Integration of heparin-binding protein and interleukin-6 in the early prediction of mortality in sepsis
-
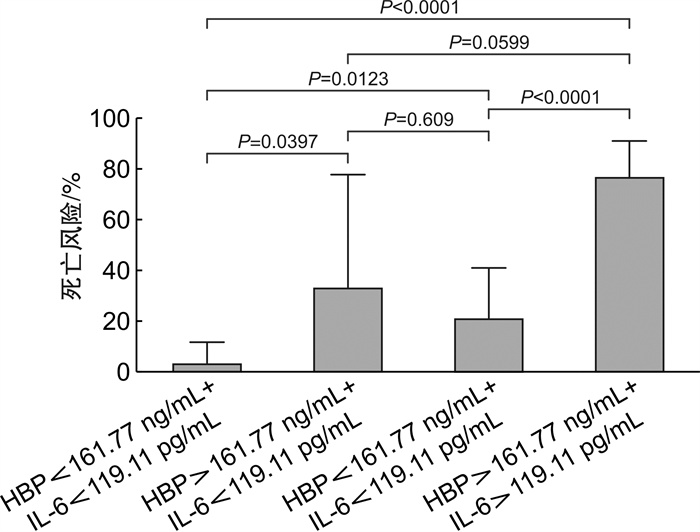
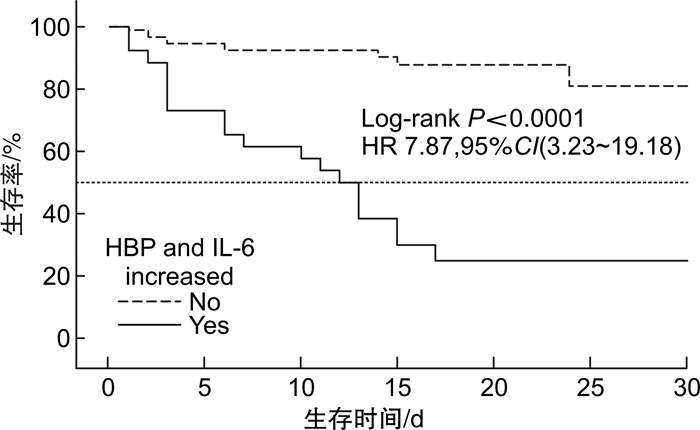
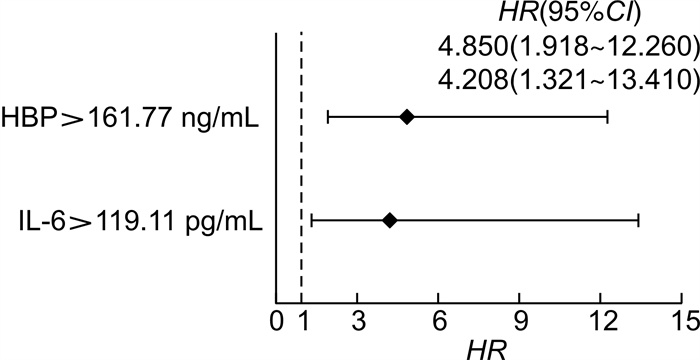
摘要: 目的 探讨肝素结合蛋白(heparin-binding protein,HBP)联合白细胞介素-6(interleukin-6,IL-6)对脓毒症预后的预测价值。 方法 采用回顾性研究方法,选取2021年9月—2023年5月期间南京医科大学附属淮安第一医院急诊医学科收治的符合Sepsis 3.0诊断标准的119例脓毒症患者,根据患者预后分为生存组和死亡组。分析比较两组患者临床资料,采用多因素Cox回归分析HBP、IL-6对患者预后的影响,绘制森林图比较患者预后的独立危险因素差异。对不同HBP、IL-6水平患者进行Kaplan-Meier(K-M)生存分析。 结果 与生存组相比,死亡组患者HBP、IL-6水平明显升高。Cox回归分析显示HBP>161.77 ng/mL(HR=4.850,95%CI:1.918~12.260,P<0.001)、IL-6>119.11 pg/mL(HR=4.208,95%CI:1.321~13.410,P=0.015)是患者住院死亡的独立危险因素。K-M生存分析显示当HBP>161.77 ng/mL且IL-6>119.11 pg/mL时,患者住院死亡风险升高,差异有统计学意义(HR=7.87,95%CI:3.23~19.18,P<0.000 1)。HBP联合IL-6预测脓毒症预后的灵敏度为66.7%,特异度为93.3%,阳性预测值为77.1%,阴性预测值为89.3%,阳性似然比为9.96,阴性似然比为0.36。 结论 HBP和IL-6是脓毒症预后的独立危险因素,两者联合对脓毒症预后有较好的预测价值。Abstract: Objective To investigate the predictive value of heparin-binding protein(HBP)and interleukin-6(IL-6)in sepsis. Methods A total of 119 adult patients with sepsis were enrolled in this retrospective study who admitted to Department of Emergency Medicine of the Affiliated Huaian No.1 People's Hospital of Nanjing Medical University from September 2021 to May 2023. They were divided into survival group and death group according to survival status. HBP, IL-6 and other clinical data of two groups were analyzed and compared. Multivariate Cox regression were used to analyze the influence of HBP and IL-6 on prognosis, and forest plots were drawn to compare the independent prognostic factors. Kaplan-Meier(K-M)survival analysis was performed for patients. Results The HBP and IL-6 of the death group was significantly higher than those of the survival group(P < 0.05). Cox regression analysis evidenced admission HBP more than 161.77 ng/mL(HR=4.850, 95%CI: 1.918-12.260, P < 0.001) and IL-6 more than 119.11 pg/mL(HR=4.208, 95%CI: 1.321-13.410, P=0.015) as independent risk factors for hospitalization motality of patients with sepsis. K-M survival analysis showed that hospitalization motality risk of patients with HBP>161.77 ng/mL and IL-6>119.11 pg/mL was higher(HR: 7.87, 95%CI: 3.23-19.18, P < 0.000 1). Integration of HBP and IL-6 prognosticated mortality with sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio and negative likelihood ratio 66.7%, 93.3%, 77.1%, 89.3%, 9.96, 0.36, respectively. Conclusion The levels of HBP and IL-6 are independent risk factors for sepsis patients. And the integration of the two had good predictive value for prognosis of sepsis patients.
-
Key words:
- heparin-binding protein /
- interleukin-6 /
- sepsis /
- prognosis
-

-
表 1 两组患者临床资料比较
X±S,M(Q1,Q3) 临床资料 生存组(89例) 死亡组(30例) t/z/χ2 P 一般情况 年龄/岁 66.3±13.6 65.5±15.0 0.292 0.771 男性/例(%) 47(52.8) 17(56.7) 0.134 0.714 SOFA/分 7.7±3.3 9.5±3.6 -2.604 0.010 APACHE Ⅱ/分 14.9±6.4 19.0±6.9 -2.921 0.004 基础疾病史/例(%) 高血压病 49(55.1) 14(46.7) 0.634 0.426 糖尿病 36(40.4) 9(30.0) 1.042 0.307 冠心病 11(12.4) 5(16.7) 0.083 0.773 脑血管意外 13(14.6) 3(10.0) 0.109 0.741 心功能不全 5(5.6) 2(6.7) <0.001 >0.999 炎症指标 HBP/(ng/mL) 101.46(67.34,135.98) 231.90(134.31,266.81) -5.374 <0.001 IL-6/(pg/mL) 111.00(38.55,176.96) 265.22(144.61,1347.85) -5.143 <0.001 WBC/(×109/L) 15.20(9.51,23.24) 16.34(7.75,26.92) -0.572 0.567 CRP/(mg/L) 161.00(104.75,196.00) 148.00(94.53,190.01) -0.695 0.487 PCT/(ng/mL) 18.17(1.55,43.90) 39.77(7.00,82.08) -1.971 0.050 感染灶/例(%) 肺部 14(15.7) 14(46.7) 11.934 0.001 泌尿系 42(47.2) 4(13.3) 10.847 0.001 肝胆系 13(14.6) 5(16.7) <0.001 >0.999 消化系 8(9.0) 1(3.3) <0.001 >0.999 腹腔 6(6.7) 2(6.7) 0.377 0.539 皮肤软组织 5(5.6) 3(10.0) 0.166 0.684 致病菌/例(%) 革兰阳性菌 8(9.0) 7(23.3) 2.990 0.084 革兰阴性菌 37(41.6) 13(43.3) 0.029 0.866 真菌 8(9.0) 11(36.7) 10.831 0.001 细菌合并真菌 6(6.7) 5(16.7) 1.584 0.208 不明确 38(46.7) 6(20.0) 4.960 0.026 脓毒性休克 48(53.9) 18(60.0) 0.334 0.563 AKI 19(21.3) 15(50.0) 9.025 0.003 呼吸衰竭 11(12.4) 13(43.3) 13.369 <0.001 治疗情况 CRRT/例(%) 8(9.0) 10(33.3) 8.548 0.003 收住EICU/例(%) 62(69.7) 26(86.7) 3.367 0.066 EICU住院时间/d 5(3,11) 6(3,11) -0.405 0.591 总住院时间/d 14(11,20) 6(3,14) -4.074 0.007 表 2 患者住院死亡风险多因素Cox回归分析
指标 β SE Z P HR 95%CI 女性 0.374 0.390 0.959 0.337 1.454 0.677~3.125 年龄 0.001 0.011 0.078 0.938 1.001 0.980~1.022 HBP>161.77 ng/mL 1.579 0.473 3.337 0.000 4.850 1.918~12.260 IL-6>119.11 pg/mL 1.437 0.591 2.430 0.015 4.208 1.321~13.410 SOFA评分1) 0.229 0.097 2.360 0.018 1.258 1.040~1.522 APACHE Ⅱ评分 0.071 0.031 2.311 0.021 1.073 1.011~1.139 1)HR=Exp[0.229-0.024t(d)]。 表 3 HBP联合IL-6对脓毒症预后的预测价值
指标 灵敏度/% 特异度/% 阳性预测值/% 阴性预测值/% 阳性似然比 阴性似然比 HBP>161.77 ng/mL 73.3 88.8 68.8 90.8 6.54 0.30 IL-6>119.11 pg/mL 86.7 68.5 48.0 93.8 2.75 0.19 HBP+IL-6 66.7 93.3 77.1 89.3 9.96 0.36 -
[1] Weng L, Xu Y, Yin P, et al. National incidence and mortality of hospitalized sepsis in China[J]. Crit Care, 2023, 27(1): 84. doi: 10.1186/s13054-023-04385-x
[2] Xie J, Wang H, Kang Y, et al. The Epidemiology of Sepsis in Chinese ICUs: A National Cross-Sectional Survey[J]. Crit Care Med, 2020, 48(3): e209-e218. doi: 10.1097/CCM.0000000000004155
[3] Wu YL, Yo CH, Hsu WT, et al. Accuracy of Heparin-Binding Protein in Diagnosing Sepsis: A Systematic Review and Meta-Analysis[J]. Crit Care Med, 2021, 49(1): e80-e90. doi: 10.1097/CCM.0000000000004738
[4] Póvoa P, Coelho L, Dal-Pizzol F, et al. How to use biomarkers of infection or sepsis at the bedside: guide to clinicians[J]. Intensive Care Med, 2023, 49(2): 142-153. doi: 10.1007/s00134-022-06956-y
[5] Fisher J, Linder A. Heparin-binding protein: a key player in the pathophysiology of organ dysfunction in sepsis[J]. J Intern Med, 2017, 281(6): 562-574. doi: 10.1111/joim.12604
[6] Othman A, Sekheri M, Filep JG. Roles of neutrophil granule proteins in orchestrating inflammation and immunity[J]. FEBS J, 2022, 289(14): 3932-3953. doi: 10.1111/febs.15803
[7] 金仁华, 李静, 沈骁, 等. 肝素结合蛋白联合白介素-6对持续性脓毒症急性肾损伤的预测价值[J]. 临床急诊杂志, 2023, 24(3): 119-125. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.03.003
[8] Katsaros K, Renieris G, Safarika A, et al. Heparin binding protein for the early diagnosis and prognosis of sepsis in the emergency department: the prompt multicenter study[J]. Shock, 2022, 57(4): 518-525. doi: 10.1097/SHK.0000000000001900
[9] Jarczak D, Kluge S, Nierhaus A. Sepsis-Pathophysiology and Therapeutic Concepts[J]. Front Med(Lausanne), 2021, 8: 628302.
[10] Kang S, Kishimoto T. Interplay between interleukin-6 signaling and the vascular endothelium in cytokine storms[J]. Exp Mol Med, 2021, 53(7): 1116-1123. doi: 10.1038/s12276-021-00649-0
[11] 周思颖, 顾国嵘, 慕婉晴, 等. 细胞因子、经皮氧分压/吸入氧浓度联合危重评分对脓毒症患者进展为脓毒性休克及预后的预测价值[J]. 中国临床医学, 2023, 30(3): 426-431. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX202303006.htm
[12] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[13] Kellum JA, Lameire N, KDIGO AKI Guideline Work Group, et al. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary(Part 1)[J]. Crit Care, 2013, 17(1): 204. doi: 10.1186/cc11454
[14] Saridaki M, Metallidis S, Grigoropoulou S, et al. Integration of heparin-binding protein and interleukin-6 in the early prediction of respiratory failure and mortality in pneumonia by SARS-CoV-2(COVID-19)[J]. Eur J Clin Microbiol Infect Dis, 2021, 40(7): 1405-1412. doi: 10.1007/s10096-020-04145-7
[15] Vincent JL, Sakr Y, Singer M, et al. Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017[J]. JAMA, 2020, 323(15): 1478-1487. doi: 10.1001/jama.2020.2717
[16] 陈雅, 金琪, 陈琪, 等. 老年脓毒症患者细胞因子谱及病情程度的差异性研究[J]. 中国临床药理学杂志, 2022, 38(18): 2128-2132. https://www.cnki.com.cn/Article/CJFDTOTAL-GLYZ202218004.htm
[17] 陈东方, 郑海, 刘树峰, 等. 不同细菌感染引起的脓毒血症患者炎症因子水平[J]. 中华医院感染学杂志, 2022, 32(3): 351-355. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202203007.htm
[18] Tang A, Shi Y, Dong Q, et al. Prognostic differences in sepsis caused by gram-negative bacteria and gram-positive bacteria: a systematic review and meta-analysis[J]. Crit Care, 2023, 27(1): 467. doi: 10.1186/s13054-023-04750-w
[19] Liu D, Huang SY, Sun JH, et al. Sepsis-induced immunosuppression: mechanisms, diagnosis and current treatment options[J]. Mil Med Res, 2022, 9(1): 56.
[20] 刘岩, 高翔, 朱玉琴, 等. 早期动态监测肝素结合蛋白对老年脓毒症患者预后的预测价值[J]. 临床急诊杂志, 2023, 24(4): 173-178, 184. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.04.001
[21] 周亮亮, 吴婧, 赵宁玲, 等. 入院血清肝素结合蛋白是脓毒症患者并发器官功能障碍的独立危险因素[J]. 中国中西医结合急救杂志, 2023, 30(2): 136-141.
[22] Linder A, Arnold R, Boyd JH, et al. Heparin-Binding Protein Measurement Improves the Prediction of Severe Infection With Organ Dysfunction in the Emergency Department[J]. Crit Care Med, 2015, 43(11): 2378-2386. doi: 10.1097/CCM.0000000000001265
[23] Linder A, Christensson B, Herwald H, et al. Heparin-binding protein: an early marker of circulatory failure in sepsis[J]. Clin Infect Dis, 2009, 49(7): 1044-1050. doi: 10.1086/605563
[24] Hamilton FW, Thomas M, Arnold D, et al. Therapeutic potential of IL6R blockade for the treatment of sepsis and sepsis-related death: A Mendelian randomisation study[J]. PLoS Med, 2023, 20(1): e1004174. doi: 10.1371/journal.pmed.1004174
[25] Lu Z, Li X, Yang P, et al. Heparin-Binding Protein Enhances NF-κB Pathway-Mediated Inflammatory Gene Transcription in M1 Macrophages via Lactate[J]. Inflammation, 2021, 44(1): 48-56.
-

计量
- 文章访问数: 263
- 施引文献: 0



 下载:
下载: