Analysis of risk factors for new-onset acute coronary syndrome in sepsis patients during hospitalization
-
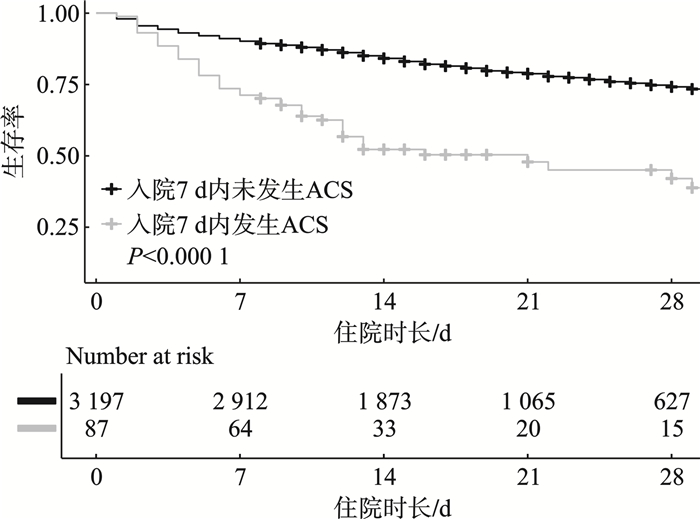
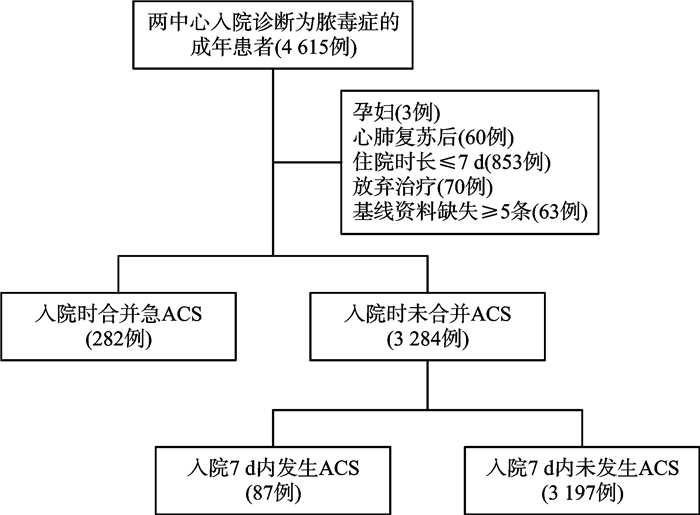
摘要: 目的 探究脓毒症患者入院后新发急性冠脉综合征(acute coronary syndrome,ACS)对短期死亡率的影响及其危险因素。方法 采用回顾性研究方法,选取2020年1月—2023年12月重庆市急救中心及2020年1月-2023年7月武汉市中心医院收治的符合Sepsis 3.0诊断标准的4 615例脓毒症患者进行分析。根据入院后7 d内是否新发急性心肌梗死(acute myocardial infarction,AMI)导致的ACS将患者分为入院后新发ACS组和未新发ACS组,比较两组患者的临床特征。对两组患者的生存水平患者进行Kaplan-Meier生存分析,使用logistic回归分析新发ACS的风险因素。结果 在入院时未合并ACS的3 284例患者中,有87例在入院后7 d内新发ACS。入院后新发ACS的脓毒症患者具有更高的28 d死亡率(19.2% vs.49.4%,P < 0.001),Kaplan-Meier生存分析显示新发ACS组具有更高的28 d死亡风险(P < 0.001)。此外,多项临床指标在两组间差异有统计学意义,包括体征:体温(中位值:36.5℃ vs.36.7℃,P=0.031),呼吸频率(中位值:22次/min vs.20次/min,P=0.02);血液生化:尿素氮(中位值:12.3 mmol/L vs. 9.3 mmol/L,P < 0.001),肌酐(中位值:150.5 μmol/L vs.95.0 μmol/L,P=0.004),肌钙蛋白(中位值:0.1 vs. 0,P < 0.001);既往病史:高血压(67.8% vs. 52.3%,P=0.039),心衰(36.8% vs.21.6%,P=0.001),ACS(19.5% vs.10.4%,P=0.006),入院时存在心肌损伤(37.9% vs.7.2%,P < 0.001);以及入院当天临床综合评分:APACHEⅡ评分(中位值:16.0分vs.13.0分,P < 0.001),SOFA评分(5.0分vs.4.0分,P=0.001)。logistic回归分析显示,入院时存在心肌损伤(OR=11.508,P < 0.001)以及既往心衰病史(OR=2.063,P=0.034)是脓毒症患者新发ACS的独立危险因素。结论 入院后新发ACS脓毒症患者具有更高的28 d死亡率,入院时存在心肌损伤以及既往心衰病史是脓毒症患者新发ACS的独立危险因素。Abstract: Objective To investigate the impact of newly developed acute coronary syndrome(ACS) on short-term mortality in septic patients, as well as risk factors of it.Methods This retrospective study was conducted from January 2020 to December 2023 in the Chongqing Emergency Medical Center, and January 2017 to July 2023 in the Wuhan Central Hospital. 4 704 septic patients who met the Sepsis 3.0 diagnostic criteria on admission were enrolled. Patients were divided into newly onset ACS group and non-ACS group based on the occurrence of newly onset ACS within 7 days after admission. Clinical characteristics of both groups were compared. Kaplan-Meier survival analysis was used to assess survival risk. logistic regression was employed to identify risk factors for newly onset ACS.Results Among 3 284 patients without ACS at admission, 87 cases developed newly onset ACS within 7 days after admission. Patients with newly onset ACS after admission had a higher 28-day mortality (19.2% vs. 49.4%, P < 0.001). Kaplan-Meier survival analysis showed a higher 28-day mortality risk in the newly onset ACS group(P < 0.001). Additionally, there were significant differences in multiple clinical indicators between the two groups, including vital signs: body temperature(median 36.5℃ vs. 36.7℃, P=0.031), respiratory rate(median 22 vs. 20, P=0.02), biochemical parameters: blood urea nitrogen(median 12.3 mmol/L vs. 9.3 mmol/L, P < 0.001), plasma creatinine(median 150.5 μmol/L vs. 95.0 μmol/L, P=0.004), plasma troponin(median 0.1 vs. 0, P < 0.001), medical history: hypertension(67.8% vs. 52.3%, P=0.039), heart failure(36.8% vs. 21.6%, P=0.001), ACS(19.5% vs. 10.4%, P=0.006). Newly onset ACS group had significantly higher myocardial injury rate at admission(37.9% vs. 7.2%, P < 0.001), and clinical scores of APACHE Ⅱ(median 16.0 vs. 13.0, P < 0.001), and SOFA(5.0 vs. 4.0, P=0.001). Logistic regression analysis indicated that myocardial injury at admission(OR=11.508, P < 0.001) and a history of heart failure(OR=2.063, P=0.034) were independent risk factors for newly onset ACS in septic patients.Conclusion Sepsis patients with newly onset ACS after admission have a higher 28-day mortality. Myocardial injury at admission and a history of heart failure are independent risk factors for newly onset ACS in these patients.
-
Key words:
- sepsis /
- acute coronary syndrome /
- acute myocardial infarction /
- risk factors
-

-
表 1 入院时合并ACS组和未合并ACS组患者临床资料比较
资料 总例数 入院时合并ACS组 入院时未合并ACS组 P 年龄/岁 75.0(65.0~85.0) 75.0(65.2~84.0) 75.0(65.0~85.0) 0.524 APACHEⅡ评分/分 14.0(10.0~18.0) 16.0(13.0~21.0) 14.0(10.0~18.0) < 0.001 SOFA评分/分 4.0(2.0~6.0) 6.0(3.2~8.0) 4.0(2.0~6.0) < 0.001 男性/% 18.4(655/3 566) 13.8(39/282) 18.8(616/3 284) 0.040 呼吸机使用率/% 10.5(376/3 566) 22.7(64/282) 9.5(312/3 284) < 0.001 升压药使用率/% 8.2(294/3 566) 21.3(60/282) 7.1(234/3 284) < 0.001 28 d病死率/% 21.1(751/3 566) 33.7(95/282) 20.0(656/3 284) < 0.001 表 2 入院后新发ACS组和未新发ACS组患者临床资料比较
资料 整体 新发ACS组 未新发ACS组 P 年龄/岁 75.0(65.0~85.0) 80.0(70.5~88.0) 75.0(65.0~85.0) 0.001 男性/% 18.8(616/3 284) 26.4(23/87) 18.5(593/3 197) 0.063 肺及胸腔疾病/% 68.8(2260/3 284) 73.6(64/87) 68.7(2 196/3 197) 0.333 消化道疾病/% 22.6(741/3 284) 18.4(16/87) 22.7(725/3 197) 0.345 泌尿系统疾病/% 17.3(567/3 284) 14.9(13/87) 17.3(554/3 197) 0.561 软组织及其他疾病/% 9.1(298/3 284) 8.0(7/87) 9.1(291/3 197) 0.735 体温/℃ 36.7(36.5~37.7) 36.5(36.5~37.0) 36.7(36.5~37.7) 0.031 心率/(次/min) 97.0(83.0~112.0) 94.0(81.5~113.0) 97.0(83.0~112.0) 0.665 呼吸频率/(次/min) 20.0(20.0~24.0) 22.0(20.0~27.0) 20.0(20.0~24.0) 0.020 平均动脉压/mmHg 89.0(75.0~99.0) 87.0(70.0~104.0) 89.0(76.0~99.0) 0.943 尿素氮/(mmol/L) 9.4(6.3~15.3) 12.3(7.8~21.5) 9.3(6.3~15.1) < 0.001 肌酐/(μmol/L) 96.0(67.0~164.0) 150.5(89.5~240.8) 95.0(66.5~162.8) 0.004 总胆红素/(μmol/L) 13.1(8.2~21.9) 11.5(6.4~19.8) 13.1(8.3~22.0) 0.334 ALT/(U/L) 21.0(13.0~41.0) 24.0(14.0~51.0) 21.0(13.0~41.0) 0.941 AST/(U/L) 30.0(19.0~55.0) 42.1(23.3~85.0) 29.2(19.0~54.5) 0.667 乳酸/(mmol/L) 2.6(1.8~3.7) 2.7(2.0~3.9) 2.6(1.8~3.7) 0.934 降钙素原/(ng/mL) 2.2(0.4~14.6) 2.2(0.7~13.2) 2.2(0.4~14.6) 0.673 CRP/(mg/L) 91.3(38.8~157.3) 106.0(44.4~142.1) 90.8(38.8~157.4) 0.682 血小板/(×109/L) 165.0(112.0~239.5) 183.0(113.5~235.5) 165.0(112.0~240.0) 0.667 纤维蛋白原/(g/L) 4.5(3.4~5.9) 4.2(3.4~5.2) 4.5(3.4~6.0) 0.097 D二聚体/(mg/L) 2.7(1.3~5.3) 2.7(1.5~6.6) 2.7(1.3~5.3) 0.225 肌钙蛋白/(μg/L) 0(0~0.1) 0.1(0~0.4) 0(0~0.1) < 0.001 高血压/% 52.7(1 732/3 284) 67.8(59/87) 52.3(1 673/3 197) 0.004 糖尿病/% 36.6(1 202/3 284) 37.9(33/87) 36.6(1 169/3 197) 0.794 房颤/% 13.3(437/3 284) 18.4(16/87) 13.2(421/3 197) 0.157 心衰/% 22.0(722/3 284) 36.8(32/87) 21.6(690/3 197) 0.001 ACS/% 10.6(349/3 284) 19.5(17/87) 10.4(332/3 197) 0.006 慢性肾病/% 12.9(422/3 284) 25.3(22/87) 12.5(400/3 197) < 0.001 脑梗死/% 25.6(840/3 284) 32.2(28/87) 25.4(812/3 197) 0.152 COPD/% 15.7(516/3 284) 12.6(11/87) 15.8(505/3 197) 0.425 心肌损伤/% 8.0(262/3 284) 37.9(33/87) 7.2(229/3 197) < 0.001 APACHEⅡ评分/分 14.0(10.0~18.0) 16.0(13.5~20.5) 13.0(10.0~18.0) < 0.001 SOFA评分/分 4.0(2.0~6.0) 5.0(3.0~7.0) 4.0(2.0~6.0) 0.001 带入呼吸机/% 312/3 284(9.5) 9/87(10.3) 303/3 197(9.5) 0.785 带入升压药/% 234/3 284(7.1) 10/87(11.5) 224/3 197(7.0) 0.108 28 d病死率/% 656/3 284(20.0) 43/87(49.4) 613/3 197(19.2) < 0.001 表 3 多因素logistic回归分析结果
因素 OR 95%CI P 年龄 1.021 0.998~1.046 0.082 性别 1.250 0.357~3.339 0.688 APACHEⅡ评分 1.025 0.975~1.076 0.316 入院肌酐 1.000 0.998~1.002 0.971 入院D-二聚体 1.003 0.968~1.015 0.786 既往心衰 2.063 1.044~4.021 0.034 既往ACS 1.097 0.500~2.300 0.811 慢性肾病 1.904 0.844~4.094 0.108 入院时存在心肌损伤 11.508 6.263~21.117 < 0.001 带入呼吸机 0.914 0.321~2.220 0.853 带入升压药 0.549 0.121~1.769 0.366 -
[1] Chiu C, Legrand M. Epidemiology of sepsis and septic shock[J]. Curr Opin Anaesthesiol, 2021, 34(2): 71-76. doi: 10.1097/ACO.0000000000000958
[2] Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the global burden of disease study[J]. Lancet, 2020, 395(10219): 200-211. doi: 10.1016/S0140-6736(19)32989-7
[3] Xie J, Wang H, Kang Y, et al. The epidemiology of sepsis in Chinese ICUs: anational cross-sectional survey[J]. Crit Care Med, 2020, 48(3): e209-e218. doi: 10.1097/CCM.0000000000004155
[4] Paraskevas T, Chourpiliadi C, Demiri S, et al. Presepsin in the diagnosis of sepsis[J]. Clin Chim Acta, 2023, 550: 117588. doi: 10.1016/j.cca.2023.117588
[5] Jacobi J. The pathophysiology of sepsis-2021 update: part 2, organ dysfunction and assessment[J]. Am J Health Syst Pharm, 2022, 79(6): 424-436. doi: 10.1093/ajhp/zxab393
[6] Bi CF, Liu J, Yang LS, et al. Research progress on the mechanism of sepsis induced myocardial injury[J]. J Inflamm Res, 2022, 15: 4275-4290. doi: 10.2147/JIR.S374117
[7] Patel N, Bajaj NS, Doshi R, et al. Cardiovascular events and hospital deaths among patients with severe sepsis[J]. Am J Cardiol, 2019, 123(9): 1406-1413. doi: 10.1016/j.amjcard.2019.01.038
[8] Bergmark BA, Mathenge N, Merlini P A, et al. Acute coronary syndromes[J]. Lancet, 2022, 399(10332): 1347-1358. doi: 10.1016/S0140-6736(21)02391-6
[9] L'Heureux M, Sternberg M, Brath L, et al. Sepsis-induced cardiomyopathy: a comprehensive review[J]. Curr Cardiol Rep, 2020, 22(5): 35. doi: 10.1007/s11886-020-01277-2
[10] 张懿, 布祖克拉·阿布都艾尼, 彭鹏. 脓毒症继发性心功能障碍动物模型的研究进展[J]. 中华危重病急救医学, 2019, 31(6): 785-788.
[11] Naghavi M, Wyde P, Litovsky S, et al. Influenza infection exerts prominent inflammatory and thrombotic effects on the atherosclerotic plaques of apolipoprotein E-deficient mice[J]. Circulation, 2003, 107(5): 762-768. doi: 10.1161/01.CIR.0000048190.68071.2B
[12] Lin YM, Lee MC, Toh HS, et al. Association of sepsis-induced cardiomyopathy and mortality: a systematic review and meta-analysis[J]. Ann Intensive Care, 2022, 12(1): 112. doi: 10.1186/s13613-022-01089-3
[13] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[14] Okisheva EA, Trushina OI. Biomarkers in acute coronary syndromes: from the origins to the present[J]. Ter Arkh, 2024, 96(9): 914-918.
[15] Geyer M, Wild J, Münzel T, et al. State of the art-high-sensitivity troponins in acute coronary syndromes[J]. Cardiol Clin, 2020, 38(4): 471-479. doi: 10.1016/j.ccl.2020.06.001
[16] Correction to: 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American heart association/American college of cardiology joint committee on clinical practice guidelines[J]. Circulation, 2023, 148(23): e186.
[17] Hollenberg SM, Singer M. Pathophysiology of sepsis-induced cardiomyopathy[J]. Nat Rev Cardiol, 2021, 18: 424-434. doi: 10.1038/s41569-020-00492-2
[18] Buffon A, Biasucci Luigi M, Liuzzo G, et al. Widespread Coronary Inflammation in Unstable Angina[J]. N Engl J Med, 347(1): 5-12.
[19] Garcia MA, Rucci JM, Thai KK, et al. Association between troponin I levels during sepsis and postsepsis cardiovascular complications[J]. Am J Respir Crit Care Med, 2021, 204(5): 557-565. doi: 10.1164/rccm.202103-0613OC
[20] 夏钰琪, 步睿, 王晓云. 心肌能量代谢与心力衰竭关系的研究进展[J]. 医学综述, 2020, 26(5): 833-838.
[21] Liu CP, Liu YJ, Chen HQ, et al. Myocardial injury: where inflammation and autophagy meet[J]. Burns Trauma, 2023, 11: tkac062. doi: 10.1093/burnst/tkac062
[22] Alkhalil M, de Maria GL, Akbar N, et al. Prospects for precision medicine in acute myocardial infarction: patient-level insights into myocardial injury and repair[J]. J Clin Med, 2023, 12(14): 4668. doi: 10.3390/jcm12144668
-

计量
- 文章访问数: 83
- 施引文献: 0



 下载:
下载: