Efficacy of combined acupuncture in the treatment of in-hospital cardiac arrest: a retrospective analysis of 120 cases
-
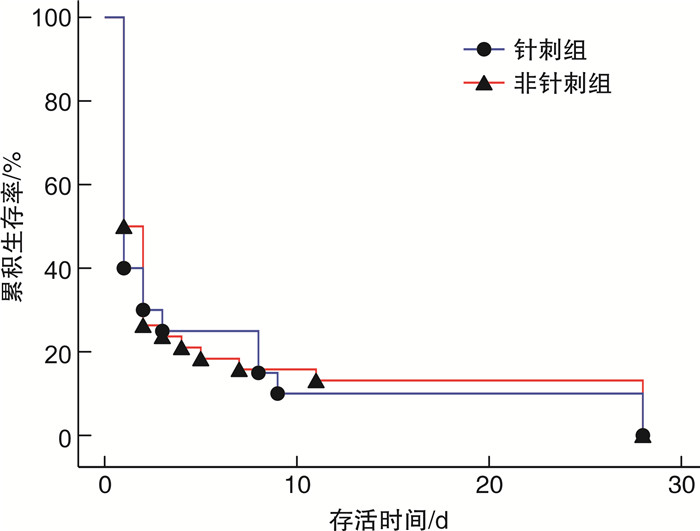
摘要: 目的 探讨联合针刺干预院内心脏骤停(in-hospital cardiac arrest,IHCA)患者临床疗效,以提供对IHCA中西医结合治疗策略的理论依据。方法 对广东省中医院急诊乌斯坦因登记模式数据库进行回顾性分析,选择2013年10月—2021年9月的IHCA为研究对象,根据纳入排除标准筛选出120例患者,根据是否进行针刺干预分为针刺组以及非针刺组。提取一般信息,基础疾病、抢救情况等,以自主循环恢复(return of spontaneous circulation,ROSC)成功率、ROSC维持时间、神经功能评价为主要指标,以实验室指标、危重症评分、28 d死亡率等为次要指标。结果 针刺组ROSC成功率为65.6%,与非针刺组(43.2%)比较,差异有统计学意义(P < 0.05)。针刺组与非针刺组ROSC维持时间方面比较[≤20 min:2例(9.5%)vs.9例(23.7%),20 min~24 h:13例(61.9%)vs.16例(42.1%),>24 h:6例(28.6%)vs.13例(34.2%)],差异无统计学意义(P>0.05)。以28 d为观察终点进行生存分析,针刺组的平均生存天数为(3.226±1.242) d(95%CI:0.791~5.661 d),非针刺组的平均生存天数为(2.352±0.692) d(95%CI:0.996~3.709 d)。Kaplan-Meier生存分析提示两组的生存曲线相同,差异无统计学意义(χ2=3.025,P=0.081)。两组各个时间点的其他指标,如血流动力学指标、血常规、血气分析、肝肾凝血功能、危重评分及器官功能支持手段等进行比较,均差异无统计学意义(均P>0.05)。结论 联合针刺救治IHCA无严重不良事件及负性结果,具有更高ROSC成功率,更稳定的ROSC比例的优势。这可能与针刺对ROSC早期的血流动力学的稳定作用有关,有一定的探索价值。Abstract: Objective To explore the clinical efficacy of combined acupuncture intervention for patients with in-hospital cardiac arrest(IHCA) to provide a theoretical basis for the integrated Chinese and Western medicine treatment strategy for IHCA.Methods A retrospective analysis was performed on the emergency Ustein registration model database of the Guangdong Provincial Hospital of Chinese Medicine. IHCA patients were selected as the research subjects from October 2013 to September 2021. According to the inclusion and exclusion criteria, 120 patients were screened and divided into an acupuncture group and a non-acupuncture group to determine whether or not acupuncture intervention was performed. General information, underlying diseases, and rescue conditions were extracted. The success rate of return of spontaneous circulation(ROSC), ROSC maintenance time, and neurological function evaluation were used as the primary outcomes. In contrast, the laboratory indicators, critical illness scores, and 28-day mortality were secondary outcomes.Results The ROSC success rate between the two groups(65.6% in the acupuncture group vs. 43.2% in the non-acupuncture group) was significantly different(P < 0.05). The comparison of ROSC maintenance time between the two groups was: ≤20 min in 2(9.5%): 9(23.7%), 20 min-24 h in 13(61.9%): 16(42.1%), and>24 h in 6(28.6%): 13(34.2%), which was not statistically significant(P>0.05). Survival analysis was performed with 28 days as the observation endpoint. The average survival days in the acupuncture group were(3.226±1.242)days(95%CI: 0.791-5.661), and the non-acupuncture group were(2.352±0.692)days(95%CI: 0.996-3.709). Kaplan-Meier survival analysis showed that the survival curves of the two groups were the same(χ2=3.025, P=0.081). There was no statistical significance in other indicators at each time point between the two groups, such as hemodynamic indicators, blood routine, blood gas analysis, liver and kidney coagulation function, critical score and organ function support measures(all P>0.05).Conclusion Combined acupuncture treatment of IHCA has no serious adverse events or negative results and has a higher ROSC success rate and a more stable ROSC ratio. This advantage may be related to the stabilizing effect of acupuncture on the hemodynamics of the early stage of ROSC, which has a specific exploration value.
-

-
表 1 病例的基线资料比较
项目 针刺组(32例) 非针刺组(88例) P 年龄/岁 42~92 22~98 0.625 男性/例(%) 20(62.5) 55(62.5) 1.000 CA到CPR时间/min 0~9 0~6 0.949 心源性CA/例(%) 8(25.0) 21(23.9) 1.000 心肌梗死 7(87.5) 20(95.2) 0.483* 其他 1(12.5) 1(4.8) 非心源性CA/例(%) 24(75.0) 67(76.1) 酸中毒 0(0.0) 3(3.7) 1.000 低氧呼衰 4(16.7) 13(19.4) 低血压休克 3(12.5) 8(11.9) 急性脑血管病 4(16.7) 2(3.0) 脓毒症 1(4.2) 5(7.5) 0.448* 复合原因 11(44.8) 30(45.8) 无法明确原因 1(4.2) 7(10.4) 基础疾病/例(%) 冠心病 10(31.3) 26(29.5) 高血压病 17(53.1) 44(50.0) 1.000 慢性心力衰竭 0(0.0) 2(2.3) 心律失常 0(0.0) 5(5.7) 1.000* 其他心脏疾病 2(6.3) 4(4.5) 0.323* 慢性阻塞性肺病 3(9.4) 9(10.2) 0.657* 哮喘 1(3.1) 2(2.3) 1.000* 脑血管疾病 7(21.9) 17(19.3) 1.000* 糖尿病 8(33.3) 23(21.1) 0.798 慢性肾病 2(6.3) 7(8.0) 1.000 慢性血液系统性疾病(非肿瘤) 1(3.1) 1(1.1) 1.000* 免疫相关性疾病 1(3.1) 3(3.4) 0.464* 肿瘤 3(9.4) 13(14.8) 1.000* 无确切病史 2(6.3) 6(6.8) 0.554* CA抢救地点/例(%) 1.000* 抢救室 8(25.0) 22(25.0) 急诊监护室 9(28.1) 39(44.3) 急诊留观室 11(34.4) 18(20.5) 住院病房 4(12.5) 7(8.0) 其他 0(0) 2(2.3) 选穴/例(%) 0.332* 内关 2(6.3) 百会 4(12.5) 足三里 6(18.8) 内关+百会 18(56.3) 不详 2(6.3) *采用Fisher确切检验法。 表 2 IHCA回顾病例的主要结果比较
X±S 项目 针刺组(32例) 非针刺组(88例) P ROSC/例(%) 21(65.6) 38(43.2) 0.039 心源性CA/例(%) 4(19.0) 12(31.6) 0.370 非心源性CA/例(%) 17(81.0) 26(68.4) 可电击心律/例(%) 7(33.3) 9(23.7) 0.543 不可电击心律/例(%) 14(66.7) 29(76.3) CPR到ROSC时间/min 24.85±11.70 23.55±15.37 0.737 ROSC维持时间/例(%) 0.284* ≤20 min 2(9.5) 9(23.7) 20 min~24 h 13(61.9) 16(42.1) >24 h 6(28.6) 13(34.2) 非死亡出院/例(%) 3(9.4) 3(3.4) 0.340* 良好神经功能出院/例(%) 1(3.1) 3(3.4) 1.000* *采用Fisher确切检验法 表 3 两组病例ROSC后次要结果比较
分组 第0天 第3天 第5天 第7天 第14天 第28天 例数 评分 例数 评分 例数 评分 例数 评分 例数 评分 例数 评分 GCS评分 针刺组 18 3~9 6 3~15 5 3~15 5 3~15 2 4~15 2 7~15 心源性CA 2 3~9 1 15 1 15 1 15 1 15 1 15 非源性CA 16 3~8 5 3~10 4 3~9 4 3~9 1 4 1 7 P 0.130 0.083 0.114 0.114 0.317 0.317 非针刺组 32 3~14 9 3~15 7 3~15 6 3~15 5 3~15 5 3~15 P 0.659 0.891 0.848 0.643 0.714 0.714 CPC评分 针刺组 18 3~4 6 1~4 5 1~4 5 1~4 2 1~4 2 1~4 心源性CA 2 3~4 1 1 1 1 1 1 1 1 1 1 非源性CA 16 3~4 5 3~4 4 4 4 4 1 4 1 4 P 0.071 0.114 0.046 0.046 0.317 0.317 非针刺组 32 1~4 9 1~4 7 1~4 6 1~4 5 1~4 5 1~4 P 0.806 0.841 0.646 0.545 1.000 1.000 表 4 两组病例ROSC后危重主分比较
分组 第0天 第3天 第5天 第7天 第14天 第28天 例数 评分 例数 评分 例数 评分 例数 评分 例数 评分 例数 评分 SOFA 针刺组 17 3~23 6 2~16 5 1~12 5 1~19 2 0~10 2 0~8 非针刺组 25 4~18 9 2~16 7 1~14 6 1~14 5 0~12 5 0~11 P 0.613 0.793 0.678 0.554 0.619 0.619 APACHEⅡ评分 针刺组 17 0~36 6 6~35 5 3~30 5 3~30 2 3~27 2 3~22 非针刺组 25 12~36 9 12~32 7 7~28 6 9~29 5 11~25 5 11~25 P 0.755 0.884 0.695 0.831 1.000 0.542 -
[1] Shao F, Li HB, Ma SK, et al. Outcomes of out-of-hospital cardiac arrest in Beijing: a 5-year cross-sectional study[J]. BMJ Open, 2021, 11(4): e041917. doi: 10.1136/bmjopen-2020-041917
[2] 中华医学会急诊医学分会, 中国医学科学院海岛急救医学创新单元(RU), 海南医学院急救与创伤研究教育部重点实验室, 等. 中国AED布局与投放专家共识[J]. 中华急诊医学杂志, 2020, 29(8): 1025-1031.
[3] Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after in-hospital cardiac arrest[J]. N Engl J Med, 2012, 367(20): 1912-1920. doi: 10.1056/NEJMoa1109148
[4] Girotra S, Spertus JA, Li Y, et al. Survival trends in pediatric in-hospital cardiac arrests: an analysis from get with the guidelines-resuscitation[J]. Circ Cardiovasc Qual Outcomes, 2013, 6(1): 42-49. doi: 10.1161/CIRCOUTCOMES.112.967968
[5] Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults[J]. JAMA, 2006, 295(1): 50-57. doi: 10.1001/jama.295.1.50
[6] 曾瑞峰, 丁邦晗, 赖芳, 等. 电针针刺足三里治疗复苏后综合征患者的临床研究[J]. 中国中医急症, 2018, 27(9): 1560-1563, 1566.
[7] Nolan JP, Sandroni C, Böttiger BW, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care[J]. Intensive Care Med, 2021, 47(4): 369-421. doi: 10.1007/s00134-021-06368-4
[8] 曾瑞峰, 钟悦嘉, 梁国荣, 等. 基于乌斯坦因模式分析150例心脏骤停患者预后的影响因素[J]. 中国急救复苏与灾害医学杂志, 2019, 14(3): 208-212.
[9] 杨晶, 段文慧, 王芳, 等. 院内心跳骤停复苏成功患者预后的预测因素分析[J]. 临床急诊杂志, 2024, 25(6): 304-309. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2024.06.006
[10] Jozwiak M, Bougouin W, Geri G, et al. Post-resuscitation shock: recent advances in pathophysiology and treatment[J]. Ann Intensive Care, 2020, 10(1): 170. doi: 10.1186/s13613-020-00788-z
[11] 曾瑞峰, 钟悦嘉, 吴炎华, 等. 电针百会穴改善心搏骤停后综合征大鼠模型的神经功能缺损及血流动力学的研究[J]. 中华危重病急救医学, 2022, 34(12): 1285-1290.
[12] Neumar RW, Nolan JP, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the international liaison committee on resuscitation(American heart association, Australian and New Zealand council on resuscitation, European resuscitation council, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation council of Asia, and the resuscitation council of southern Africa); the American heart association emergency cardiovascular care committee; the council on cardiovascular surgery and anesthesia; the council on cardiopulmonary, perioperative, and critical care; the council on clinical cardiology; and the stroke council[J]. Circulation, 2008, 118(23): 2452-2483. doi: 10.1161/CIRCULATIONAHA.108.190652
[13] 中国中西医结合学会急救医学专业委员会, 国家卫健委危重病急救医学重点实验室, 李海林, 等. 中国成人心搏骤停后综合征中西医结合诊治专家共识(2023)[J]. 中华危重病急救医学, 2023, 35(10): 1009-1025.
[14] 刘百求, 李静, 王美堂. 146例院内心搏骤停患者自主循环恢复的影响因素分析[J]. 临床急诊杂志, 2020, 21(5): 341-345. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.05.001
[15] Perman SM, Elmer J, Maciel CB, et al. 2023 American heart association focused update on adult advanced cardiovascular life support: an update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care[J]. Circulation, 2024, 149(5): e254-e273.
[16] Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care[J]. Circulation, 2020, 142(16_suppl_2): S366-S468.
[17] Burton MJ, Ramke J, Marques AP, et al. The lancet global health commission on global eye health: vision beyond 2020[J]. Lancet Glob Health, 2021, 9(4): e489-e551. doi: 10.1016/S2214-109X(20)30488-5
[18] Sun Y, Liu Y, Liu B, et al. Efficacy of acupuncture for chronic prostatitis/chronic pelvic pain syndrome: a randomized trial[J]. Ann Intern Med, 2021, 174(10): 1357-1366. doi: 10.7326/M21-1814
[19] Xu SB, Yu LL, Luo X, et al. Manual acupuncture versus sham acupuncture and usual care for prophylaxis of episodic migraine without aura: multicentre, randomised clinical trial[J]. BMJ, 2020, 368: m697.
[20] Yang JW, Wang LQ, Zou X, et al. Effect of acupuncture for postprandial distress syndrome: a randomized clinical trial[J]. Ann Intern Med, 2020, 172(12): 777-785. doi: 10.7326/M19-2880
[21] Wang YY, Liu YT, Lv QQ, et al. Effect and safety of Chinese herbal medicine granules in patients with severe coronavirus disease 2019 in Wuhan, China: a retrospective, single-center study with propensity score matching[J]. Phytomedicine, 2021, 85: 153404. doi: 10.1016/j.phymed.2020.153404
[22] Liu SQ, Yao C, Xie JF, et al. Effect of an herbal-based injection on 28-day mortality in patients with sepsis: the EXIT-SEP randomized clinical trial[J]. JAMA Intern Med, 2023, 183(7): 647-655. doi: 10.1001/jamainternmed.2023.0780
[23] Inchauspe AA. Drawing the Yongquan protocol into the different stages of the cardiopulmonary resuscitation sequence[J]. World J Crit Care Med, 2013, 2(3): 17-20.
-




 下载:
下载: