Early dynamic monitoring of the predictive value of heparin-binding protein in elderly patients with sepsis
-
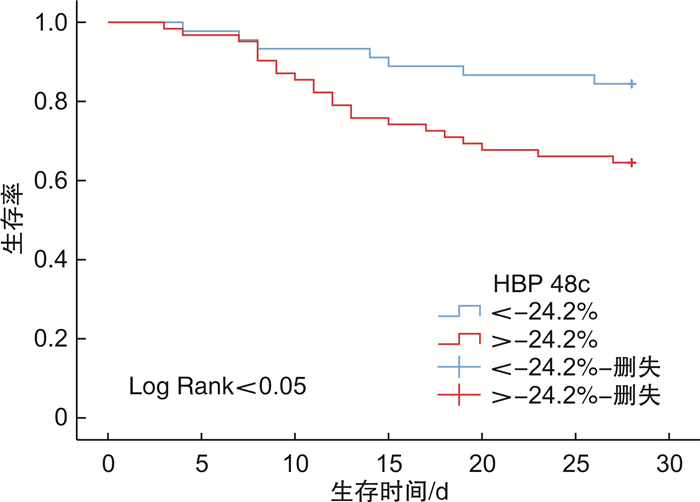
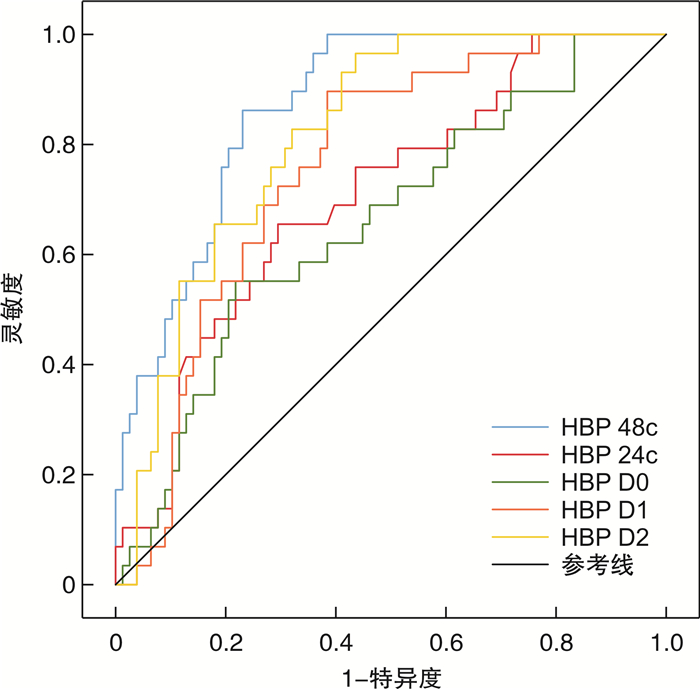
摘要: 目的 评估早期动态监测血浆肝素结合蛋白(heparin-binding protein,HBP)水平对65周岁及以上老年脓毒症患者临床预后的预测价值。方法 选取2021年9月1日—2022年8月31日入住潍坊医学院附属医院重症医学科(intensive care unit,ICU)并诊断为脓毒症的老年患者107例。记录患者转入ICU时的一般人口学特征、基本生命体征及相关化验指标,并在转入后24 h内完成SOFA评分和APACHE Ⅱ评分。检测患者转入ICU时(D0)、转入后24 h(D1),转入后48 h(D2)的血浆HBP水平,并计算HBP的24 h变化率(24c)及48 h变化率(48c)。根据患者28 d内的预后情况,分为存活组和死亡组。绘制ROC曲线评价不同时间点的血浆HBP水平及变化率对老年脓毒症患者预后的预测价值,采用Kaplan-Meier生存曲线分析生存率的差异,使用Cox回归分析相关指标与患者预后不良的关系。结果 死亡组患者入院时的SOFA评分和APACHE Ⅱ评分较存活组高,差异均有统计学意义(P < 0.001);死亡组的白蛋白水平相对较低,差异有统计学意义(P < 0.001);与存活组相比,死亡组患者D0(P=0.012)、D1(P < 0.001)、D2(P < 0.001)的血浆HBP水平更高,且存活组患者的HBP水平在48 h内明显下降,而死亡组患者的HBP水平下降速度较慢甚至仍然保持在较高的水平,两组患者HBP 24c和48c差异有统计学意义(P < 0.05);血浆HBP的48c、D2、D1、24c、D0预测患者预后不良的AUC依次为0.870、0.817、0.760、0.705、0.658;当HBP的48c截断值为-24.2%时,其约登指数为0.631,综合比较后最有诊断价值;绘制HBP 48c为-24.2%时的Kaplan-Meier曲线,患者HBP 48c>-24.2%时生存率更低(P < 0.05);Cox回归分析显示SOFA评分和APACHE Ⅱ评分升高、白蛋白水平降低及HBP 24c和48c升高是患者预后不良的危险因素。结论 血浆HBP 48 h变化率能较好的反映老年脓毒症患者的预后,在临床中可以动态监测老年脓毒症患者的血浆HBP水平,以便早期识别可能预后不良的患者。Abstract: Objective To evaluate the predictive value of early dynamic monitoring of plasma heparin-binding protein(HBP) levels on the clinical prognosis of sepsis in patients over 65 years of age(including 65 years).Methods A total of 107 elderly patients admitted to the ICU of the Affiliated Hospital of Weifang Medical University from September 1, 2021 to August 31, 2022 and diagnosed with sepsis were selected. The general demographic characteristics, basic vital signs and related laboratory indicators were recorded when the patients were transferred to the ICU, and the SOFA score and APACHE Ⅱ score were completed within 24 hours after the transfer. The plasma HBP levels were detected when the patients were transferred to ICU(D0), 24 h after transfer(D1), and 48 h after transfer(D2). Meanwhile, the 24 h change rate(24c) and 48 h change rate(48c) of HBP were calculated. According to the prognosis of patients within 28 days, they were divided into survival group and death group. The receiver operating characteristic curve(ROC) was drawn, and then the predictive value of plasma HBP levels and change rates at different time spots on the prognosis of elderly patients with sepsis were evaluated. Kaplan-Meier survival curves were used to analyze the differences in survival rates, and Cox regression was used to analyze the relationship between related indicators and poor prognosis of patients.Results The SOFA score and APACHE Ⅱ score of the patients in the death group were higher than those in the survival group, and the differences were all statistically significant(P < 0.001). The albumin level was lower in the death group, and the difference was statistically significant(P < 0.001). Compared with the survival group, the plasma HBP levels at D0(P=0.012), D1(P < 0.001) and D2(P < 0.001) were higher in the death group; And the HBP level of patients in the survival group decreased significantly within 48 hours, but decreased slowly or even remained at a high level in the death group, there were statistically significant differences between the two groups in HBP 24c and 48c(P < 0.05). The AUC of plasma HBP 48c, D2, D1, 24c, and D0 in predicting poor prognosis of patients were 0.870, 0.817, 0.760, 0.705, and 0.658, respectively. When the HBP 48c cut off value was -24.2%, its Youden index was 0.631, which is the most diagnostic value after comprehensive comparison. The Kaplan-Meier curve was drawn when HBP 48c was -24.2%, and the survival rate of patients with HBP 48c>-24.2% was lower(P < 0.05). Cox regression analysis showed that the increase of SOFA score and APACHE Ⅱ score, decrease of albumin level and increase of HBP 24c and 48c were the influencing factors of poor prognosis of patients.Conclusion Plasma HBP 48c can better reflect prognosis of elderly patients with sepsis, which suggested that in clinical practice, the plasma HBP levels of elderly patients with sepsis can be dynamically monitored, and patients with poor prognosis can be identified early.
-
Key words:
- dynamic monitoring /
- heparin-binding protein /
- sepsis /
- prognosis
-

-
表 1 存活组与死亡组基本资料比较
例(%),X±S,M(P25,P75) 临床特征 存活组(n=78) 死亡组(n=29) t/χ2/z P 男性 37(47.43) 18(62.07) 1.812 0.178 年龄/岁 75(70,83) 74(71,85) -0.551 0.582 心率/(次/min) 93±17 93±21 0.183 0.855 体温/℃ 37.0(36.5,37.8) 36.9(36.4,38.1) -0.108 0.914 MAP/mmHga) 84.9±15.7 88.4±16.6 -1.027 0.307 呼吸/(次/min) 19(18,20) 20(18,22) -1.384 0.166 SOFA评分/分 5(4,7) 7(6,10) -3.965 < 0.001 APACHE Ⅱ评分/分 17(15,19) 21(18,25) -3.829 < 0.001 合并症 高血压 36(46.15) 12(41.38) 0.277 0.598 冠心病 21(26.92) 12(41.38) 2.742 0.098 糖尿病 19(24.36) 11(37.93) 2.625 0.105 肿瘤 11(14.10) 7(24.14) 1.861 0.173 脑血管病 12(15.38) 5(17.24) 0.051 0.821 感染来源 0.007 0.997 呼吸系统 38(48.72) 14(48.28) 消化系统 27(34.62) 10(34.48) 皮肤或软组织 7(8.97) 3(10.34) 泌尿系统 6(7.69) 2(6.90) 休克 19(24.36) 13(44.83) 4.225 0.040 PCT/(ng/mL) 8.09(3.55,15.23) 5.44(2.43,15.54) -5.515 0.606 CRP/(mg/L) 59.99(11.49,172.68) 151.00(73.29,247.68) -1.451 0.147 白细胞计数/(×109/L) 8.77(6.18,12.82) 9.40(7.22,12.85) -0.792 0.428 中性粒细胞绝对值/(×109/L) 6.37(4.22,10.79) 8.36(5.86,11.35) -1.577 0.115 红细胞比容/% 37.3(34.4,41.8) 36.5(33.1,39.3) -0.918 0.358 血小板/(×109/L) 176(149,251) 186(145,294) -0.596 0.551 纤维蛋白原/(g/L) 4.78±1.76 4.68±2.15 0.260 0.222 D-二聚体/(mg/L) 0.67(0.33,1.65) 0.90(0.34,1.91) -0.624 0.533 谷草转氨酶/(U/L) 36.5(27.5,52.8) 33.4(27.9,39.6) -0.834 0.404 谷丙转氨酶/(U/L) 39.3(30.3,61.0) 36.0(33.2,42.0) -0.340 0.734 白蛋白/(g/L) 35.70(31.10,39.03) 27.50(24.60,31.65) -4.717 < 0.001 总胆红素/(μmol/L) 20.00(11.73,26.43) 16.90(13.22,24.14) -0.133 0.894 肌酐/(μmol/L) 83.5(63.00,117.8) 84.0(56.1,140.4) -0.144 0.886 血清Na+/(mmol/L) 138.9(134.8,141.4) 136.8(130.0,140.5) -1.251 0.211 注:a)1 mmHg=0.133 kPa。 表 2 HBP基线水平及动态变化
M(P25,P75) 指标 存活组 死亡组 Z P HBP D0/(ng/mL) 123.77(88.70,182.84) 206.13(103.63,277.72) -2.509 0.012 HBP D1/(ng/mL) 82.30(40.13,126.74) 172.62(102.21,244.43) -4.121 < 0.001 HBP D2/(ng/mL) 81.85(32.10,152.67) 205.64(130.90,277.05) -5.025 < 0.001 HBP 24c/% -46.40(-61.07,-26.00) -24.30(-45.15,20.80) -3.249 0.001 HBP 48c/% -43.87(-65.10,-25.87) -2.41(-20.09,29.17) -5.866 < 0.001 表 3 预测预后的ROC曲线特征
指标 AUC SE 95% CI P HBP 48c 0.870 0.033 0.805~0.935 < 0.001 HBP D2 0.817 0.041 0.738~0.896 < 0.001 HBP D1 0.760 0.048 0.667~0.853 < 0.001 HBP 24c 0.705 0.055 0.598~0.812 0.001 HBP D0 0.658 0.059 0.543~0.774 0.012 表 4 HBP不同时间点、变化率的截断值及约登指数
指标 截断值 灵敏度/% 特异度/% 约登指数 HBP 48c -24.2% 86.2 76.9 0.631 HBP D2 88.66 96.6 56.4 0.530 HBP D1 92.65 89.7 61.5 0.512 HBP 24c -35.1% 65.5 70.5 0.360 HBP D0 192.31 55.2 78.2 0.334 表 5 Cox生存回归分析影响老年脓毒症患者死亡的危险因素
指标 B SE Wald HR 95% CI P SOFA评分 0.210 0.095 4.901 1.234 1.024~1.485 0.027 APACHE Ⅱ评分 0.111 0.055 4.010 1.117 1.002~1.245 0.045 白蛋白 -0.127 0.033 14.706 0.881 0.826~0.940 < 0.001 HBP D0 0.009 0.005 3.512 1.009 1.000~1.019 0.061 HBP D1 -0.012 0.006 3.622 0.988 0.976~1.000 0.057 HBP D2 0.001 0.006 0.014 1.001 0.990~1.012 0.905 HBP 24c 1.863 0.850 4.799 6.440 1.217~34.089 0.028 HBP 48c 1.643 0.769 4.561 5.170 1.145~23.353 0.033 -
[1] Kaukonen KM, Bailey M, Suzuki S, et al. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012[J]. JAMA, 2014, 311(13): 1308-1316. doi: 10.1001/jama.2014.2637
[2] Michels EHA, Butler JM, Reijnders TDY, et al. Association between age and the host response in critically ill patients with sepsis[J]. Crit Care, 2022, 26(1): 385. doi: 10.1186/s13054-022-04266-9
[3] Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[4] Martin-Loeches I, Guia MC, Vallecoccia MS, et al. Risk factors for mortality in elderly and very elderly critically ill patients with sepsis: a prospective, observational, multicenter cohort study[J]. Ann Intensive Care, 2019, 9(1): 26. doi: 10.1186/s13613-019-0495-x
[5] Rowe TA, McKoy JM. Sepsis in older adults[J]. Infect Dis Clin North Am, 2017, 31(4): 731-742. doi: 10.1016/j.idc.2017.07.010
[6] Xu H, Li T, Zhang X, et al. Impaired circulating antibody-secreting cells generation predicts the dismal outcome in the elderly septic shock patients[J]. J Inflamm Res, 2022, 15: 5293-5308. doi: 10.2147/JIR.S376962
[7] Zhang LM, Huang T, Xu FS, et al. Prediction of prognosis in elderly patients with sepsis based on machine learning(random survival forest)[J]. BMC Emerg Med, 2022, 22(1): 26. doi: 10.1186/s12873-022-00582-z
[8] 闫圣涛, 练睿, 孙力超, 等. 降钙素原和危重症评分在腹腔感染脓毒症病原学诊断及预后评估中的价值[J]. 中华危重病急救医学, 2021, 33(7): 792-797. doi: 10.3760/cma.j.cn121430-20200909-00621
[9] Tan MC, Lu YX, Jiang H, et al. The diagnostic accuracy of procalcitonin and C-reactive protein for sepsis: a systematic review and meta-analysis[J]. J Cell Biochem, 2019, 120(4): 5852-5859. doi: 10.1002/jcb.27870
[10] He WX, Xiao K, Fang M, et al. Immune cell number, phenotype, and function in the elderly with sepsis[J]. Aging Dis, 2021, 12(1): 277-296. doi: 10.14336/AD.2020.0627
[11] Pierrakos C, Velissaris D, Bisdorff M, et al. Biomarkers of sepsis: time for a reappraisal[J]. Crit Care, 2020, 24(1): 287. doi: 10.1186/s13054-020-02993-5
[12] Wu YL, Yo CH, Hsu WT, et al. Accuracy of heparin-binding protein in diagnosing sepsis: a systematic review and meta-analysis[J]. Crit Care Med, 2021, 49(1): e80-e90. doi: 10.1097/CCM.0000000000004738
[13] 谭德敏, 陈军, 张敏. 脓毒症患者血清HBP与器官损伤严重程度和临床结局的相关性研究[J]. 临床急诊杂志, 2022, 23(6): 412-418. doi: 10.13201/j.issn.1009-5918.2022.06.008
[14] 张重威, 祝益民, 曹彦, 等. 肝素结合蛋白对脓毒症的预测价值[J]. 中华危重病急救医学, 2021, 33(6): 654-658. doi: 10.3760/cma.j.cn121430-20210424-00605
[15] Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016[J]. Intensive Care Med, 2017, 43(3): 304-377. doi: 10.1007/s00134-017-4683-6
[16] Rowe T, Araujo KLB, Van Ness PH, et al. Outcomes of older adults with sepsis at admission to an intensive care unit[J]. Open Forum Infect Dis, 2016, 3(1): ofw010. doi: 10.1093/ofid/ofw010
[17] Norman DC. Clinical features of infection in older adults[J]. Clin Geriatr Med, 2016, 32(3): 433-441. doi: 10.1016/j.cger.2016.02.005
[18] Boonmee P, Ruangsomboon O, Limsuwat C, et al. Predictors of mortality in elderly and very elderly emergency patients with sepsis: a retrospective study[J]. West J Emerg Med, 2020, 21(6): 210-218. http://www.xueshufan.com/publication/3101938229
[19] 杨光耀, 郑文龙, 盛鹰, 等. 血尿素氮联合快速序贯器官衰竭评分对老年脓毒症患者预后的评估价值[J]. 中国急救医学, 2022, 42(3): 209-213. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJJY202203004.htm
[20] Chou EH, Mann S, Hsu TC, et al. Incidence, trends, and outcomes of infection sites among hospitalizations of sepsis: a nationwide study[J]. PLoS One, 2020, 15(1): e0227752. doi: 10.1371/journal.pone.0227752
[21] 许伟, 吴剑卿. 衰弱综合征与老年肺部感染[J]. 实用老年医学, 2022, 36(8): 784-787. doi: 10.3969/j.issn.1003-9198.2022.08.008
[22] Eckart A, Struja T, Kutz A, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study[J]. Am J Med, 2020, 133(6): 713-722. e7. doi: 10.1016/j.amjmed.2019.10.031
[23] Arnau-Barrés I, Güerri-Fernández R, Luque S, et al. Serum albumin is a strong predictor of sepsis outcome in elderly patients[J]. Eur J Clin Microbiol Infect Dis, 2019, 38(4): 743-746. doi: 10.1007/s10096-019-03478-2
[24] Di Napoli M, Behrouz R, Topel CH, et al. Hypoalbuminemia, systemic inflammatory response syndrome, and functional outcome in intracerebral hemorrhage[J]. J Crit Care, 2017, 41: 247-253. doi: 10.1016/j.jcrc.2017.06.002
[25] Zhang XM, Zhang WW, Yu XZ, et al. Comparing the performance of SOFA, TPA combined with SOFA and APACHE-Ⅱ for predicting ICU mortality in critically ill surgical patients: a secondary analysis[J]. Clin Nutr, 2020, 39(9): 2902-2909. doi: 10.1016/j.clnu.2019.12.026
[26] Haas LEM, Termorshuizen F, de Lange DW, et al. Performance of the quick SOFA in very old ICU patients admitted with sepsis[J]. Acta Anaesthesiol Scand, 2020, 64(4): 508-516. doi: 10.1111/aas.13536
[27] 高翔, 张明, 张勇, 等. 血浆肝素结合蛋白对脓毒症相关急性肾损伤的早期诊断及预后预测[J]. 临床急诊杂志, 2021, 22(10): 647-652. doi: 10.13201/j.issn.1009-5918.2021.10.002
[28] 王亮, 马晓春. 肝素结合蛋白的结构和功能特点及其在脓毒症中的作用[J]. 中华危重病急救医学, 2014, 26(3): 200-203. doi: 10.3760/cma.j.issn.2095-4352.2014.03.018
[29] Opal SM, van der Poll T. Endothelial barrier dysfunction in septic shock[J]. J Intern Med, 2015, 277(3): 277-293. doi: 10.1111/joim.12331
[30] Katsaros K, Renieris G, Safarika A, et al. Heparin binding protein for the early diagnosis and prognosis of sepsis in the emergency department: the prompt multicenter study[J]. Shock, 2022, 57(4): 518-525. doi: 10.1097/SHK.0000000000001900
[31] Kahn F, Tverring J, Mellhammar L, et al. Heparin-binding protein as a prognostic biomarker of sepsis and disease severity at the emergency department[J]. Shock, 2019, 52(6): e135-e145. doi: 10.1097/SHK.0000000000001332
[32] Yeh CF, Wu CC, Liu SH, et al. Comparison of the accuracy of neutrophil CD64, procalcitonin, and C-reactive protein for sepsis identification: a systematic review and meta-analysis[J]. Ann Intensive Care, 2019, 9(1): 5. doi: 10.1186/s13613-018-0479-2
[33] 徐策, 葛新, 宦陟榕. 脓毒症患者血清HBP水平与常规炎症标志物相关性及联合HBP清除率对不良预后的预测价值[J]. 临床急诊杂志, 2021, 22(9): 582-586. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202109003.htm
-




 下载:
下载: