Relationship between optic nerve sheath diameter and intracranial pressure after hyperventilation in patients with severe craniocerebral trauma
-
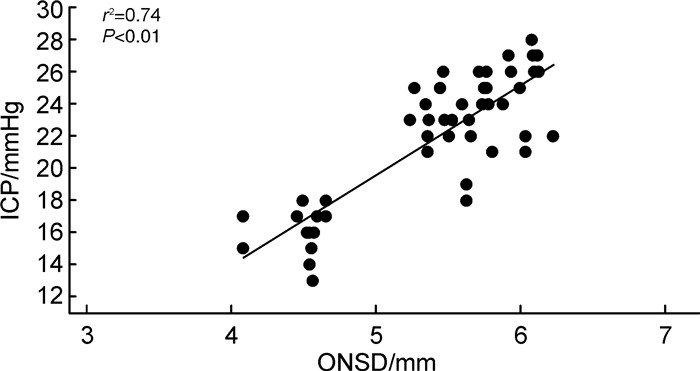
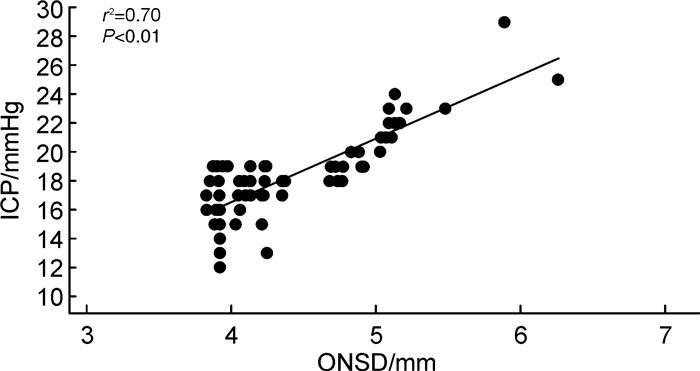
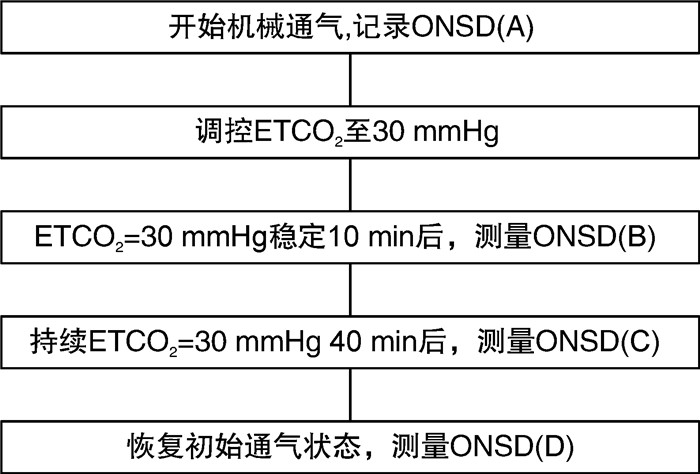
摘要: 目的 探索重型颅脑外伤(traumatic brain injury,TBI)患者过度通气前后超声测量神经鞘直径(optical nerve sheath diameter,ONSD)与颅内压(intracranial pressure,ICP)的关系。方法 前瞻性收集2023年1月—2023年12月我院急诊重症监护病房住院治疗并接受有创ICP监测的74例重型TBI患者,其中男43例,女31例;平均年龄(57.09±4.03)岁。对入组患者完成4次ONSD监测[呼气末二氧化碳(end-tidal carbon dioxide,ETCO2)在基线水平、ETCO2从基线水平调控至30 mmHg(1 mmHg=0.133 kPa)的起始及结束阶段、ETCO2再次恢复至基线水平],在测量ONSD的同时记录同期ICP值,并收集同期平均动脉压、动脉血氧饱和度、pH和PaCO2。记录ETCO2变化前后ONSD的动态改变,采用Wilcoxon秩和检验比较ETCO2变化前后ONSD的差异。采用Spearman方法评估ETCO2在基线水平及30 mmHg时ONSD与ICP间的关系。结果 ONSD在ETCO2基线水平时中位数为5.15(4.02~6.63) mm,在ETCO2为30 mmHg期间显著降低至4.73(3.67~5.91) mm(P=0.01)。ICP在ETCO2基线水平时均数为(23.30±5.01)mmHg,在ETCO2为30 mmHg期间显著降低至(17.22±3.14)mmHg(P=0.03)。PaCO2、pH在ETCO2基线水平及ETCO2为30 mmHg时对比,差异有统计学意义(P < 0.05)。Spearman相关分析显示,ETCO2在基线水平及30 mmHg时,ONSD与有创ICP之间存在线性相关关系(基线水平:r2=0.74,95%CI:0.66~0.80,P < 0.01;ETCO2为30 mmHg:r2=0.70,95%CI:0.63~0.78,P < 0.01)。结论 重型TBI患者在过度通气下,ONSD呈下降趋势,且与同期ICP具有线性关系。提示对采取过度通气下的重型TBI患者,动态监测ONSD能够反映ICP的实时变化。Abstract: Objective To explore the relationship between optical nerve sheath diameter (ONSD) and intracranial pressure (ICP) before and after hyperventilation in patients with severe traumatic brain injury (TBI).Methods Patients with severe TBI who were hospitalized in our emergency intensive care unit and received invasive ICP monitoring from January 2023 to December 2023 were prospectively collected. A total of 74 patients with TBI were included in this study, 43 males and 31 females with a mean age of (57.09±4.03) years. Four ONSDs monitoring(end-tidal carbon dioxide[ETCO2]at the baseline level, at the beginning and end of ETCO2 modulation from the baseline level to 30 mmHg[1 mmHg=0.133 kPa], and the return of ETCO2 to the baseline level)were completed in the enrolled patients. ICP values for the same time period were recorded at the same time while ONSDs was measured, and mean arterial pressure, arterial oxygen saturation, pH, and PaCO2 were collected during the same period. The dynamic changes of ONSD before and after the changes of ETCO2 were recorded, and the Wilcoxon rank sum test was used to compare the differences of ONSD before and after the changes of ETCO2. Spearman method was used to evaluate the relationship between ONSD and ICP at baseline and 30mmHg ETCO2.Results The median baseline ETCO2 level of ONSD was 5.15 (4.02-6.63) mm and reduced significantly to 4.73(3.67-5.91)mm during the period of ETCO2 of 30 mmHg (P= 0.01). ICP at baseline of ETCO2 averaged(23.30±5.01)mmHg and significantly decreased to(17.22±3.14)mmHg during ETCO2 30 mmHg (P=0.03). The difference of PaCO2 and pH was statistically significant when compared at baseline level of ETCO2 and ETCO2 30 mmHg (P < 0.05). Spearman correlation analysis showed a linear correlation between ONSD and invasive ICP at baseline and 30 mmHg of ETCO2 (baseline level: r2= 0.74, 95%CI: 0.66-0.80, P < 0.01; ETCO2 of 30 mmHg: r2=0.70, 95%CI: 0.63-0.78, P < 0.01).Conclusion In patients with severe TBI under hyperventilation, ONSD showed a decreasing trend and had a linear relationship with ICP during the same period. This suggests that dynamic monitoring of ONSD can reflect real-time changes in ICP in patients with heavy TBI under hyperventilation.
-

-
表 1 ETCO2变化前后各观察指标的变化
X ± S 参数 ETCO2 P 调控前(基线) 30 mmHg ONSD/mm 5.15(4.02~6.63) 4.73(3.67~5.91) 0.01 ICP/mmHg 23.30±5.01 17.22±3.14 0.03 PaCO2/mmHg 39.5±4.2 32.5±3.7 0.01 pH 7.31±0.10 7.47±0.22 0.02 SaO2/% 99.00±0.33 98.10±0.12 0.70 心率/(次/min) 73.10±17.77 77.10±13.21 0.10 MAP/mmHg 76.10±10.78 78.10±11.38 0.20 -
[1] Jiang JY, Gao GY, Feng JF, et al. Traumatic brain injury in China[J]. Lancet Neurol, 2019, 18(3): 286-295. doi: 10.1016/S1474-4422(18)30469-1
[2] 顾帅鹏, 龚嵩, 高伟. 颅内压监测在颅脑损伤中的应用进展[J]. 临床急诊杂志, 2024, 25(2): 87-92, 98. doi: 10.13201/j.issn.1009-5918.2024.02.007
[3] 张志花, 赵平, 汤建磊, 等. 急性中重型颅脑损伤后亚低温治疗对凝血功能及预后的影响[J]. 临床急诊杂志, 2024, 25(1): 28-31. doi: 10.13201/j.issn.1009-5918.2024.01.006
[4] Carney N, Totten AM, O'Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition[J]. Neurosurgery, 2017, 80(1): 6-15. doi: 10.1227/NEU.0000000000001432
[5] Robba C, Graziano F, Rebora P, et al. Intracranial pressure monitoring in patients with acute brain injury in the intensive care unit(SYNAPSE-ICU): an international, prospective observational cohort study[J]. Lancet Neurol, 2021, 20(7): 548-558. doi: 10.1016/S1474-4422(21)00138-1
[6] Glushakova OY, Glushakov AV, Yang L, et al. Intracranial Pressure Monitoring in Experimental Traumatic Brain Injury: Implications for Clinical Management[J]. Neurotrauma, 2020, 37(22): 2401-2413. doi: 10.1089/neu.2018.6145
[7] 曹霞, 张蓉蓉, 薛晓宏. 颅内压联合PCT与NSE监测对重型颅脑损伤患者病情的预测价值研究[J]. 临床急诊杂志, 2023, 24(3): 137-142. doi: 10.13201/j.issn.1009-5918.2023.03.006
[8] Hirzallah MI, Lochner P, Hafeez MU, et al. Quality assessment of optic nerve sheath diameter ultrasonography: Scoping literature review and Delphi protocol[J]. Neuroimaging, 2022, 32(5): 808-824. doi: 10.1111/jon.13018
[9] Rasulo FA, Bertuetti R. Transcranial Doppler and Optic Nerve Sonography[J]. Cardiothorac Vasc Anesth, 2019, 33(Suppl 1): S38-S52.
[10] Sterrett ME, Austin B, Barnes RM, et al. Optic nerve sheath diameter in severe preeclampsia with neurologic features versus controls[J]. BMC Pregnancy Childbirth, 2022, 22(1): 224. doi: 10.1186/s12884-022-04548-8
[11] 卢安阳, 吕汝琦. 呼气末二氧化碳动态变化与亚低温治疗的心肺复苏患者神经预后的关系研究[J]. 临床急诊杂志, 2022, 23(8): 548-552. doi: 10.13201/j.issn.1009-5918.2022.08.002
[12] Robba C, Battaglini D, Abbas A, et al. Clinical practice and effect of carbon dioxide on outcomes in mechanically ventilated acute brain-injured patients: a secondary analysis of the ENIO study[J]. Intensive Care Med, 2024, 50(2): 234-246. doi: 10.1007/s00134-023-07305-3
[13] Al-Hassani A, Strandvik G, Abayazeed S, et al. Relationship of Optic Nerve Sheath Diameter and Intracranial Hypertension in Patients with Traumatic Brain Injury[J]. Emerg Trauma Shock, 2020, 13(3): 183-189. doi: 10.4103/JETS.JETS_103_19
[14] Stevens RRF, Gommer ED, Aries MJH, et al. Optic nerve sheath diameter assessment by neurosonology: A review of methodologic discrepancies[J]. Neuroimaging, 2021, 31(5): 814-825. doi: 10.1111/jon.12906
[15] Pansell J, Bell M, Rudberg P, et al. Optic nerve sheath diameter measurement by ultrasound: Evaluation of a standardized protocol[J]. Neuroimaging, 2022, 32(1): 104-110. doi: 10.1111/jon.12936
[16] Cnossen MC, Huijben JA, van der Jagt M, et al. Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study[J]. Crit Care, 2017, 21(1): 233. doi: 10.1186/s13054-017-1816-9
[17] Hawryluk GWJ, Aguilera S, Buki A, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference(SIBICC)[J]. Intensive Care Med, 2019, 45(12): 1783-1794. doi: 10.1007/s00134-019-05805-9
[18] Robba C, Poole D, McNett M, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicineconsensus[J]. Intensive Care Med, 2020, 46(12): 2397-2410. doi: 10.1007/s00134-020-06283-0
[19] Gouvea Bogossian E, Peluso L, Creteur J, et al. Hyperventilation in Adult TBI Patients: How to Approach It[J]. Front Neurol, 2021, 28: 11: 580859. http://www.socolar.com/Article/Index?aid=100086450448&jid=100000009585
[20] Robba C, Taccone FS, Citerio G. Monitoring cerebral oxygenation in acute brain-injury patients[J]. Intensive Care Med, 2022, 48(10): 1463-1466. doi: 10.1007/s00134-022-06788-w
[21] Cinotti R, Mijangos JC, Pelosi P, et al. Extubation in neurocritical care patients: the ENIO international prospective study[J]. Intensive Care Med, 2022, 48(11): 1539-1550. doi: 10.1007/s00134-022-06825-8
[22] Dinsmore M, Han JS, Fisher JA, et al. Effects of acute controlled changes in end-tidal carbon dioxide on the diameter of the optic nerve sheath: a transorbital ultrasonographic study in healthy volunteers[J]. Anaesthesia, 2017, 72(5): 618-623. doi: 10.1111/anae.13784
[23] Brandi G, Stocchetti N, Pagnamenta A, et al. Cerebral metabolism is not affected by moderate hyperventilation in patients with traumatic brain injury[J]. Crit Care, 2019, 23(1): 45. doi: 10.1186/s13054-018-2304-6
[24] Danes D, Vaishnav J, Pillai L, et al. Effect of Respiratory Physiological Changes on Optic Nerve Sheath Diameter and Cerebral Oxygen Saturation in Patients With Acute Traumatic Brain Injury[J]. Neurosurg Anesthesiol, 2022, 34(1): e52-e56. doi: 10.1097/ANA.0000000000000706
[25] Claassen JAHR, Thijssen DHJ, Panerai RB, et al. Regulation of cerebral blood flow in humans: physiology and clinical implications of autoregulation[J]. Physiol Rev, 2021, 101(4): 1487-1559. doi: 10.1152/physrev.00022.2020
-




 下载:
下载: