Effect of hyperoxia exposure on in-hospital mortality and neurological outcomes in patients resuscitated from cardiac arrest
-
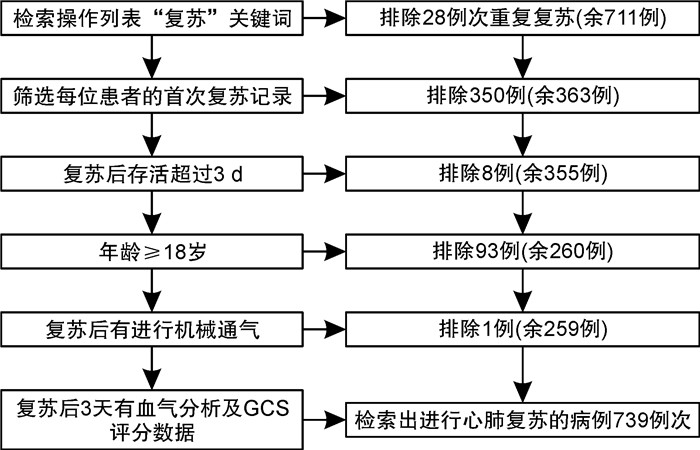
摘要: 目的 心脏骤停(cardiac arrest,CA)患者复苏后特定时间段内暴露于高氧环境可能会加重脑缺血/再灌注损伤。本文主要研究高氧暴露对CA复苏后患者院内死亡率和神经功能预后的影响。方法 本研究利用MIMIC-Ⅳ数据库检索CA复苏后患者进行回顾性队列研究,根据设定的纳入排除标准,选择复苏后进行机械通气且存活72 h以上的病例进行研究。以复苏后72 h内有无发生动脉血氧分压(PaO2)≥200 mmHg(1 mmHg=0.133 kPa)为高氧暴露临界值分为高氧暴露组和非高氧暴露组。所有CA患者复苏后均采集动脉血气分析和进行神经功能评分,有完整的神经功能预后信息。通过统计两组患者的基线资料和相关临床数据,分析复苏后早期高氧暴露对临床预后结局的影响。结果 本研究共纳入了259例CA患者,高氧暴露组170例(65.6%)和非高氧暴露组89例(34.4%)。两组患者在年龄、性别、种族及既往患有高血压、恶心肿瘤、肺部疾病等基础疾病中差异无统计学意义(P>0.05)。与非高氧暴露组相比,高氧暴露组院内死亡率显著升高(P < 0.05)。高氧暴露组患者复苏后72 h评估神经功能不良的占比明显高于非暴露组(P < 0.05)。复苏后72 h内高氧暴露是CA复苏后患者院内死亡和神经功能预后不良的独立危险因素。其OR分别为2.1(95%CI:1.1~4.0)和2.2(95%CI:1.1~4.5)。结论 ROSC后72 h内发生高氧暴露是CA患者预后不良的独立危险因素,且高氧暴露选择的最佳临界点以PaO2≥200 mmHg为宜。Abstract: Objective Exposure to hyperoxia for a specific duration following the resuscitation of cardiac arrest(CA) patients may exacerbate cerebral ischemia/reperfusion injury. This study investigates the impact of hyperoxia on in-hospital mortality and neurological outcomes in patients who have been resuscitated from cardiac arrest.Methods A retrospective cohort study was conducted using data from the MIMIC-Ⅳ database. The study included post-resuscitation CA patients who were mechanically ventilated and survived for more than 72 hours, based on predefined inclusion and exclusion criteria. Patients were divided into two groups: hyperoxia-exposed and non-hyperoxia-exposed, with hyperoxia defined as partial pressure of arterial oxygen(PaO2) ≥200 mmHg within 72 hours post-resuscitation. Arterial blood gas analysis and neurological function scores were collected for all patients with complete neurological prognostic information. The impact of early post-resuscitation hyperoxia on clinical outcomes was analyzed by comparing baseline characteristics and relevant clinical data between the two groups.Results The study included 259 CA patients, with 170(65.6%) in the hyperoxia-exposed group and 89(34.4%) in the non-hyperoxia-exposed group. No statistically significant differences were observed between the groups in terms of age, gender, race, or pre-existing conditions such as hypertension, malignancies, and lung diseases(P>0.05). In-hospital mortality was significantly higher in the hyperoxia-exposed group compared to the non-hyperoxia-exposed group(P < 0.05). Additionally, the percentage of patients with neurological dysfunction at 72 hours post-resuscitation was significantly greater in the hyperoxia-exposed group(P < 0.05). Hyperoxia exposure within 72 hours after resuscitation was identified as an independent risk factor for in-hospital mortality and poor neurological prognosis, with odd ratio of 2.1(95%CI 1.1, 4.0) and 2.2(95%CI 1.1, 4.5) respectively.Conclusion Hyperoxia exposure within 72 hours after the return of spontaneous circulation(ROSC) is an independent risk factor for adverse outcomes in CA patients. The optimal threshold for defining hyperoxia exposure is a PaO2 of ≥200 mmHg.
-

-
表 1 非高氧暴露组和高氧暴露组组间的基础数据比较
变量 非高氧暴露组(89例) 高氧暴露组(170例) P 年龄/岁 66.9±15.1 66.4±16.2 0.818 性别/例(%) 0.651 男 32(36.0) 66(38.8) 女 57(64.0) 104(61.2) 种族/例(%) 0.568 白人 61(68.5) 116(68.2) 黑人 11(12.4) 18(10.6) 亚洲人 1(1.1) 8(4.7) 西班牙人 5(5.6) 6(3.5) 不确定 11(12.4) 22(12.9) 复苏前心律/例(%) 0.743 室速/室颤 11(12.4) 21(12.4) 无脉性电活动/心室停搏 5(5.6) 14(8.2) 不确定 73(82.0) 135(79.4) 既往病史/例(%) 糖尿病 43(48.3) 63(37.1) 0.080 创伤 12(13.5) 32(18.8) 0.277 脓毒症 22(24.7) 42(24.7) 0.998 冠心病 38(42.7) 49(28.8) 0.025 高血压 30(33.7) 77(45.3) 0.072 恶性肿瘤 14(15.7) 40(23.5) 0.142 慢性肾脏疾病 10(11.2) 20(11.8) 0.900 肺部疾患 38(42.7) 59(34.7) 0.207 脑血管病 14(15.7) 26(15.3) 0.926 心衰 45(50.6) 90(52.9) 0.716 复苏72 h内GCS评分/分 10.8±4.3 9.5±4.6 0.020 72 h神经功能不良/例(%) 15(16.85) 55(32.35) 0.008 院内死亡/例(%) 18(20.2) 61(35.9) 0.009 注:以复苏后72 h内有无发生PaO2≥200 mmHg为高氧暴露临界值分为高氧暴露组及非高氧暴露组;72 h GCS评分≤6分评估患者神经功能不良。 表 2 非高氧暴露组和高氧暴露组复苏后相关临床数据比较
X±S 变量 非高氧暴露组(89例) 高氧暴露组(170例) P 初始呼吸机相关参数 机械通气平台压 21.71±6.50 20.46±5.96 0.145 呼吸机PEEP 7.1±3.6 6.3±3.0 0.060 呼吸机FIO2 64.8±25.0 68.5±27.3 0.365 血气相关参数 72 h内血气次数 8.49±6.20 12.35±7.84 < 0.001 复苏后24 h pH 7.36±0.11 7.37±0.09 0.378 复苏后24 h PO2 128.00(86.50~167.50) 119.00(92.00~169.50) 0.831 复苏后24 h PCO2 42.18±11.83 41.56±13.30 0.275 复苏后24 h BE -1.00(-5.00~1.00) -1.00(-4.00~2.00) 0.305 复苏后72 h pH 7.37±0.07 7.40±0.06 0.009 复苏后72 h PO2 96.00(73.00~114.00) 112.00(89.00~146.75) < 0.001 复苏后72 h PCO2 42.47±11.23 39.06±7.29 0.039 复苏后72 h BE 0.00(-3.00~2.00) 0.00(-2.00~2.00) 0.898 其他参数 使用血管活性药物 55(61.8) 124(72.9) 0.065 行PCI治疗 12(13.5) 14(8.2) 0.182 表 3 高氧暴露对CA患者院内死亡的多因素logistic回归分析
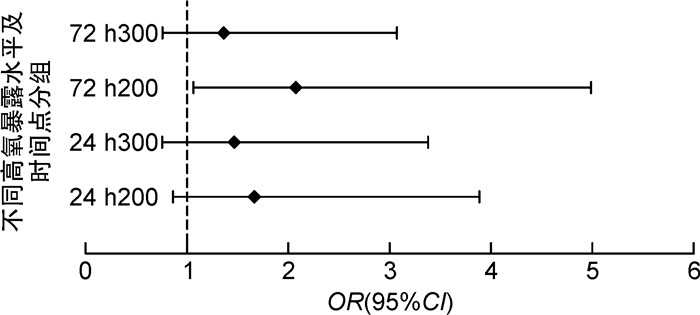
X±S 分组 未校正模型 校正模型 OR(95%CI) P OR(95%CI) P 复苏后72 h内PaO2≥300 mmHg 1.3(0.8~2.3) 0.315 1.4(0.8~2.5) 0.291 复苏后72 h内PaO2≥200 mmHg 2.2(1.2~4.0) 0.010 2.1(1.1~4.0) 0.030 复苏后24 h内PaO2≥300 mmHg 1.3(0.8~2.3) 0.326 1.5(0.8~2.7) 0.217 复苏后24 h内PaO2≥200 mmHg 1.6(0.9~2.9) 0.085 1.7(0.9~3.1) 0.108 注:校正模型为校正了性别、年龄、种族以及糖尿病、高血压、冠心病等常见病史后的logistic回归分析模型。 表 4 高氧暴露对CA患者神经功能预后不良的多因素logistic回归分析
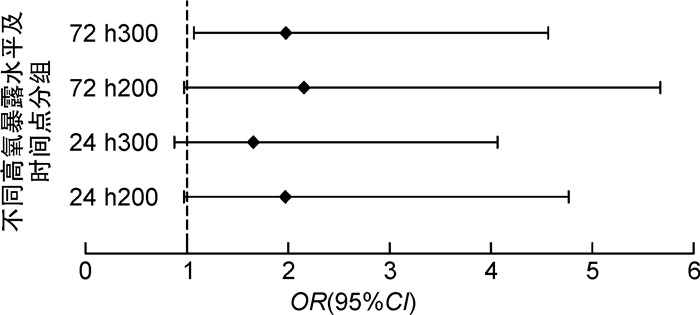
X±S 分组 未校正模型 校正模型 OR(95%CI) P OR(95%CI) P 72 h内PaO2≥300 mmHg 1.9(1.1~3.3) 0.025 2.0(1.1~3.7) 0.034 72 h内PaO2≥200 mmHg 2.4(1.2~4.5) 0.009 2.2(1.1~4.5) 0.025 24 h内PaO2≥300 mmHg 1.7(1.0~3.0) 0.072 1.7(0.9~3.3) 0.095 24 h内PaO2≥200 mmHg 1.8(1.0~3.3) 0.048 2.0(1.0~3.8) 0.049 注:神经功能预后不良以GCS≤6分为界,校正模型为校正了性别、年龄、种族以及糖尿病、高血压、冠心病等常见病史后的logistic回归分析模型。 -
[1] Hirsch KG, Abella BS, Amorim E, et al. Critical care management of patients after cardiac arrest: a scientific statement from the American heart association and neurocritical care society[J]. Circulation, 2024, 149(2): e168-e200. doi: 10.1161/CIRCULATIONAHA.123.067370
[2] 中国心脏骤停与心肺复苏报告编写组. 中国心脏骤停与心肺复苏报告(2022年版)概要[J]. 中国循环杂志, 2023, 38(10): 1005-1017. doi: 10.3969/j.issn.1000-3614.2023.10.002
[3] Penketh J, Nolan JP. Post-cardiac arrest syndrome[J]. J Neurosurg Anesthesiol, 2023, 35(3): 260-264. doi: 10.1097/ANA.0000000000000921
[4] Geocadin RG, Callaway CW, Fink EL, et al. Standards for studies of neurological prognostication in comatose survivors of cardiac arrest: a scientific statement from the American heart association[J]. Circulation, 2019, 140(9): e517-e542.
[5] Sandroni C, Cronberg T, Sekhon M. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis[J]. Intensive Care Med, 2021, 47(12): 1393-1414. doi: 10.1007/s00134-021-06548-2
[6] Awad A, Nordberg P, Jonsson M, et al. Hyperoxemia after reperfusion in cardiac arrest patients: a potential dose-response association with 30-day survival[J]. Crit Care, 2023, 27(1): 86. doi: 10.1186/s13054-023-04379-9
[7] Singer M, Young PJ, Laffey JG, et al. Dangers of hyperoxia[J]. Crit Care, 2021, 25(1): 440. doi: 10.1186/s13054-021-03815-y
[8] Nolan JP, Sandroni C, Böttiger BW, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care[J]. Intensive Care Med, 2021, 47(4): 369-421. doi: 10.1007/s00134-021-06368-4
[9] Roberts BW, Kilgannon JH, Hunter BR, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: prospective multicenter protocol-directed cohort study[J]. Circulation, 2018, 137(20): 2114-2124. doi: 10.1161/CIRCULATIONAHA.117.032054
[10] Giesa N, Heeren P, Klopfenstein S, et al. MIMIC-Ⅳ as a clinical data Schema[J]. Stud Health Technol Inform, 2022, 294: 559-560.
[11] 柯紫薇, 卢中秋. 急危重症患者高氧血症发生现状及管理策略[J]. 中国急救医学, 2020, 40(9): 909-912.
[12] Latif RK, Clifford SP, Byrne KR, et al. Hyperoxia after return of spontaneous circulation in cardiac arrest patients[J]. J Cardiothorac Vasc Anesth, 2022, 36(5): 1419-1428. doi: 10.1053/j.jvca.2021.03.007
[13] Hencz AJ, Magony A, Thomas C, et al. Short-term hyperoxia-induced functional and morphological changes in rat hippocampus[J]. Front Cell Neurosci, 2024, 18: 1376577. doi: 10.3389/fncel.2024.1376577
[14] Stoll SE, Paul E, Pilcher D, et al. Hyperoxia and mortality in conventional versus extracorporeal cardiopulmonary resuscitation[J]. J Crit Care, 2022, 69: 154001. doi: 10.1016/j.jcrc.2022.154001
[15] Bonnemain J, Rusca M, Ltaief Z, et al. Hyperoxia during extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest is associated with severe circulatory failure and increased mortality[J]. BMC Cardiovasc Disord, 2021, 21(1): 542. doi: 10.1186/s12872-021-02361-3
[16] Kobayashi M, Kashiura M, Yasuda H, et al. Hyperoxia is not associated with 30-day survival in out-of-hospital cardiac arrest patients who undergo extracorporeal cardiopulmonary resuscitation[J]. Front Med, 2022, 9: 867602. doi: 10.3389/fmed.2022.867602
[17] Barreto JA, Weiss NS, Nielsen KR, et al. Hyperoxia after pediatric cardiac arrest: association with survival and neurological outcomes[J]. Resuscitation, 2022, 171: 8-14. doi: 10.1016/j.resuscitation.2021.12.003
[18] Robba C, Badenes R, Battaglini D, et al. Oxygen targets and 6-month outcome after out of hospital cardiac arrest: a pre-planned sub-analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest(TTM2) trial[J]. Crit Care, 2022, 26(1): 323. doi: 10.1186/s13054-022-04186-8
-




 下载:
下载: