Predictive value of renal hemodynamic ultrasound monitoring for acute kidney injury
-
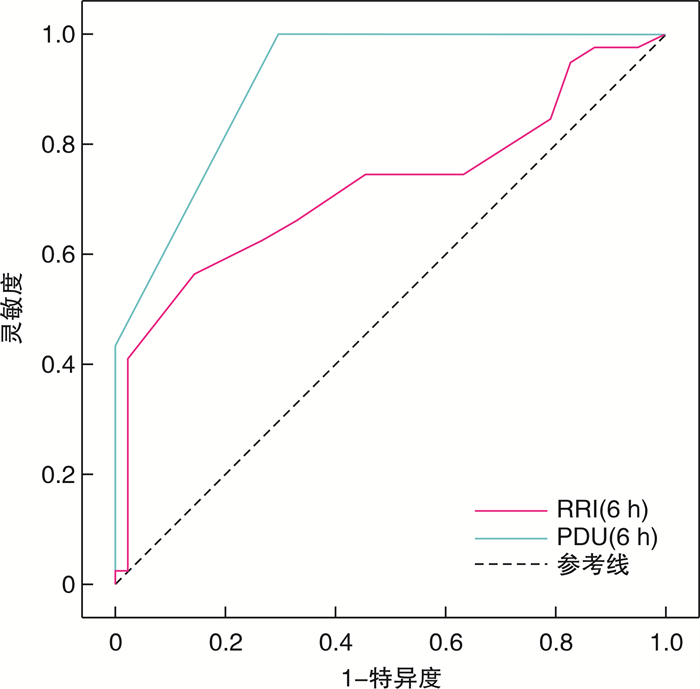
摘要: 目的 探讨肾脏血流动力学超声监测对急性肾损伤(acute kidney injury, AKI)的预测价值。方法 采用回顾性分析方法, 选取2022年8月-2023年6月入住无锡市第五人民医院重症医学科的90例AKI患者及30例肾功能正常患者为研究对象, 根据AKI程度分为肾功能正常对照组(30例)、AKI 1期组(38例)、AKI 2期组(32例)和AKI 3期组(20例)。记录患者的一般临床资料, 同时记录入科时肾脏阻力指数(renal resistive index, RRI)、能量多普勒超声(power doppler ultrasound, PDU)评分。比较各组RRI和PDU评分。将AKI患者分为短暂性AKI组(51例)和持续性AKI组(39例), 比较两组RRI和PDU评分。采用ROC曲线分析RRI和PDU评分对AKI的预测能力。结果 AKI 1~3期组的RRI高于正常对照组, 差异有统计学意义(P < 0.05);AKI 3期组RRI高于AKI 1、2期组, 差异有统计学意义(P < 0.05);AKI 1期组和正常对照组PDU评分比较差异无统计学意义(P>0.05), AKI 2期组和AKI 3期组PDU评分小于正常对照组和AKI 1期组, AKI 3期组PDU评分小于AKI 2期组, 差异有统计学意义(P < 0.05);持续性AKI组RRI高于及PDU评分低于短暂性AKI组, 差异均有统计学意义(P < 0.05);ROC曲线分析结果显示, RRI(AUC=0.724, P < 0.01)和PDU评分(AUC=0.917, P < 0.01)均可预测AKI的发生, PDU评分对AKI的预测效能要好于RRI(P < 0.05)。结论 肾脏血流动力学超声早期监测指标RRI和PDU评分对预测AKI的发生具有重要价值。Abstract: Objective To explore the predictive value of renal hemodynamic ultrasound monitoring for acute kidney injury(AKI).Methods A retrospective analysis method was used. 90 AKI patients and 30 patients with normal renal function were enrolled in this study who were admitted to the Intensive Care Unit of Wuxi Fifth People's Hospital from August 2022 to June 2023. According to the degree of AKI, they were divided into a normal renal function control group(30 cases), an AKI stage 1 group(38 cases), an AKI stage 2 group(32 cases), and an AKI stage 3 group(20 cases). Their general clinical data were recorded, and simultaneously the renal resistance index(RRI) and power Doppler ultrasound(PDU) scores were recorded at admission. The RRI and PDU scores of each group were compared. AKI patients were divided into transient AKI group(51 cases) and persistent AKI group(39 cases), and the RRI and PDU scores were compared between the two groups. The predictive ability of RRI and PDU scores on AKI was analyzed using ROC curves.Results The RRI of AKI stage 1-3 group was higher than that of the normal control group, with a statistically significant difference(P < 0.05); The RRI of AKI stage 3 group was higher than that of AKI stage 1 and stage 2 groups, with a statistically significant difference(P < 0.05); There was no difference in PDU scores between the AKI stage 1 group and the normal control group(P>0.05). The PDU scores of the AKI stage 2 and AKI stage 3 groups were lower than those of the normal control group and AKI stage 1 group, and the PDU scores of the AKI stage 3 group were lower than those of the AKI stage 2 group, with a statistically significant difference(P < 0.05); The RRI in the persistent AKI group was higher and the PDU score was lower than that in the transient AKI group, with statistical significance(P < 0.05); The ROC curve analysis results showed that both RRI(AUC=0.724, P < 0.01) and PDU score(AUC=0.917, P < 0.01) can predict the occurrence of AKI, and PDU score has a better predictive effect on AKI than RRI(P < 0.05).Conclusion Early monitoring indicators of renal hemodynamic ultrasound, RRI and PDU score, have important value in predicting the occurrence of AKI.
-
Key words:
- renal ultrasound /
- acute kidney injury /
- renal hemodynamics
-

-
表 1 KDIGO定义的AKI分期
分期 血肌酐 尿量 1期 升高至基础值的1.5~1.9倍或增加≥0.3 mg/dL(≥26.5 μmol/L) < 0.5 mL/kg/h>6 h 2期 升高至基础值的2.0~2.9倍 < 0.5 mL/kg/h>12 h 3期 升高至基础值的3倍或增加至4mg/dL或开始RRT < 0.3 mL/kg/h>24 h或无尿>12 h 表 2 PDU评分方法
评分 检查结果 0分 检测不到肾脏血流信号 1分 肾门处可见少许血流信号 2分 肾门处血流信号明显,肾皮髓交界处可见少许叶间动脉血流信号 3分 整个肾脏可见血流显像,血流信号可至弓状动脉水平 表 3 正常对照组与AKI 1~3期患者基础资料比较
资料项目 正常对照组(30例) AKI 1期组(38例) AKI 2期组(32例) AKI 3期组(20例) 年龄/[岁,M(Q25,Q75)] 76.0(60.0,80.0) 76.5(62.0,84.0) 71.5(59.0,76.0) 70.5(63.5,79.5) 性别/例(%) 女 10(33.33) 14(36.84) 7(21.88) 1(5.00) 男 20(66.67) 24(63.16) 25(78.13) 19(95.00) 高血压/例(%) 无 23(76.67) 19(50.00) 9(28.13) 0 有 7(23.33) 19(50.00) 23(71.88) 20(100.00) 糖尿病/例(%) 无 25(83.33) 30(78.95) 25(78.13) 13(65.00) 有 5(16.67) 8(21.05) 7(21.88) 7(35.00) 冠心病/例(%) 无 26(86.67) 25(65.79) 14(43.75) 8(40.00) 有 4(13.33) 13(34.21) 18(56.25) 12(60.00) APACHEⅡ评分/[分,M(Q25,Q75)] 8(7,9) 11(10,12) 14.5(13,16) 18.5(17,20) SOFA评分/[分,M(Q25,Q75)] 2(1,2) 5(4,7) 6(6,7) 11(10,12) SCr/[μmol/L,M(Q25,Q75)] 57.90
(52.20,67.20)132.60
(124.60,136.80)208.45
(197.30,225.25)341.30
(308.00,361.60)Lac/[mmol/L,M(Q25,Q75)] 1.35(0.90,1.60) 2.05(1.80,2.50) 2.20(1.70,2.50) 3.50(2.05,7.40) MAP/[mmHga),M(Q25,Q75)] 71.30(67.30,75.30) 83.15(75.50,88.40) 80.25(77.95,89.00) 88.65(74.20,94.95) 注:a)1 mmHg=0.133 kPa。 表 4 正常对照组与AKI 1~3期组患者血流动力学及实验室检查结果的比较
指标 正常对照组(30例) AKI 1期组(38例) AKI 2期组(32例) AKI 3期组(20例) H P RRI/M(Q25,Q75) 0.55
(0.52,0.57)0.77
(0.74,0.78)1)0.76
(0.73,0.77)1)0.81
(0.80,0.82)1)2)3)88.241 < 0.001 PDU评分/例(%) 1分 0(0.00) 0(0.00) 0(0.00) 17(85.00) 2分 0(0.00) 6(15.79) 28(87.50) 3(15.00) 3分 30(100.00) 32(84.21) 4(12.50) 0(0.00) PDU评分/[分,M(Q25,Q75)] 3(3,3) 3(3,3) 2(2,2)1)2) 1(1,1)1)2)3) 93.694 < 0.001 与正常对照组比较,1)P < 0.05;与AKI 1期组比较,2)P < 0.05;与AKI 2期组比较,3)P < 0.05。 表 5 短暂性AKI与持续性AKI肾血流动力学超声监测指标比较
指标 短暂性AKI(51例) 持续性AKI(39例) Z P RRI/M(Q25,Q75) 0.76(0.74,0.78) 0.79(0.75,0.81) 3.645 < 0.001 PDU评分/例(%) 1分 0(0.00) 17(43.59) 2分 15(29.41) 22(56.41) 3分 36(70.59) 0(0.00) PDU评分/[分,M(Q25,Q75)] 3(2,3) 2(1,2) -7.279 < 0.001 表 6 RRI和PDU评分对AKI发生的预测效能
指标 AUC P 截断值 灵敏度 特异度 RRI 0.724(0.611~0.838) < 0.001 0.785 0.564 0.863 PDU评分 0.917(0.875~0.960) < 0.001 2.500 1.000 0.706 -
[1] Khwaja A. KDIGO clinical practice guidelines for a-cute kidney injury[J]. Nephron Clin Pract, 2012, 120(4): 79-184.
[2] Shi HP, Xu DM, Wang GE. Prognostic indicators of patients with acute kidney injury in intensive care unit[J]. World J Emerg Med, 2010, 1(3): 209-211.
[3] Susantitaphong P, Cruz DN, Cerda J, et al. World in-cidence of AKI: a meta-analysis[J]. Clin J Am Soc Nephrol, 2013, 8(9): 1482-1493. doi: 10.2215/CJN.00710113
[4] Schneider A, Johnson L, Goodwin M, et al. Bench-to-bedside review: contrast enhanced ultrasonography-a promising technique to assess renal perfusion in the ICU[J]. Crit Care, 2011, 15(3): 157. doi: 10.1186/cc10058
[5] Yohannes S, Chawla LS. Evolving practices in the management of acute kidney injury in the ICU(Inten-sive Care Unit)[J]. Clin Nephrol, 2009, 71(6): 602-607. doi: 10.5414/CNP71602
[6] Song J, Wu W, He Y, et al. Value of the combination of renal resistance index and central venous pressure in the early prediction of sepsis-induced acute kidney injury[J]. J Crit Care, 2018, 45: 204-208. doi: 10.1016/j.jcrc.2018.03.016
[7] Schnell D, Deruddre S, Harrois A, et al. Renal resis-tive index better predicts the occurrence of acute kidney injury than cystatin C[J]. Shock, 2012, 38(6): 592-597. doi: 10.1097/SHK.0b013e318271a39c
[8] Bude RO, Rubin JM, Adler RS. Power versus conven-tional color Doppler sonography: comparison in the depiction of normal intrarenal vasculature[J]. Radiology, 1994, 192(3): 777-780. doi: 10.1148/radiology.192.3.8058946
[9] Kuwa T, Cancio LC, Sondeen JL, et al. Evaluation of renal cortical perfusion by noninvasive power Doppler ultrasound during vascular occlusion and reperfusion[J]. J Trauma, 2004, 56(3): 618-624. doi: 10.1097/01.TA.0000075331.21241.80
[10] Bagshaw SM, Langenberg C, Wan L, et al. A system-atic review of urinary findings in experimental septic acute renal failure[J]. Crit Care Med, 2007, 35(6): 1592-1598. doi: 10.1097/01.CCM.0000266684.17500.2F
[11] Zhang Z, Lu B, Sheng X, et al. Cystatin C in predic-tion of acute kidney injury: a systemic review and meta-analysis[J]. Am J Kidney Dis, 2011, 58(3): 356-365. doi: 10.1053/j.ajkd.2011.02.389
[12] Harer MW, Chock VY. Renal Tissue Oxygenation Monitoring-An Opportunity to Improve Kidney Out-comes in the Vulnerable Neonatal Population[J]. Front Pediatr, 2020, 8: 241. doi: 10.3389/fped.2020.00241
[13] Tay SY, Tiu CM, Hu B, et al. Characterization and management of various renal cystic lesions by sono-graphic features[J]. J Chin Med Assoc, 2018, 81(12): 1017-1026. doi: 10.1016/j.jcma.2018.04.008
[14] Yu A, Zhao Q, Qu Y, et al. Renal Doppler Ultrasound in the Evaluation of Renal Function in Patients with Sepsis[J]. Appl Bionics Biomech, 2022, 2022: 3472405.
[15] 万辉, 杜建文, 石秀霞, 等. 能量多普勒超声在围术期重症妊娠期高血压疾病患者急性肾损伤早期诊断的应用研究[J]. 中国妇幼保健, 2016, 31(23): 5183-5186. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201623107.htm
[16] 江锦雄, 郭黎红, 蔡承哲, 等. 肾脏彩超评价急性有机磷农药中毒并发急性肾损伤严重程度及预后的价值[J]. 中华劳动卫生职业病杂志, 2021, 39(11): 862-865. doi: 10.3760/cma.j.cn121094-20201021-00593
[17] Boddi M, Bonizzoli M, Chiostri M, et al. Renal Resis-tive Index and mortality in critical patients with acute kidney injury[J]. Eur J Clin Invest, 2016, 46(3): 242-251. doi: 10.1111/eci.12590
[18] 金仁华, 李静, 沈骁, 等. 肝素结合蛋白联合白介素-6对持续性脓毒症急性肾损伤的预测价值[J]. 临床急诊杂志, 2023, 24(3): 119-125. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.03.003
[19] 李文涛, 陈莹, 靳小静, 等. 肾阻力指数及生物标志物对脓毒症患者发生急性肾损伤的早期预测价值[J]. 临床急诊杂志, 2022, 23(3): 209-213. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.03.009
[20] 李佳, 袁野, 罗娟娟, 等. 联合肾动脉阻力指数和β2微球蛋白及降钙素原水平构建脓毒症合并急性肾损伤患者预后模型的验证评价[J]. 临床急诊杂志, 2022, 23(10): 727-732. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.10.008
[21] Oliveira RAG, Mendes PV, Park M, et al. Factors as-sociated with renal Doppler resistive index in critically ill patients: a prospective cohort study[J]. Ann Intensive Care, 2019, 9(1): 23. doi: 10.1186/s13613-019-0500-4
[22] Boddi M, Natucci F, Ciani E. The internist and the re-nal resistive index: truths and doubts[J]. Intern Emerg Med, 2015, 10(8): 893-905. doi: 10.1007/s11739-015-1289-2
[23] Andrikou I, Tsioufis C, Konstantinidis D, et al. Renal resistive index in hypertensive patients[J]. J Clin Hy-pertens, 2018, 20(12): 1739-1744. doi: 10.1111/jch.13410
-




 下载:
下载: