Clinical value of atherogenic index of plasma in elevating acute ST-segment elevation myocardial infarction
-
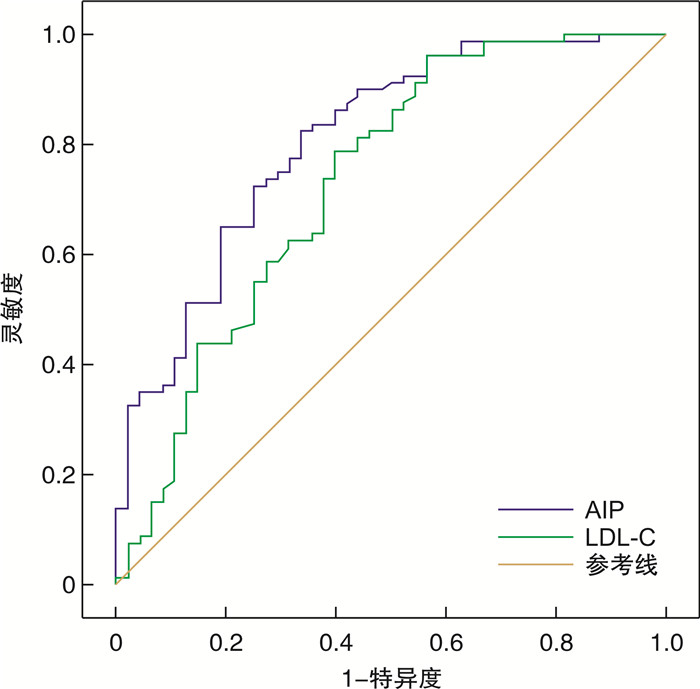
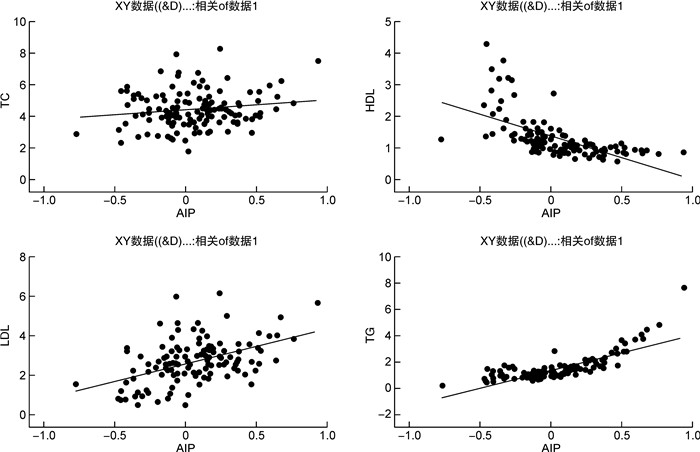
摘要: 目的 探讨血浆致动脉硬化指数(atherogenic index of plasma,AIP)预测急性ST段抬高型心肌梗死的临床价值。方法 选取我院2018年12月—2022年3月期间因胸痛、胸闷等疑诊急性心肌梗死(acute myocardial infarction,AMI)住院且行冠状动脉造影(coronary angiography,CAG)检查的患者80例为AMI组,同期因胸闷、胸痛住院,行CAG检查为正常者48例为对照组,比较两组患者的一般资料和相关实验室检查结果并计算AIP。以是否AMI为因变量,控制混杂因素吸烟史、入院时收缩压、入院时舒张压、空腹血糖、白细胞计数(WBC)、尿酸,分别以AIP为自变量进行二元logistic回归分析。结果 两组患者在吸烟比例、入院时收缩压、入院时舒张压、WBC、甘油三酯(triglyceride,TG)、高密度脂蛋白(high density lipoprotein, HDL)、低密度脂蛋白(low density lipoprotein,LDL)、空腹血糖、尿酸、AIP等方面进行比较,均差异有统计学意义(均P < 0.05)。二元logistic回归分析显示,AIP是AMI的独立预测指标;AIP预测AMI的AUC为0.81,差异有统计学意义(95%CI:0.732~0.887,P < 0.001)。最佳截断值为-0.061,并根据最大约登指数确定灵敏度为82.5%,特异度为66.7%。结论 AIP是AMI的独立危险因素,对预测AMI的发生和临床防治均有一定的指导价值。Abstract: Objective To investigate the clinical value of atherogenic index of plasma(AIP) in predicting acute ST-segment elevation myocardial infarction.Methods Eighty patients who were hospitalized for suspected acute myocardial infarction with chest pain and underwent coronary angiography(CAG) during the period from December 2018 to March 2022 were collected as the experimental group, and 48 patients who were hospitalized for chest tightness and chest and underwent CAG examination as normal during the same period were selected as the control group. The general data and relevant laboratory findings of the patients were compared and the AIP was calculate. Take whether acute myocardial infarction or not as the dependent variable, control the confounding factors, including smoking history, systolic and diastolic blood pressure at admission, fasting blood glucose, white blood cell(WBC), uric acid, and carry out binary logistic regression analysis according to the AIP as the independent variable.Results There were statistically significant differences in the proportion of patients smoking, systolic blood pressure on admission, diastolic blood pressure on admission, WBC, triglyceride(TG), high density lipoprotein(HDL), low density lipoprotein(LDL), fasting glucose, uric acid and AIP between the two groups, the differences were statistically significant(all P < 0.05). Binary logistic regression analysis showed that AIP was an independent predictor of acute myocardial infarction; The area under the curve of acute myocardial infarction predicted by AIP was 0.81(95%CI: 0.732-0.887, P < 0.001). The best cutoff value was -0.061. The sensitivity was 82.5% and the specificity was 66.7% based on the maximum Jordan index.Conclusion AIP is an independent risk factor for acute myocardial infarction and is a useful guide for predicting the occurrence of acute myocardial infarction and clinical prevention management.
-

-
表 1 一般基线资料对比
变量 AMI组(80例) 对照组(48例) χ2/t P 年龄/岁 59.35±13.82 61.83±9.89 -1.181 0.240 性别/例(%) 0.219 0.647 男 66(82.5) 38(72.9) 女 14(17.5) 10(27.1) 高血压史/例(%) 42(52.2) 27(56.3) 0.170 0.717 糖尿病病史/例(%) 13(16.3) 6(12.5) 0.334 0.563 吸烟史/例(%) 48(60.0) 15(31.3) 9.921 0.002 饮酒史/例(%) 26(32.5) 13(27.1) 0.415 0.558 入院时收缩压/mmHg 127.43±24.02 138.19±19.24 -2.637 0.009 入院时舒张压/mmHg 77.48±15.37 85.96±12.64 -3.224 0.002 BMI 25.02±3.78 25.59±3.20 -0.777 0.349 WBC/(×109/L) 9.94±3.02 6.11±1.51 8.148 < 0.001 TC/(mmol/L) 4.60±1.10 4.29±1.24 1.445 0.151 TG/(mmol/L) 1.78±1.13 1.29±0.52 2.838 0.005 HDL/(mmol/L) 1.06±0.21 1.78±0.85 -5.748 < 0.001 LDL/(mmol/L) 3.03±0.93 2.15±1.19 4.378 < 0.001 空腹血糖/(mmol/L) 7.09±3.28 5.46±1.34 3.945 < 0.001 肌酐/(μmol/L) 69.36±19.77 72.89±20.55 -0.957 0.340 尿酸/(μmol/L) 376.45±99.70 388.22±127.76 6.708 < 0.001 AIP 0.18±0.26 -0.13±0.25 6.708 < 0.001 注:1 mmHg=0.133 kPa。 表 2 二元logistic回归
变量 B SE Walds df P OR 95%CI 步骤1 AIP -6.052 1.833 10.899 1 0.001 0.002 0~0.086 入院时收缩压 0.002 0.022 0.007 1 0.931 1.002 0.959~1.046 入院时舒张压 0.087 0.043 4.045 1 0.044 1.091 1.002~1.188 吸烟(是1否0) -1.071 0.707 2.299 1 0.129 0.343 0.086~1.368 空腹血糖 -0.391 0.257 2.311 1 0.128 0.676 0.409~1.120 白细胞(0) -1.002 0.278 13.031 1 0 0.367 0.213~0.633 尿酸(1) 0.004 0.004 0.852 1 0.356 1.004 0.996~1.011 常量 1.207 3.070 0.155 1 0.694 3.343 注:在步骤1中输入的变量:AIP,入院时收缩压,入院时舒张压,吸烟是1否0,空腹血糖,白细胞0,尿酸1。 -
[1] Aryan L, Younessi D, Zargari M, et al. The Role of Estrogen Receptors in Cardiovascular Disease[J]. Int J Mol Sci, 2020, 21(12): 4314. doi: 10.3390/ijms21124314
[2] Packard C, Chapman MJ, Sibartie M, et al. Intensive low-density lipoprotein cholesterol lowering in cardiovascular disease prevention: opportunities and challenges[J]. Heart, 2021, 107(17): 1369-1375. doi: 10.1136/heartjnl-2020-318760
[3] Anderson TJ. Optimal Low-Density Lipoprotein Cholesterol for Cardiovascular Prevention: How Low Should We Go?[J]. Can J Cardiol, 2017, 33(3): 405-408. doi: 10.1016/j.cjca.2016.12.007
[4] Younis NN, Soran H, Pemberton P, et al. Small dense LDL is more susceptible to glycation than more buoyant LDL in Type 2 diabetes[J]. Clin Sci(Lond), 2013, 124(5): 343-349. doi: 10.1042/CS20120304
[5] Fernández-Macías JC, Ochoa-Martínez AC, et al. Atherogenic Index of Plasma: Novel Predictive Biomarker for Cardiovascular Illnesses[J]. Arch Med Res, 2019, 50(5): 285-294. doi: 10.1016/j.arcmed.2019.08.009
[6] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction(2018)[J]. Eur Heart J, 2019, 40(3): 237-269. doi: 10.1093/eurheartj/ehy462
[7] 李颖珂. 伊伐布雷定片对冠状动脉粥样硬化性心脏病患者经皮冠状动脉介入治疗术后心功能及血流介导性舒张功能一氧化氮内皮素水平的影响[J]. 中国药物与临床, 2021, 21(23): 3857-3860. https://www.cnki.com.cn/Article/CJFDTOTAL-YWLC202123025.htm
[8] 刘鹿, 刘英华. 高脂血症的营养干预策略[J]. 中华医学信息导报, 2021, 36(9): 11.
[9] Ivanova EA, Myasoedova VA, Melnichenko AA, et al. Small Dense Low-Density Lipoprotein as Biomarker for Atherosclerotic Diseases[J]. Oxid Med Cell Longev, 2017, 2017: 1273042.
[10] Koba S, Yokota Y, Hirano T, et al. Small LDL-cholesterol is superior to LDL-cholesterol for determining severe coronary atherosclerosis[J]. J Atheroscler Thromb, 2008, 15(5): 250-260. doi: 10.5551/jat.E572
[11] Qiao YN, Zou YL, Guo SD. Low-density lipoprotein particles in atherosclerosis[J]. Front Physiol, 2022, 13: 931931. doi: 10.3389/fphys.2022.931931
[12] 杨晓, 谢勇, 徐日新, 等. 血浆致动脉硬化指数对早发冠心病的预测作用[J]. 临床心血管病杂志, 2020, 36(11): 1000-1003. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202011007.htm
[13] 王雪华, 李红建. 血浆致动脉硬化指数的临床研究进展[J]. 中国动脉硬化杂志, 2022, 30(5): 449-453. https://www.cnki.com.cn/Article/CJFDTOTAL-KDYZ202205012.htm
[14] Si Y, Fan W, Han C, et al. Atherogenic Index of Plasma, Triglyceride-Glucose Index and Monocyte-to-Lymphocyte Ratio for Predicting Subclinical Coronary Artery Disease[J]. Am J Med Sci, 2021, 362(3): 285-290. doi: 10.1016/j.amjms.2021.05.001
[15] Niroumand S, Khajedaluee M, Khadem-Rezaiyan M, et al. Atherogenic Index of Plasma(AIP): A marker of cardiovascular disease[J]. Med J Islam Repub Iran, 2015, 29: 240.
[16] 房伟, 方艳辉, 耿巍, 等. 冠心病患者血浆致动脉硬化指数及炎症因子水平与冠状动脉钙化严重程度的相关性[J]. 中国医师杂志, 2022, 24(9): 1368-1372.
-




 下载:
下载: