The prognostic value of neutrophil-lymphocyte ratio in patients with return of spontaneous circulation after in-hospital cardiac arrest
-
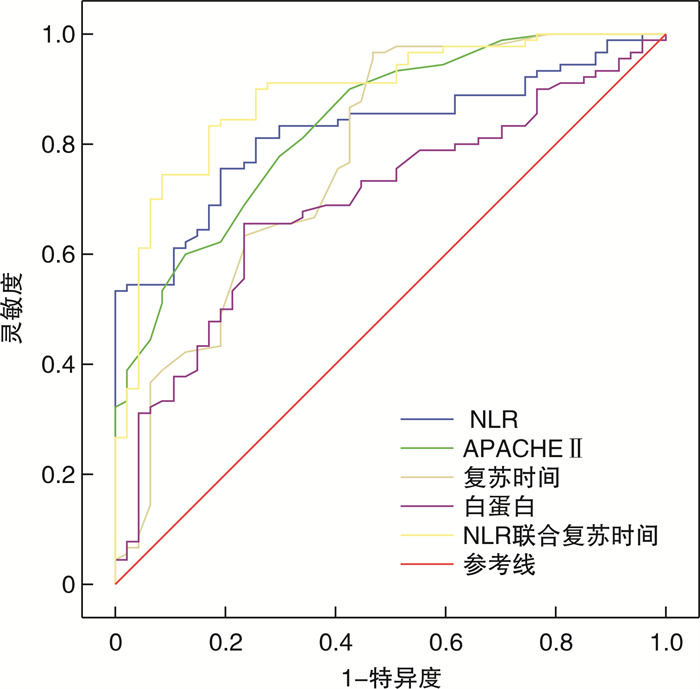
摘要: 目的 探讨中性粒细胞/淋巴细胞比值(neutrophil-lymphocyte ratio,NLR)对院内心跳骤停(in-hospital cardiac arrest,IHCA)患者恢复自主循环(return of spontaneous circulation,ROSC)不良预后的预测价值。 方法 采用回顾性分析方法,根据纳入与排除标准收集2021年10月—2023年9月收住长治市人民医院重症医学科的IHCA患者ROSC且住院≥24 h,根据最终结局分为存活组和死亡组。收集患者的一般资料、急性生理学与慢性健康状况评分Ⅱ(acute physiology and chronic health evaluation,APACHE Ⅱ)及ROSC后24 h内最初实验室指标如白细胞计数(WBC)、中性粒细胞绝对值、淋巴细胞绝对值、酸碱度(PH)、血乳酸(Lac)、白蛋白,计算NLR。比较两组指标,将有统计学意义的指标进行二元多因素logistic回归分析,绘制受试者工作曲线(ROC曲线)进一步评估NLR对疾病预后的预测价值。 结果 本研究共纳入137例,存活组47例,死亡组90例,死亡率为65.7%。两组患者年龄、性别、基础疾病、连续性肾脏替代治疗及体外膜肺氧合使用率、心源性、电除颤及肾上腺素(>5 mg)、WBC均差异无统计学意义(P>0.05)。与存活组相比,死亡组心肺复苏时间、中性粒细胞绝对值、NLR、APACHE Ⅱ、Lac明显升高,而淋巴细胞绝对值、PH、白蛋白水平明显下降,差异有统计学意义(P<0.05)。二元多因素logistic回归分析结果显示:NLR、APACHE Ⅱ、复苏时间、白蛋白均是ROSC患者预后不良的独立危险因素。ROC曲线分析显示:NLR与APACHE Ⅱ预测价值相当,其次为复苏时间、白蛋白。曲线下面积(AUC)分别为0.825、0.837、0.774、0.696,当截断值分别为6.16、24.5、18.0、31.15时灵敏度和特异度分别为80.9%和75.6%、77.8%和77.2%、96.7%和53.2%、76.6%和65.6%,且NLR联合复苏时间时AUC更高,为0.891,灵敏度和特异度分别为83.3%和83.0%。 结论 对ROSC的IHCA患者预后NLR与APACHE Ⅱ的预测价值相当,且NLR简单、经济,联合复苏时间预测价值更高,可用于临床治疗决策。
-
关键词:
- 心跳骤停 /
- 心肺复苏 /
- 自主循环恢复 /
- 中性粒细胞/淋巴细胞比值
Abstract: Objective To investigate the prognostic value of the neutrophil-lymphocyte ratio(NLR) for adverse outcomes in patients with return of spontaneous circulation(ROSC) after in-hospital cardiac arrest(IHCA). Methods A retrospective analysis was performed. The patients with ROSC after IHCA who were admitted to the Department of Critical Care, Changzhi People's Hospital and hospitalized for ≥24 hours from October 2021 to September 2023 were enrolled according to the inclusion and exclusion criteria. They were divided into survival group and death group according to the final outcome. General information, acute physiology and Chronic Health Evaluation Ⅱ (APACHE Ⅱ) and initial laboratory parameters such as white blood cell (WBC), absolute neutrophil, absolute lymphocyte, PH, blood lactic acid (Lac), albumin within 24 hours after ROSC were collected. Calculate the NLR. The two groups parameters were compared, and the statistical significance was analyzed by multivariate logistic regression. The receiver operating characteristic (ROC) curve was drawn to further evaluate the prognostic value of NLR. Results A total of 137 patients were enrolled in this study, 47 in the survival group and 90 in the death group. The mortality rate was 65.7%. There were no significant differences in age, sex, underlying diseases, CRRT, ECMO usage, cardiogenic, defibrillation, epinephrine (>5 mg) and WBC between the two groups (P>0.05). Compared those in the survival group, the time of CPR, absolute value of neutrophil, NLR, APACHE Ⅱ and Lac in the death group were significantly increased, while the absolute value of lymphocyte, PH and albumin level were significantly decreased, with significant differences (P < 0.05). Multivariate logistic regression analysis showed that NLR, APACHE Ⅱ, time of resuscitation and albumin were independent risk factors for poor prognosis of ROSC. ROC curve analysis showed that NLR had the same predictive value as APACHE Ⅱ, followed by recovery time and albumin. The area under the curve (AUC) was 0.825, 0.837, 0.774 and 0.696, respectively. When the cut-off values were 6.16, 24.5, 18.0 and 31.15, the sensitivity and specificity were 80.9% and 75.6%, 77.8% and 77.2%, 96.7% and 53.2%, 76.6% and 65.6%, respectively. When NLR combined resuscitation time, the AUC was higher (0.891) and the sensitivity and specificity were 83.3% and 83.0%, respectively. Conclusion The prognostic value of NLR in IHCA patients with ROSC is similar to that of APACHE Ⅱ, and NLR is simple, economical. When NLR combined resuscitation time, the predictive value is higher, which can be better used in clinical treatment decision. -

-
表 1 两组患者一般资料比较
变量 存活组(47例) 死亡组(90例) χ2/t P 年龄/岁 65.66±12.29 67.06±11.41 0.662 0.509 性别/例 1.189 0.276 男 28 62 女 19 28 高血压/例(%) 18(38.3) 48(53.3) 2.796 0.095 糖尿病/例(%) 12(25.5) 32(35.6) 1.423 0.233 冠心病/例(%) 13(27.7) 30(33.3) 0.462 0.497 脑血管病/例(%) 9(19.1) 24(26.7) 0.954 0.329 其他/例(%) 10(21.3) 21(23.3) 0.075 0.785 CRRT/例(%) 15(31.9) 29(32.2) 0.001 0.971 ECMO/例(%) 2(4.3) 5(5.6) 0.107 0.744 肾上腺素>5mg/例(%) 24(51.1) 60(66.7) 3.169 0.075 心源性/例(%) 8(17.0) 17(18.9) 0.072 0.788 可除颤心律/例(%) 9(19.1) 19(21.1) 0.073 0.787 复苏时间/min 23(10,28) 43(25,46) 6.267 <0.001 表 2 两组患者ROSC后24h内实验室指标比较
M(Q1,Q3) 指标 存活组(47例) 死亡组(90例) Z/t P WBC/(×109/L) 13.61(10.65,15.89) 16.39(11.13,19.57) 1.578 0.115 中性粒细胞/(×109/L) 10.09(7.35,12.81) 13.68(9.43,16.11) 2.702 0.007 淋巴细胞/(×109/L) 2.73(1.55,3.20) 1.66(0.85,2.30) 4.750 <0.001 NLR 4.40(2.59,5.82) 14.91(6.14,12.54) 6.237 <0.001 PH 7.10(6.98,7.24) 7.02(6.86,7.21) 2.171 0.030 Lac/(mmol/L) 7.78(4.94,10.60) 10.78(6.90,14.93) 2.952 0.003 白蛋白/(g/L) 33.75±5.90 29.46±7.04 3.573 <0.001 APACHE Ⅱ/分 22.14±4.58 30.63±7.49 8.225 <0.001 表 3 单因素和多因素logistic回归分析
变量 单因素logistic回归分析 多因素logistic回归分析 OR(95%CI) P OR(95%CI) P 复苏时间 1.106(1.145~1.172) 0.001 1.035(1.007~1.064) 0.013 中性粒细胞 0.925(0.718~1.191) 0.545 淋巴细胞 1.284(0.394~4.186) 0.679 NLR 1.708(1.016~2.869) 0.043 1.523(1.234~1.880) <0.001 APACHE Ⅱ 1.308(1.132~1.512) 0.000 1.305(1.143~1.490) <0.001 PH 0.207(0.010~4.133) 0.303 Lac 1.136(0.983~1.312) 0.085 白蛋白 0.885(0.802~0.976) 0.015 0.904(0.827~0.989) 0.028 表 4 NLR、APACHE Ⅱ、复苏时间、NLR联合复苏时间、白蛋白绘制的ROC曲线分析
变量 最佳截断值 AUC 95%CI P 灵敏度/% 特异度/% NLR 6.16 0.825 0.757~0.893 <0.001 80.9 75.6 APACHE Ⅱ 24.5 0.837 0.770~0.905 <0.001 77.8 77.2 复苏时间 18.0 0.774 0.687~0.862 <0.001 96.7 53.2 NLR+复苏时间 0.58 0.891 0.835~0.947 <0.001 83.3 83.0 白蛋白 31.15 0.696 0.606~0.786 <0.001 76.6 65.6 -
[1] 中华医学会急诊医学分会复苏学组, 中国医药教育协会急诊专业委员会, 成人心脏骤停后综合征诊断和治疗中国急诊专家共识组. 成人心脏骤停后综合征诊断和治疗中国急诊专家共识[J]. 中华急诊医学杂志, 2021, 30(7): 799-808. doi: 10.3760/cma.j.issn.1671-0282.2021.07.002
[2] Weiser C, Schwameis M, Sterz F, et al. Mortality in patients resuscitated from out-of-hospital cardiac arrest based on automated blood cell count and neutrophil lymphocyte ratio at admission[J]. Resuscitation, 2017, 116(1): 49-55. doi: 10.3760/cma.j.issn.1673-4378.2017.01.011
[3] Feng XF, Hai JJ, Ma Y, et al. Sudden Cardiac Death in Mainland China: A Systematic Analysis[J]. Circ Arrhythm Electrophysiol, 2018, 11(11): e006684. doi: 10.1161/CIRCEP.118.006684
[4] Seppä A, Skrifvars MB, Pekkarinen PT. Inflammatory response after out-of-hospital cardiac arrest-Impact on outcome and organ failure development[J]. Acta Anaesthesiol Scand, 2023, 67(9): 1273-1287. doi: 10.1111/aas.14291
[5] Tangjitgamol S, Udayachalerm W, Wanishsawad C, et al. Association of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio and Coronary Artery Disease Among the Physicians[J]. J Inflamm Res, 2024, 17: 59-66. doi: 10.2147/JIR.S447750
[6] Chang CJ, Liou TH, Tsai WT, et al. Clinical and Hematological Predictors for Return of Spontaneous Circulation in Patients With Out-of-Hospital Cardiac Arrest[J]. J Acute Med, 2020, 10(2): 51-59.
[7] Perman SM, Elmer J, Maciel CB, et al. 2023 American Heart Association Focused Update on Adult Advanced Cardiovascular Life Support: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care[J]. Circulation, 2024, 149(5): e254-e273.
[8] 曾琴兵, 晁彦公, 陈晓杰, 等. 肺部超声联合NLR及D-二聚体对医院获得性肺炎疗效及预后的评估价值[J]. 临床急诊杂志, 2023, 24(3): 105-111. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.03.001
[9] Martins EC, Silveira L, Viegas K, et al. Neutrophil-lymphocyte ratio in the early diagnosis of sepsis in an intensive care unit: a case-control study[J]. Rev Bras Ter Intensiva, 2019, 31(1): 64-70.
[10] 刘佳琪, 侯志刚, 米玉霞, 等. 血清hs-CRP和NLR与急性脑梗死患者依达拉奉右莰醇治疗效果的相关性[J]. 临床急诊杂志, 2023, 24(4): 179-184. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.04.002
[11] Han SI, Cha KC, Roh YI, et al. Association between Novel Marker(Platelet-Lymphocyte Ratio, Neutrophil-Lymphocyte Ratio, and Delta Neutrophil Index)and Outcomes in Sudden Cardiac Arrest Patients[J]. Emerg Med Int, 2021, 2021: 6650958.
[12] Patel VH, Vendittelli P, Garg R, et al. Neutrophil-lymphocyte ratio: A prognostic tool in patients with in-hospital cardiac arrest[J]. World J Crit Care Med, 2019, 8(2): 9-17. doi: 10.5492/wjccm.v8.i2.9
[13] Huang YH, Lin YS, Wu CH, et al. Prognostic value of neutrophil-lymphocyte ratio in out-of-hospital cardiac arrest patients receiving targeted temperature management: An observational cohort study[J]. J Formos Med Assoc, 2023, 122(9): 890-898. doi: 10.1016/j.jfma.2023.01.005
[14] Kim S, Yang H, Rhee B, et al. Predicting Survival Outcomes in Post-Cardiac Arrest Syndrome: The Impact of Combined Sequential Organ Failure Assessment Score and Serum Lactate Measurement[J]. Med Sci Monit, 2023, 29: e942119.
[15] Isenschmid C, Kalt J, Gamp M, et al. Routine blood markers from different biological pathways improve early risk stratification in cardiac arrest patients: Results from the prospective, observational COMMUNICATE study[J]. Resuscitation, 2018, 130: 138-145. doi: 10.1016/j.resuscitation.2018.07.021
[16] Toftgaard Pedersen A, Kjaergaard J, Hassager C, et al. Association between inflammatory markers and survival in comatose, resuscitated out-of-hospital cardiac arrest patients[J]. Scand Cardiovasc J, 2022, 56(1): 85-90. doi: 10.1080/14017431.2022.2074093
[17] Dölling M, Eckstein M, Singh J, et al. Hypoxia Promotes Neutrophil Survival After Acute Myocardial Infarction[J]. Front Immunol, 2022, 13: 726153.
[18] Wada T. Coagulofibrinolytic Changes in Patients with Post-cardiac Arrest Syndrome[J]. Front Med(Lausanne), 2017, 4: 156.
[19] Taha-Sert E, Kokulu K, Mutlu H, et al. Performance of the systemic immune-inflammation index in predicting survival to discharge in out-of-hospital cardiac arrest[J]. Resusc Plus, 2023, 14: 100382.
[20] Miyazaki Y, Hayashida K, Ikeda K, et al. Inhaled nitric oxide improves post-cardiac arrest outcomes via guanylate cyclase-1 in bone marrow-derived cells[J]. Nitric Oxide, 2022, 125-126: 47-56.
[21] 王宏, 兰超, 罗垚, 等. 血红蛋白与红细胞分布宽度比值对院外心搏骤停心肺复苏后患者预后的预测价值[J]. 中华危重病急救医学, 2023, 35(9): 958-962.
[22] 刘畅, 王金龙, 仲轶, 等. 高敏C反应蛋白与血清白蛋白比值对院内心脏骤停患者预后的预测价值[J]. 中华急诊医学杂志, 2021, 30(8): 1002-1006.
-

计量
- 文章访问数: 60
- 施引文献: 0



 下载:
下载: