The value of the ratio of neutrophil count to lymphocyte count and platelet count combined with blood lactic acid in predicting AKI in patients with multiple injuries
-
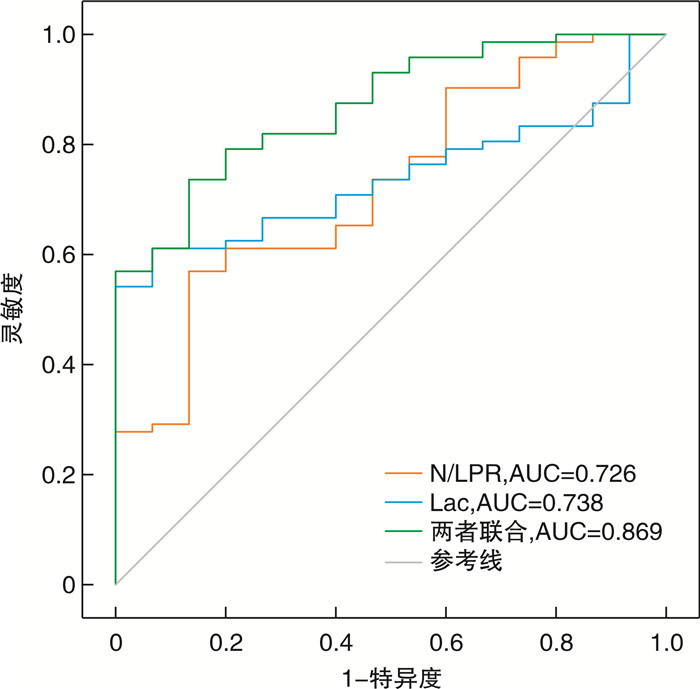
摘要: 目的 探讨中性粒细胞计数与淋巴细胞和血小板计数比值(N/LPR)联合血乳酸对多发伤患者并发急性肾功能损伤(acute kidney injury,AKI)的预测价值。方法 回顾性分析2021年2月—2023年10月南宁市第八人民医院急诊科收治的87例重型多发伤患者临床资料,根据患者住院期间是否发生AKI,分为AKI组及非AKI组,对比两组患者入院时创伤严重度评分、中性粒细胞计数、淋巴细胞计数、血小板计数、血清乳酸等指标,采用logistic回归筛选患者发生AKI的影响因素,ROC曲线分析N/LPR、血乳酸及两者联合对AKI发生的预测价值。结果 治疗前两组患者年龄、性别、合并疾病、入院白细胞计数、血红蛋白计数、血清肌酐进行比较,均差异无统计学意义(均P>0.05);AKI组ISS评分、N/LPR、血乳酸、C反应蛋白高于非AKI组,差异有统计学意义(均P < 0.05);入院平均动脉压低于非AKI组,差异有统计学意义(P < 0.05);logistics回归分析显示,N/LPR和血乳酸是多发伤患者发生AKI的独立危险因素(P < 0.05);ROC分析显示,以N/LPR>9.06判断多发伤患者发生AKI的灵敏度为86.7%,特异度为62.9%,曲线下面积为0.726;以血乳酸>2.58 mmol/L判断多发伤患者发生AKI的灵敏度为90.7%,特异度为54.2%,曲线下面积为0.738;两者联合,判断多发伤患者发生AKI的灵敏度为86.7%,特异度为73.6%,曲线下面积为0.869。结论 N/LPR和血乳酸升高是影响多发伤患者发生AKI的独立危险因素,N/LPR和血乳酸可有效预测多发伤患者并发AKI,对临床预防和治疗AKI发生具有重要临床意义。
-
关键词:
- 中性粒细胞/淋巴细胞和血小板计数比值 /
- 多发伤 /
- 急性肾损伤 /
- 预测
Abstract: Objective To investigate the value of neutrophil count to lymphocyte and platelet count ratio (N/LPR) combined with blood lactic acid in predicting acute kidney injury (AKI) in patients with multiple injuries.Methods The clinical data of 87 patients with severe multiple injuries admitted to the emergency Department of the Eighth People's Hospital of Nanning, Guangxi from February 2021 to October 2023 were retrospectively analyzed. According to whether AKI occurred during hospitalization, the patients were divided into AKI group and non-AKI group. Trauma severity score, neutrophil count, lymphocyte count, platelet count, serum lactic acid and other indicators were compared between the two groups at admission. logistic regression was used to screen the factors affecting the occurrence of AKI in patients. ROC curve was used to analyze the predictive value of N/LPR, blood lactic acid and their combination on the occurrence of AKI.Results Before treatment, there were no significant differences in age, gender, disease, white blood cell count, hemoglobin count and serum creatinine between the two groups (all P>0.05). ISS score, ratio of neutrophil count to lymphocyte and platelet count, blood lactic acid and C-reactive protein in AKI group were higher than those in non-AKI group (all P < 0.05). The mean arterial pressure on admission was lower than that in non-AKI group (P < 0.05). logistics regression analysis showed that N/LPR and blood lactic acid were independent risk factors for AKI in patients with multiple injuries (P < 0.05). ROC analysis showed that with N/LPR>9.06, the AUC of AKI occurance in patients with multiple injuries was 0.726 and the sensitivity and specificity were 86.7%, 62.9% respectively.With blood lactic acid>2.58 mmol/L, the sensitivity and specificity of AKI in patients with multiple injuries were 90.7%, 54.2%, and the AUC was 0.738. Combined both indicators, the AUC of AKI in patients with multiple injuries was 0.869 and the sensitivity and specificity were 86.7%, 73.6% respectively.Conclusion Elevated N/LPR and blood lactic acid are independent risk factors for AKI in patients with multiple injuries. N/LPR and blood lactic acid can effectively predict AKI in patients with multiple injuries, which is of great clinical significance for clinical prevention and treatment of AKI. -

-
表 1 两组患者一般资料比较
X±S 项目 AKI组(15例) 非AKI组(72例) χ2/T/U P 年龄/岁 44.85±12.55 45.67±13.41 -0.882 0.380 性别/例 1.000 男 12 54 女 3 18 糖尿病/例(%) 2(13.33) 4(7.41) 0.275 高血压病/例(%) 1(6.67) 3(4.17) 0.538 ISS评分/分 36.12±1.84 34.76±2.41 2.050 0.043 入院平均动脉压/mmHg 74.22±7.80 81.01±11.78 -2.781 0.009 入院WBC/(×109/L) 13.55±2.91 13.06±2.16 0.628 0.538 入院N/(×109/L) 14.39±2.19 13.45±1.96 1.663 0.100 入院L/(×109/L) 0.82±0.17 0.91±0.17 -1.768 0.081 入院PLT/(×109/L) 157.37±25.73 171.49±27.43 -1.831 0.071 入院Lac/(mmol/L) 3.02(2.88,3.19) 2.51(2.17,3.04) 0.004 入院N/LPR 10.72(9.39,13.62) 8.68(7.33,8.68) 0.006 入院CRP/(mg/L) 17.12±4.11 15.45±2.61 1.514 0.046 入院Hb/(g/L) 97.06±5.96 94.81±5.78 1.370 0.174 入院SCr/(mol/L) 55.63±7.46 54.08±8.77 0.636 0.527 注:1 mmHg=0.133 kPa。 表 2 AKI危险因素二元logistic回归分析
影响因素 β SE Waldχ2 EXP(B) P 95%CI 入院Lac 1.981 0.869 5.196 7.252 0.023 1.320~39.834 入院N/LPR 2.736 1.403 3.975 9.349 0.046 1.471~41.807 入院CRP 0.128 0.109 1.383 1.136 0.240 0.918~1.406 入院平均动脉压 -0.059 0.036 2.680 0.942 0.102 0.878~1.012 ISS评分 0.261 0.173 2.275 1.299 0.131 0.925~1.824 -
[1] 张翔, 袁乙铜, 何静, 等. 创伤院前救护能力现状及延时现场救护知识和能力准备-多中心横断面调研[J]. 创伤外科杂志, 2023, 25(3): 216-222. doi: 10.3969/j.issn.1009-4237.2023.03.010
[2] 中国县域创伤救治体系建设标准专家共识专家组. 中国县域创伤救治体系建设标准专家共识(2024年版)[J]. 中华骨科杂志, 2024, 44(1): 6-9. doi: 10.3760/cma.j.cn121113-20230908-00149
[3] 池锐彬, 李超锋, 邹启明, 等. 重症创伤患者急性肾损伤的临床特征及危险因素分析[J]. 中华急诊医学杂志, 2022, 31(12): 1691-1696. doi: 10.3760/cma.j.issn.1671-0282.2022.12.021
[4] 刘大东, 虞宗颖, 张德厚, 等. 外周血中性粒细胞计数与淋巴细胞和血小板计数比值对脓毒症患者28 d死亡的预测价值[J]. 中华危重病急救医学, 2021, 33(1): 33-37. doi: 10.3760/cma.j.cn121430-20200727-00545
[5] Duque-Santana V, López-Campos F, Martin-Martin M, et al. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Prognostic Factors in Locally Advanced Rectal Cancer[J]. Oncology, 2023, 101(6): 349-357. doi: 10.1159/000526450
[6] 龚春蕾, 蒋远霞, 唐艳, 等. 血乳酸升高是脓毒症相关性急性肾损伤发生及死亡的独立危险因素[J]. 中华危重病急救医学, 2022, 34(7): 714-720. doi: 10.3760/cma.j.cn121430-20210823-01238
[7] Messerer DAC, Halbgebauer R, Nilsson B, et al. Immunopathophysiology of trauma-related acute kidney injury[J]. Nat Rev Nephrol, 2021, 17(2): 91-111. doi: 10.1038/s41581-020-00344-9
[8] 中华医学会创伤学分会创伤急救与多发伤学组. 多发伤病历与诊断: 专家共识意见(2013版)[J]. 创伤外科杂志, 2014, 16(2): 192-193. https://www.cnki.com.cn/Article/CJFDTOTAL-XIBU202309002.htm
[9] Cullough PA, Shaw AD, Haase M, et al. Diagnosis of acute kidney injuryusing functional and injury biomarkers: Workgroup statements from the tenth Acute Dialysis Quality Initiative Consensus Conference[J]. Contrih Nephrol, 2013, 182: 13-29.
[10] Gameiro J, Fonseca JA, Jorge S, et al. Neutrophil, lymphocyte and platelet ratio as a predictor of mortality in septic-acute kidney injury patients[J]. Nefrologia (Engl Ed), 2020, 40(4): 461-468. doi: 10.1016/j.nefroe.2020.09.001
[11] Mortaz E, Zadian SS, Shahir M, et al. Does Neutrophil Phenotype Predict the Survival of Trauma Patients?[J]. Front Immunol, 2019, 10: 2122. doi: 10.3389/fimmu.2019.02122
[12] 晁晟, 贾磊, 熊建斌, 等. 血乳酸及乳酸清除率与多发伤失血性休克患者急性肾损伤的关系[J]. 中国老年学杂志, 2023, 43(2): 348-351. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLXZ202302026.htm
[13] Uchino S, Kellum JA, Bellomo R, et al. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Acute renal failure in critically ill patients: a multinational, multicenter study[J]. JAMA, 2005, 17, 294(7): 813-818.
[14] 孙涛, 陶志华. 急性肾损伤标志物应用价值: 现状与未来[J]. 中华检验医学杂志, 2022, 45(7): 671-676. doi: 10.3760/cma.j.cn114452-20211223-00791
[15] Dehouche N. The injury severity score: an operations perspective[J]. BMC Med Res Methodol, 2022, 22(1): 48. doi: 10.1186/s12874-022-01528-6
[16] 韩圣瑾, 周正武, 翁云龙, 等. 碳酸氢钠林格液联合连续性肾脏替代疗法对创伤合并急性肾损伤患者炎症水平及肾功能的影响[J]. 中华危重症医学杂志(电子版), 2023, 16(5): 376-381. doi: 10.3877/cma.j.issn.1674-6880.2023.05.005
[17] Leng J, Zhao W, Guo J, et al. E-prostanoid 3 receptor deficiency on myeloid cells protects against ischemic acute kidney injury via breaking the auto-amplification loop of necroinflammation[J]. Kidney Int, 2023, 103(1): 100-114. doi: 10.1016/j.kint.2022.08.019
[18] anicova A, Becker N, Xu B, et al. Severe Traumatic Injury Induces Phenotypic and Functional Changes of Neutrophils and Monocytes[J]. J Clin Med, 2021, 10(18): 4139. doi: 10.3390/jcm10184139
[19] Junger WG, Rhind SG, Rizoli SB, et al. Resuscitation of traumatic hemorrhagic shock patients with hypertonic saline-without dextran-inhibits neutrophil and endothelial cell activation[J]. Shock, 2012, 38: 341-350. doi: 10.1097/SHK.0b013e3182635aca
[20] Groeneveld KM, Koenderman L, Warren BL, et al. Early decreased neutrophil responsiveness is related to late onset sepsis in multitrauma patients: an international cohort study[J]. PLoS One, 2017, 12(6): e0180145. doi: 10.1371/journal.pone.0180145
[21] 张波, 范家伟, 康超, 等. 成年急性创伤性休克患者预后预测因素分析[J]. 中华创伤杂志, 2022, 38(4): 365-370.
[22] 郭辅政, 赵秀娟, 邓玖旭, 等. 严重创伤患者早期外周血淋巴细胞变化与预后之间的关系[J]. 北京大学学报(医学版), 2022, 54(3): 552-556. https://www.cnki.com.cn/Article/CJFDTOTAL-BYDB202203023.htm
[23] Koupenova M, Livada AC, Morrell CN. Platelet and Megakaryocyte Roles in Innate and Adaptive Immunity[J]. Circ Res, 2022, 130(2): 288-308.
-




 下载:
下载: