Relationship between serum Ang-2 and IFABP levels and survival within 28 days after admission in patients with acute ST segment elevation myocardial infarction complicated with cardiogenic shock
-
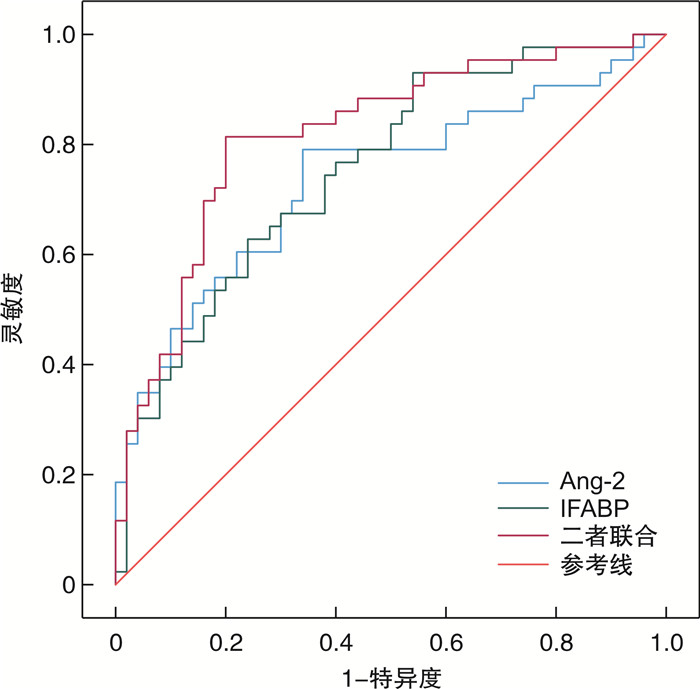
摘要: 目的 探究血清血管生成素-2(angiopoietin-2,Ang-2)、肠型脂肪酸结合蛋白(intestinal fatty acid binding protein,IFABP)水平与急性ST段抬高型心肌梗死(ST segment elevation myocardial infarction,STEMI)并发心源性休克(cardiogenic shock,CS)患者入院后28 d内生存的关系。方法 选取邯郸市中心医院2020年5月—2023年10月收治的162例STEMI患者,有61例患者就诊时并发CS(并发CS组),101例患者就诊时没有并发CS(非CS组);另选取健康者98例作为对照组。根据入院后28 d生存情况将并发CS组分成生存组(患者存活)34例和死亡组(患者死亡)27例。收集所有受试者临床资料,检测实验室指标和血清Ang-2、IFABP水平;分析STEMI并发CS患者血清Ang-2、IFABP与临床资料、实验室指标的相关性,STEMI并发CS患者入院后28 d内生存的影响因素,Ang-2、IFABP预测STEMI并发CS患者入院后28 d内生存的价值。结果 与对照组比较,非CS组和并发CS组空腹血糖(fasting plasma glucose,FPG)、总胆固醇(total cholesterol,TC)、甘油三酯(triglyceride,TG)、低密度脂蛋白胆固醇(low density lipoprotein-cholesterol,LDL-C)、肌酸激酶同工酶(creatine kinase isoenzyme,CK-MB)、同型半胱氨酸(homocysteine,Hcy)、心肌肌钙蛋白I(cardiac troponin I,cTnI)、Ang-2、IFABP水平显著升高,高密度脂蛋白胆固醇(high density lipoprotein cholesterol,HDL-C)、左心室射血分数(left ventricular ejection fraction,LVEF)水平显著降低(P < 0.05)。与非CS组比较,并发CS组多支心肌罪犯血管数患者比例、TC、TG、CK-MB、Hcy、cTnI、Ang-2、IFABP水平显著升高,HDL-C、LVEF水平显著降低(P < 0.05)。与生存组比较,死亡组糖尿病史、高脂血症史、多支心肌罪犯血管数患者比例、FPG、TC、TG、LDL-C、CK-MB、Hcy、cTnI、Ang-2、IFABP水平显著升高,HDL-C、LVEF水平显著降低(P < 0.05)。STEMI并发CS患者血清Ang-2与IFABP水平呈正相关(P < 0.05);血清Ang-2、IFABP均与糖尿病史、高脂血症史、心肌罪犯血管数量、FPG、TC、TG、LDL-C、CK-MB、Hcy、cTnI呈正相关,与HDL-C、LVEF呈负相关(P < 0.05)。有糖尿病史、有高脂血症史、多支心肌罪犯血管数、FPG、TC、TG、LDL-C、CK-MB、Hcy、cTnI、Ang-2、IFABP均是影响STEMI并发CS患者入院后28 d内生存的独立危险因素,HDL-C、LVEF均是影响STEMI并发CS患者入院后28 d内生存的独立保护因素(P < 0.05)。相较于血清Ang-2、IFABP单独预测STEMI并发CS患者入院后28 d内生存的曲线下面积(AUC)(0.741、0.759),二者联合预测的AUC(0.836)更高(P < 0.05)。结论 STEMI并发CS患者血清Ang-2、IFABP水平较高,其高水平可能导致患者入院后28 d内死亡,Ang-2和IFABP联合检测对STEMI并发CS患者入院后28 d内生存有较高预测价值。
-
关键词:
- 急性ST段抬高型心肌梗死 /
- 心源性休克 /
- 血管生成素-2 /
- 肠型脂肪酸结合蛋白 /
- 生存
Abstract: Objective To explore the relationship between serum angiopoietin-2 (Ang-2) and intestinal fatty acid binding protein (IFABP) levels and survival within 28 days after admission in patients with acute ST segment elevation myocardial infarction (STEMI) complicated with cardiogenic shock (CS).Methods One hundred and sixty-two patients with STEMI admitted to Handan Central Hospital from May 2020 to October 2023 were selected, there were 61 patients with concurrent CS at the time of visit (concurrent CS group) and 101 patients with no concurrent CS at the time of visit (non-CS group); another 98 healthy volunteers were selected as control group. According to the survival conditions 28 days after admission, the concurrent CS group was divided into survival group (34 patients survived with good prognosis) and death group (27 patients died with poor prognosis). Clinical data of all subjects were collected and laboratory indexes and serum levels of Ang-2 and IFABP were detected; the correlation between serum Ang-2, IFABP and clinical data and laboratory indexes in patients with STEMI complicated with CS, the influencing factors of survival within 28 days after admission in patients with STEMI complicated with CS, and the value of Ang-2 and IFABP in predicting survival within 28 days after admission in patients with STEMI complicated with CS were analyzed.Results Compared with control group, fasting plasma glucose (FPG), total cholesterol (TC), triglyceride (TG), low density lipoprotein-cholesterol (LDL-C), creatine kinase isoenzyme (CK-MB), homocysteine (Hcy), cardiac troponin I (cTnI), Ang-2 and IFABP levels in non-CS group and concurrent CS group were significantly increased, the levels of high density lipoprotein cholesterol (HDL-C) and left ventricular ejection fraction (LVEF) were significantly decreased (P < 0.05); compared with non-CS group, the proportion of patients with multiple myocardial culprit vessels, the levels of TC, TG, CK-MB, Hcy, cTnI, Ang-2 and IFABP in concurrent CS group were significantly increased, while the levels of HDL-C and LVEF were significantly decreased (P < 0.05). Compared with survival group, the proportion of diabetes history, hyperlipidemia history, patients with multiple myocardial culprit vessels, FPG, TC, TG, LDL-C, CK-MB, Hcy, cTnI, Ang-2 and IFABP levels in death group were significantly increased, while the levels of HDL-C and LVEF were significantly decreased (P < 0.05). Serum Ang-2 was positively correlated with IFABP level in STEMI patients complicated with CS (P < 0.05); serum Ang-2 and IFABP were positively correlated with history of diabetes mellitus, history of hyperlipidemia, number of myocardial criminal vessels, FPG, TC, TG, LDL-C, CK-MB, Hcy and cTnI, and negatively correlated with HDL-C and LVEF (P < 0.05). History of diabetes, history of hyperlipidemia, number of multiple myocardial offender vessels, FPG, TC, TG, LDL-C, CK-MB, Hcy, cTnI, Ang-2 and IFABP were all independent risk factors for survival within 28 days after admission in STEMI patients complicated with CS, both HDL-C and LVEF were independent protective factors for survival within 28 days after admission in STEMI patients complicated with CS (P < 0.05). Compared with the area under curve (AUC) of serum Ang-2 and IFABP alone in predicting survival within 28 days after admission of STEMI patients with CS (0.741, 0.759), the AUC of serum Ang-2 and IFABP combined in predicting survival within 28 days after admission was higher (0.836, P < 0.05).Conclusion The serum levels of Ang-2 and IFABP in patients with STEMI complicated with CS are high, which may lead to death within 28 days after admission of patients, the combined detection of Ang-2 and IFABP has a high predictive value for the survival within 28 days after admission of STEMI complicated with CS. -

-
表 1 对照组、非CS组、并发CS组临床资料、实验室指标及血清Ang-2、IFABP水平的比较
X±S 组别 对照组(98例) 非CS组(101例) 并发CS组(61例) F/χ2 P 年龄/岁 57.69±7.24 57.79±7.96 58.04±8.13 0.352 0.703 性别/例 0.033 0.855 男 61 61 38 女 37 40 23 糖尿病史/例(%) - 32(31.68) 26(42.62) 1.980 0.159 高血压史/例(%) - 39(38.61) 28(45.90) 0.833 0.361 高脂血症史/例(%) - 31(30.69) 25(40.98) 1.781 0.182 心肌罪犯血管数量(1支/多支) - 65/36 28/33 5.297 0.021 RBC/(×1012/L) 4.18±0.63 4.15±0.71 4.20±0.59 0.150 0.861 WBC/(×109/L) 5.08±0.72 5.12±0.75 5.05±0.68 0.237 0.789 PLT/(×109/L) 161.53±32.07 157.71±34.11 155.94±31.58 0.737 0.479 FPG/(mmol/L) 5.03±0.62 5.91±1.281) 6.08±1.351) 24.129 <0.001 TC/(mmol/L) 3.07±0.58 4.69±0.911) 5.01±1.121)2) 131.695 <0.001 TG/(mmol/L) 1.18±0.29 1.51±0.351) 1.67±0.411)2) 48.439 <0.001 HDL-C/(mmol/L) 1.31±0.22 0.92±0.151) 0.77±0.131)2) 255.975 <0.001 LDL-C/(mmol/L) 2.24±0.53 3.29±0.741) 3.41±0.771) 85.476 <0.001 CK-MB/(μg/L) 2.35±0.48 33.86±5.291) 46.79±6.151)2) 2200.551 <0.001 Hcy/(μmol/L) 7.19±0.85 20.14±3.711) 29.53±5.091)2) 908.976 <0.001 cTnI/(μg/L) 0.11±0.02 3.98±0.531) 4.77±0.681)2) 4293.607 <0.001 LVEF/% 61.17±5.08 41.09±5.131) 36.53±6.771)2) 517.365 <0.001 Ang-2/(mg/L) 1.03±0.22 2.14±0.461) 2.79±0.551)2) 295.706 <0.001 IFABP/(ng/L) 298.62±48.71 417.35±70.621) 596.53±81.801)2) 233.518 <0.001 与对照组比较,1)P<0.05;与非CS组比较,2)P<0.05。 表 2 生存组和死亡组临床资料、实验室指标及血清Ang-2、IFABP水平的比较
X±S 组别 生存组(34例) 死亡组(27例) t/χ2 P 年龄/岁 57.98±7.83 58.12±8.51 0.067 0.947 性别/例 0.009 0.924 男 21 10 女 13 17 糖尿病史/例(%) 10(29.41) 16(59.26) 5.482 0.019 高血压史/例(%) 14(41.18) 14(51.85) 0.691 0.406 高脂血症史/例(%) 10(29.41) 15(55.56) 4.253 0.039 心肌罪犯血管数量(1支/多支) 20/14 8/19 5.165 0.023 RBC/(×1012/L) 4.17±0.57 4.24±0.62 0.458 0.648 WBC/(×109/L) 5.10±0.71 4.99±0.64 0.628 0.533 PLT/(×109/L) 158.66±32.41 152.51±30.53 0.755 0.453 FPG/(mmol/L) 5.11±1.25 7.30±1.48 6.264 <0.001 TC/(mmol/L) 4.25±0.98 5.97±1.30 5.893 <0.001 TG/(mmol/L) 1.50±0.38 1.88±0.45 3.575 0.001 HDL-C/(mmol/L) 0.85±0.16 0.67±0.09 5.221 <0.001 LDL-C/(mmol/L) 3.04±0.69 3.88±0.87 4.207 <0.001 CK-MB/(μg/L) 39.82±5.97 55.57±6.38 9.928 <0.001 Hcy/(μmol/L) 25.61±4.42 34.47±5.93 6.686 <0.001 cTnI/(μg/L) 4.36±0.61 5.29±0.77 5.266 <0.001 LVEF/% 38.59±6.94 33.94±6.56 2.662 0.01 Ang-2/(mg/L) 2.29±0.43 3.42±0.70 7.757 <0.001 IFABP/(ng/L) 522.26±79.89 690.06±84.21 7.957 <0.001 表 3 STEMI并发CS患者血清Ang-2、IFABP与临床资料、实验室指标的相关性分析
指标 Ang-2 IFABP r P r P IFABP 0.429 <0.001 - - 糖尿病史 0.539 <0.001 0.545 <0.001 高脂血症史 0.498 <0.001 0.509 <0.001 心肌罪犯血管数量 0.524 <0.001 0.571 <0.001 FPG 0.446 <0.001 0.492 <0.001 TC 0.512 <0.001 0.536 <0.001 TG 0.483 <0.001 0.507 <0.001 HDL-C -0.463 <0.001 -0.518 <0.001 LDL-C 0.515 <0.001 0.564 <0.001 CK-MB 0.601 <0.001 0.627 <0.001 Hcy 0.582 <0.001 0.594 <0.001 cTnI 0.533 <0.001 0.579 <0.001 LVEF -0.568 <0.001 -0.624 <0.001 表 4 Cox回归分析STEMI并发CS患者入院后28 d内生存的影响因素
自变量 β SE Wald P HR 95%CI 糖尿病史 0.816 0.294 7.703 0.006 2.261 1.271~4.024 高脂血症史 0.729 0.305 5.713 0.017 2.073 1.140~3.769 心肌罪犯血管数量 0.856 0.313 7.479 0.006 2.354 1.274~4.347 FPG 0.652 0.283 5.308 0.021 1.919 1.102~3.342 TC 0.705 0.261 7.296 0.007 2.024 1.213~3.376 TG 0.853 0.314 7.380 0.007 2.347 1.268~4.342 HDL-C -0.758 0.255 8.836 0.003 0.469 0.284~0.772 LDL-C 0.902 0.324 7.750 0.005 2.465 1.306~4.651 CK-MB 0.849 0.338 6.309 0.012 2.337 1.205~4.533 Hcy 0.698 0.217 10.346 0.001 2.010 1.313~3.075 cTnI 0.917 0.233 15.489 <0.001 2.502 1.585~3.950 LVEF -0.886 0.264 11.263 0.001 0.412 0.246~0.692 Ang-2 0.857 0.279 9.435 0.002 2.356 1.364~4.071 IFABP 0.911 0.325 7.857 0.005 2.487 1.315~4.702 表 5 血清Ang-2、IFABP预测STEMI并发CS患者入院后28 d内生存的价值
指标 截断值 AUC 95%CI 灵敏度/% 特异度/% 约登指数 Ang-2 2.81 mg/L 0.741 0.629~0.838 60.92 77.58 0.385 IFABP 602.38 ng/L 0.759 0.660~0.849 63.14 72.39 0.355 二者联合 - 0.836 0.728~0.911 81.78 70.26 0.520 -
[1] 陈振飞, 方曹阳, 张静, 等. 血清YKL-40联合CHA2DS2-VASc-HSF评分在急性ST段抬高型心肌梗死诊断中的价值[J]. 临床心血管病杂志, 2022, 38(8): 643-648. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202208015.htm
[2] 张同昌, 李海山, 陈敏, 等. 血浆致动脉硬化指数评价急性ST段抬高型心肌梗死的临床价值[J]. 临床急诊杂志, 2023, 24(7): 359-363. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.07.005
[3] Sato R, Hasegawa D, Guo SC, et al. Temporary mechanical circulatory support in sepsis-associated cardiogenic shock with and without acute myocardial infarction[J]. J Cardiothorac Vasc Anesth, 2024, 38(1): 207-213. doi: 10.1053/j.jvca.2023.09.026
[4] Kunkel KJ, Fuller B, Basir MB. Management of Cardiogenic Shock in Patients with Acute Myocardial Infarction[J]. Interv Cardiol Clin, 2021, 10(3): 345-357.
[5] Khosraviani N, Wu R, Fish JE. Angiopoietin-2: An Emerging Tie to Pathological Vessel Enlargement[J]. Arterioscler Thromb Vasc Biol, 2022, 42(1): 3-5. doi: 10.1161/ATVBAHA.121.317102
[6] Skowerski T, Nabrdalik K, Kwiendacz H, et al. Angiopoietin-2 as a biomarker of non-ST-segment elevation myocardial infarction in patients with or without type 2 diabetes[J]. Arch Med Sci, 2019, 18(3): 624-631.
[7] Wu C, Zhu X, Ren H, et al. Intestinal fatty acid-binding protein as a biomarker for the diagnosis of strangulated intestinal obstruction: A meta-analysis[J]. Open Med (Wars), 2021, 16(1): 264-273. doi: 10.1515/med-2021-0214
[8] Kastl SP, Krychtiuk KA, Lenz M, et al. Intestinal Fatty Acid Binding Protein is Associated With Mortality in Patients With Acute Heart Failure or Cardiogenic Shock[J]. Shock, 2019, 51(4): 410-415. doi: 10.1097/SHK.0000000000001195
[9] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019, 47(10): 766-783. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJXB201709002.htm
[10] Vahdatpour C, Collins D, Goldberg S. Cardiogenic Shock[J]. J Am Heart Assoc, 2019, 8(8): e011991. doi: 10.1161/JAHA.119.011991
[11] Nishihira K, Honda S, Takegami M, et al. Percutaneous coronary intervention for ST-elevation myocardial infarction complicated by cardiogenic shock in a super-aging society[J]. Eur Heart J Acute Cardiovasc Care, 2023, 12(12): 847-855. doi: 10.1093/ehjacc/zuad113
[12] Wang Y, Fang J, Niu T, et al. Serum Ang-1/Ang-2 ratio may be a promising biomarker for evaluating severity of diabetic retinopathy[J]. Graefes Arch Clin Exp Ophthalmol, 2023, 261(1): 49-55. doi: 10.1007/s00417-022-05745-z
[13] Chen SM, Li D, Xing X, et al. Higher serum angiopoietin 2 levels are independently associated with coronary microvascular dysfunction in patients with angina in the absence of obstructive coronary artery disease[J]. Chin Med J (Engl), 2020, 133(14): 1662-1668. doi: 10.1097/CM9.0000000000000812
[14] Ranjbar K. Improved Cardiac Function Following Ischemia Reperfusion Injury Using Exercise Preconditioning and L-Arginine Supplementation via Oxidative Stress Mitigation and Angiogenesis Amelioration[J]. Cardiovasc Toxicol, 2022, 22(8): 736-745. doi: 10.1007/s12012-022-09752-8
[15] 蒋玲, 邱实, 陈丽梅, 等. 血清Ang-2、cTnI和NT-proBNP联合检测在急性冠状动脉综合征诊断及预后评估中的价值[J]. 检验医学与临床, 2022, 19(6): 749-754. doi: 10.3969/j.issn.1672-9455.2022.06.008
[16] Huang L, Bichsel C, Norris AL, et al. Endothelial GNAQ p. R183Q Increases ANGPT2 (Angiopoietin-2) and Drives Formation of Enlarged Blood Vessels[J]. Arterioscler Thromb Vasc Biol, 2022, 42(1): 27-43.
[17] Joussen AM, Ricci F, Paris LP, et al. Angiopoietin/Tie2 signalling and its role in retinal and choroidal vascular diseases: a review of preclinical data[J]. Eye (Lond), 2021, 35(5): 1305-1316. doi: 10.1038/s41433-020-01377-x
[18] Fleischer LT, Ballester L, Dutt M, et al. Evaluation of galectin-3 and intestinal fatty acid binding protein as serum biomarkers in autosomal recessive polycystic kidney disease[J]. J Nephrol, 2023, 36(1): 133-145.
[19] Zenger S, Demir Piroǧlu I, Çevik A, et al. The importance of serum intestinal fatty acid-binding protein for the early diagnosis of acute mesenteric ischemia[J]. Ulus Travma Acil Cerrahi Derg, 2021, 27(3): 278-283.
[20] Sekino M, Funaoka H, Sato S, et al. Intestinal fatty acid-binding protein level as a predictor of 28-day mortality and bowel ischemia in patients with septic shock: A preliminary study[J]. J Crit Care, 2017, 42(1): 92-100.
[21] Huang X, Zhou Y, Sun Y, et al. Intestinal fatty acid binding protein: A rising therapeutic target in lipid metabolism[J]. Prog Lipid Res, 2022, 87(1): 101178.
[22] Strang SG, Habes QLM, Van der Hoven B, et al. Intestinal fatty acid binding protein as a predictor for intra-abdominal pressure-related complications in patients admitted to the intensive care unit; a prospective cohort study (Ⅰ-Fabulous study)[J]. J Crit Care, 2021, 63(1): 211-217.
-




 下载:
下载: