Predictive value of heparin-binding protein combined with interleukin-6 in different subtypes of sepsis associated acute kidney injury
-
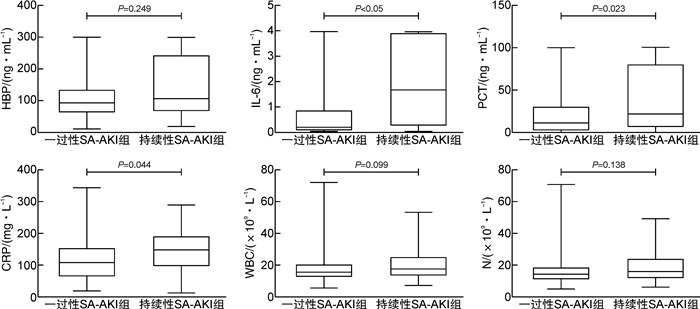
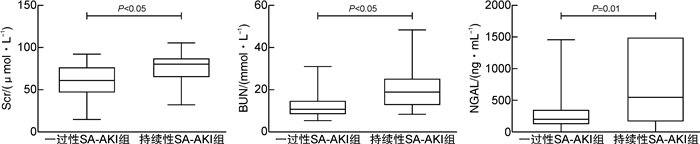
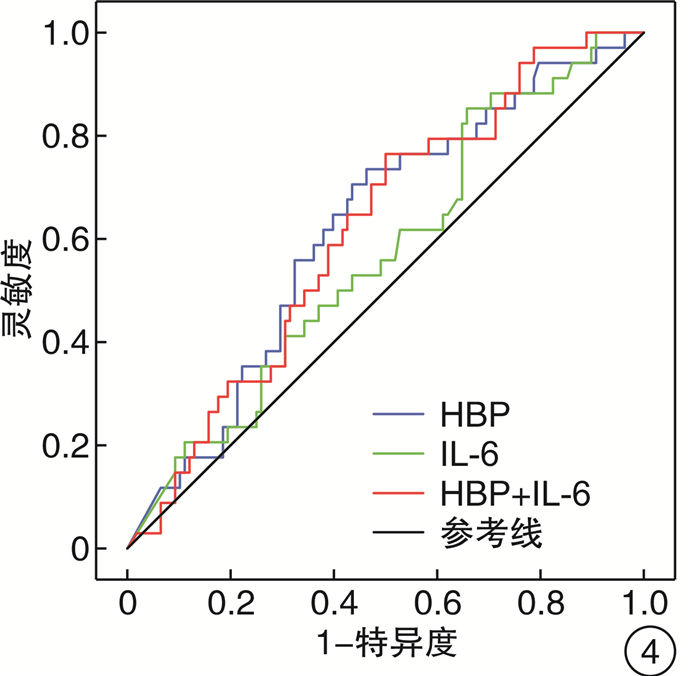
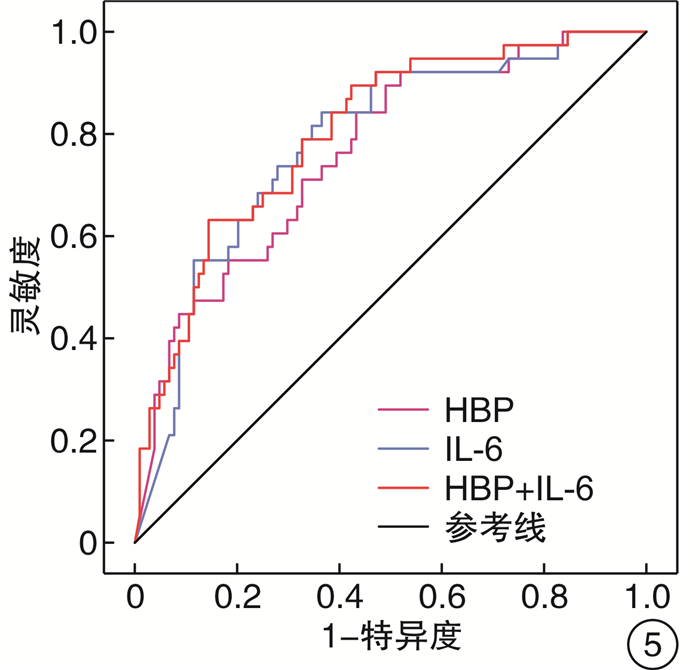
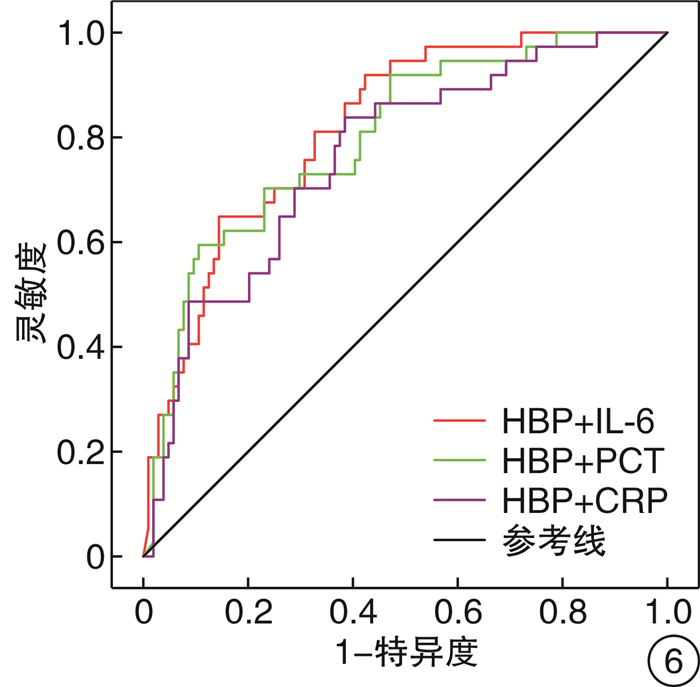
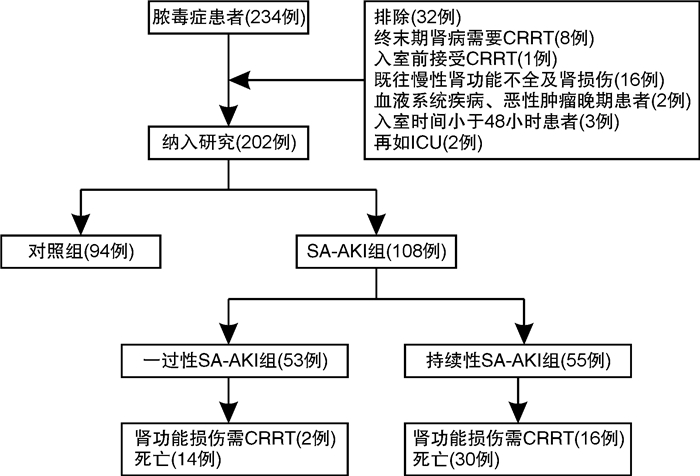
摘要: 目的 探讨肝素结合蛋白(HBP)联合白介素-6(IL-6)对持续性脓毒症急性肾损伤(SA-AKI)的预测价值。方法 回顾性选取2019年12月—2021年11月期间在南京医科大学附属南京医院重症医学科收治的符合Sepsis 3.0诊断标准的脓毒症患者,根据KIDGO标准将患者分为对照组(脓毒症无AKI组)及SA-AKI组,再根据急性疾病质量倡议(ADQI)标准将SA-AKI组患者分为一过性SA-AKI组和持续性SA-AKI组。分析比较3组患者基本临床资料以及预后情况。应用受试者工作特征(ROC)曲线分析HBP、IL-6及HBP联合IL-6对SA-AKI不同亚型尤其是持续性SA-AKI的预测价值。结果 共有202例脓毒症患者纳入分析,其中108例患者(53.4%)发生SA-AKI,53例(26.2%)为一过性SA-AKI,55例(27.2%)为持续性SA-AKI。在SA-AKI患者中,与一过性SA-AKI相比,持续性SA-AKI患者的炎症反应更重,HBP、IL-6、PCT、CRP水平更高。HBP、IL-6对持续性SA-AKI均有预测价值,ROC曲线下面积分别为0.763(95%CI:0.677~0.849)、0.782(95%CI:0.699~0.866)。HBP联合IL-6可提高对持续性SA-AKI的预测价值,ROC曲线下面积为0.801(95%CI:0.722~0.880)。结论 HBP、IL-6均对持续性SA-AKI有较高的预测价值,HBP联合IL-6可提高对持续性SA-AKI的预测价值。Abstract: Objective To investigate the predictive value of heparin-binding protein (HBP) combined with interleukin-6(IL-6) in persistent sepsis associated acute kidney injury (AKI).Methods This retrospective study enrolled adult patients with confirmed diagnostic criteria of Sepsis 3.0 and admitting to Department of Critical Care Medicine of our hospital, during the period from December 2019 to November 2021. Patients were divided into control group(sepsis without AKI) and SA-AKI group according to KIDGO criteria, and then SA-AKI group was divided into transient SA-AKI group and persistent SA-AKI group according to ADQI criteria. The baseline clinical data and prognosis of the patients were analyzed and compared. Receiver operating characteristic(ROC) curve was used to analyze the predictive value of HBP, IL-6 and HBP combined with IL-6 for different subtypes of SA-AKI.Results Of the 202 sepsis patients, 108(53.4%) developed AKI, 53(26.2%) had transient AKI, and 55(27.2%) had persistent AKI. In patients with SA-AKI, persistent SA-AKI had severer inflammatory response and higher levels of HBP, IL-6, PCT, CRP compared with transient SA-AKI. HBP and IL-6 had predictive value for persistent SA-AKI, and the area under ROC curve(AUC) was 0.763(95%CI: 0.677-0.849) and 0.782(95%CI: 0.699-0.866) respectively. HBP combined with IL-6 could improve the predictive value for persistent SA-AKI, and the AUC was 0.801(95%CI: 0.722-0.880).Conclusion HBP and IL-6 had high predictive value for persistent SA-AKI, and HBP combined with IL-6 could improve the predictive value for persistent SA-AKI.
-

-
表 1 基本临床资料
例(%),X±S,M(P25,P75) 指标 对照组(94例) 一过性SA-AKI组(53例) 持续性SA-AKI组(55例) P 一般情况 男性 56(59.6) 32(60.4) 35(63.6) 0.883 年龄/岁 72.71±14.16 71.40±13.68 75.04±13.91 0.384 BMI/(kg·m-2) 22.78±4.95 23.58±5.53 23.95±4.56 0.355 APACHE Ⅱ/分 21.15±6.96 24.40±7.63 28.58±6.89 < 0.001 SOFA/分 4(3,6) 7(6,8) 9(6,11) < 0.001 既往病史 高血压 59(62.8) 35(66.0) 37(67.3) 0.838 糖尿病 26(27.7) 16(30.2) 20(36.4) 0.537 冠心病 32(34.0) 18(34.0) 26(47.3) 0.223 房颤 13(13.8) 5(9.4) 4(7.3) 0.429 脑血管意外 35(37.2) 19(35.8) 19(34.5) 0.946 心功能不全 22(23.4) 6(11.3) 15(27.3) 0.102 炎症指标 PCT/(ng·mL-1) 0.744(0.158,2.196) 10.900(1.365,30.058) 21.595(4.910,79.510) < 0.001 HBP/(ng·mL-1) 46.47(21.81,70.83) 93.16(59.90,134.28) 105.69(63.86,244.13) < 0.001 IL-6/(ng·mL-1) 0.064(0.026,0.174) 0.191(0.059,0.865) 1.683(0.244,3.950) < 0.001 WBC/(×109·L-1) 13.06(9.59,16.36) 15.48(12.33,20.17) 17.90(13.34,25.41) < 0.001 N/(×109·L-1) 11.25(7.64,14.69) 14.45(10.87,18.52) 16.56(11.84,24.17) < 0.001 CRP/(mg·L-1) 63.92(26.30,93.90) 107.74(62.76,154.18) 148.49(95.99,191.00) < 0.001 肾功能指标 基线Scr/(μmol·L-1) 49.30(41.95,59.03) 61.00(47.05,77.65) 80.00(64.80,88.00) < 0.001 BUN/(mmol·L-1) 7.74(6.36,10.05) 10.83(8.26,14.97) 19.08(12.61,25.61) < 0.001 NGAL/(ng·mL-1) 156.40(72.00,267.97) 201.45(120.40,352.35) 551.00(165.20,1500.00) < 0.001 感染部位 肺部感染 78(83.0) 33(62.3) 22(76.4) 0.019 腹腔感染 22(23.4) 23(43.4) 11(20.0) 0.011 泌尿系感染 7(7.4) 7(13.2) 14(25.5) < 0.001 血流感染 2(2.1) 4(7.5) 8(14.5) 0.015 皮肤软组织感染 3(3.2) 3(5.7) 3(5.5) 0.713 感染性休克 6(6.4) 19(35.8) 24(43.6) < 0.001 AKI分期 < 0.001 1期 0 33(62.3) 5(9.1) 2期 0 15(28.3) 23(41.8) 3期 0 5(9.4) 27(49.1) 治疗及预后 CRRT 0 2(3.8) 16(29.1) < 0.001 ICU住院时间/d 7(4,10) 8(5,12) 9(4,18) 0.197 死亡 15(16.0) 14(26.4) 30(54.5) < 0.001 -
[1] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[2] Kellum JA, Lameire N, AKI Guideline Work Group KDIGO. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary(Part 1)[J]. Crit Care, 2013, 17(1): 204. doi: 10.1186/cc11454
[3] Bellomo R, Kellum JA, Ronco C, et al. Acute kidney injury in sepsis[J]. Intensive Care Med, 2017, 43(6): 816-828. doi: 10.1007/s00134-017-4755-7
[4] Manrique-Caballero CL, Del Rio-Pertuz G, Gomez H. Sepsis-associated acute kidney injury[J]. Crit Care Clin, 2021, 37(2): 279-301. doi: 10.1016/j.ccc.2020.11.010
[5] Forni LG, Darmon M, Ostermann M, et al. Renal recovery after acute kidney injury[J]. Intensive Care Med, 2017, 43(6): 855-866. doi: 10.1007/s00134-017-4809-x
[6] Chawla LS, Bellomo R, Bihorac A, et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative(ADQI)16 Workgroup[J]. Nat Rev Nephrol, 2017, 13(4): 241-257. doi: 10.1038/nrneph.2017.2
[7] Uhel F, Peters-Sengers H, Falahi F, et al. Mortality and host response aberrations associated with transient and persistent acute kidney injury in critically ill patients with sepsis: a prospective cohort study[J]. Intensive Care Med, 2020, 46(8): 1576-1589. doi: 10.1007/s00134-020-06119-x
[8] Peerapornratana S, Manrique-Caballero CL, Gómez H, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment[J]. Kidney Int, 2019, 96(5): 1083-1099. doi: 10.1016/j.kint.2019.05.026
[9] Pajenda S, Figurek A, Wagner L, et al. Heparin-binding protein as a novel biomarker for sepsis-related acute kidney injury[J]. PeerJ, 2020, 8: e10122. doi: 10.7717/peerj.10122
[10] 高翔, 张明, 张勇, 等. 血浆肝素结合蛋白对脓毒症相关急性肾损伤的早期诊断及预后预测[J]. 临床急诊杂志, 2021, 22(10): 647-652. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202110003.htm
[11] Fisher J, Russell JA, Bentzer P, et al. Heparin-binding protein(HBP): a causative marker and potential target for heparin treatment of human sepsis-induced acute kidney injury[J]. Shock, 2017, 48(3): 313-320. doi: 10.1097/SHK.0000000000000862
[12] Shimazui T, Nakada TA, Tateishi Y, et al. Association between serum levels of interleukin-6 on ICU admission and subsequent outcomes in critically ill patients with acute kidney injury[J]. BMC Nephrol, 2019, 20(1): 74. doi: 10.1186/s12882-019-1265-6
[13] Nagata K, Horino T, Hatakeyama Y, et al. Effects of transient acute kidney injury, persistent acute kidney injury and acute kidney disease on the long-term renal prognosis after an initial acute kidney injury event[J]. Nephrology(Carlton), 2021, 26(4): 312-318.
[14] Li QL, Zhao M, Wang XD. The impact of transient and persistent acute kidney injury on short-term outcomes in very elderly patients[J]. Clin Interv Aging, 2017, 12: 1013-1020. doi: 10.2147/CIA.S135241
[15] Ma S, Evans RG, Iguchi N, et al. Sepsis-induced acute kidney injury: a disease of the microcirculation[J]. Microcirculation, 2019, 26(2): e12483. doi: 10.1111/micc.12483
[16] Fitzgerald JC, Ross ME, Thomas NJ, et al. Association of early hypotension in pediatric sepsis with development of new or persistent acute kidney injury[J]. Pediatr Nephrol, 2021, 36(2): 451-461. doi: 10.1007/s00467-020-04704-2
[17] Lu ZQ, Li X, Yang P, et al. Heparin-binding protein enhances NF-κB pathway-mediated inflammatory gene transcription in M1 macrophages via lactate[J]. Inflammation, 2021, 44(1): 48-56. doi: 10.1007/s10753-020-01263-4
[18] Bentzer P, Fisher J, Kong HJ, et al. Heparin-binding protein is important for vascular leak in sepsis[J]. Intensive Care Med Exp, 2016, 4(1): 33. doi: 10.1186/s40635-016-0104-3
[19] Fisher J, Linder A. Heparin-binding protein: a key player in the pathophysiology of organ dysfunction in sepsis[J]. J Intern Med, 2017, 281(6): 562-574. doi: 10.1111/joim.12604
[20] Lu HY, Ning XY, Chen YQ, et al. Predictive value of serum creatinine, blood urea nitrogen, uric acid, and β2-microglobulin in the evaluation of acute kidney injury after orthotopic liver transplantation[J]. Chin Med J(Engl), 2018, 131(9): 1059-1066.
[21] Kellum JA, Romagnani P, Ashuntantang G, et al. Acute kidney injury[J]. Nat Rev Dis Primers, 2021, 7(1): 52. doi: 10.1038/s41572-021-00284-z
[22] Gaut JP, Liapis H. Acute kidney injury pathology and pathophysiology: a retrospective review[J]. Clin Kidney J, 2020, 14(2): 526-536.
[23] Darmon M, Truche AS, Abdel-Nabey M, et al. Early recognition of persistent acute kidney injury[J]. Semin Nephrol, 2019, 39(5): 431-441. doi: 10.1016/j.semnephrol.2019.06.003
[24] Wilson M, Packington R, Sewell H, et al. Biomarkers during recovery from AKI and prediction of long-term reductions in estimated GFR[J]. Am J Kidney Dis, 2022, 79(5): 646-656. e1. doi: 10.1053/j.ajkd.2021.08.017
[25] Hoste E, Bihorac A, Al-Khafaji A, et al. Identification and validation of biomarkers of persistent acute kidney injury: the RUBY study[J]. Intensive Care Med, 2020, 46(5): 943-953. doi: 10.1007/s00134-019-05919-0
-




 下载:
下载: