyan, et al. Sex differences in the clinical characteristics of patients with urosepsis in ICU[J]. J Clin Emerg, 2024, 25(9): 456-460. doi: 10.13201/j.issn.1009-5918.2024.09.002 |
- Figure 1.
- Figure 2.



 下载:
下载: