The predictive value of ROX index related parameters for high-flow nasal cannula oxygen therapy failure in elderly patients with pneumonia-related acute hypoxemia respiratory failure
-
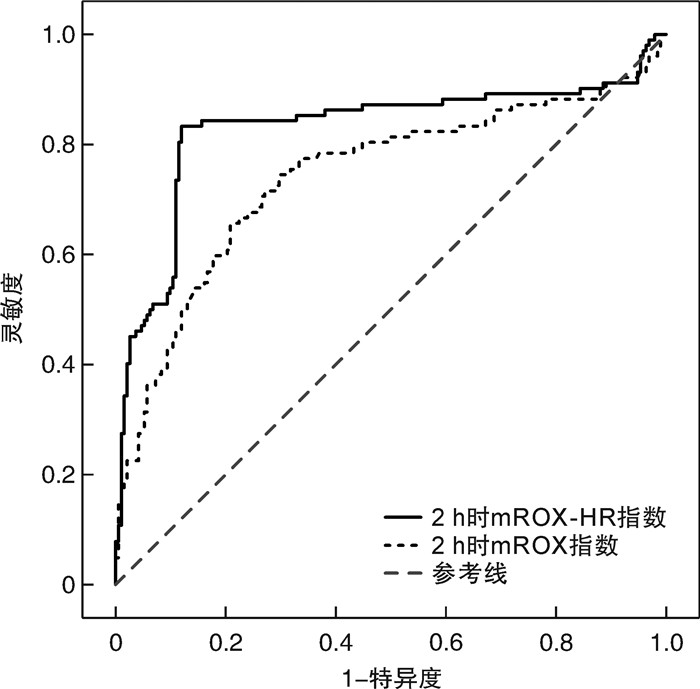
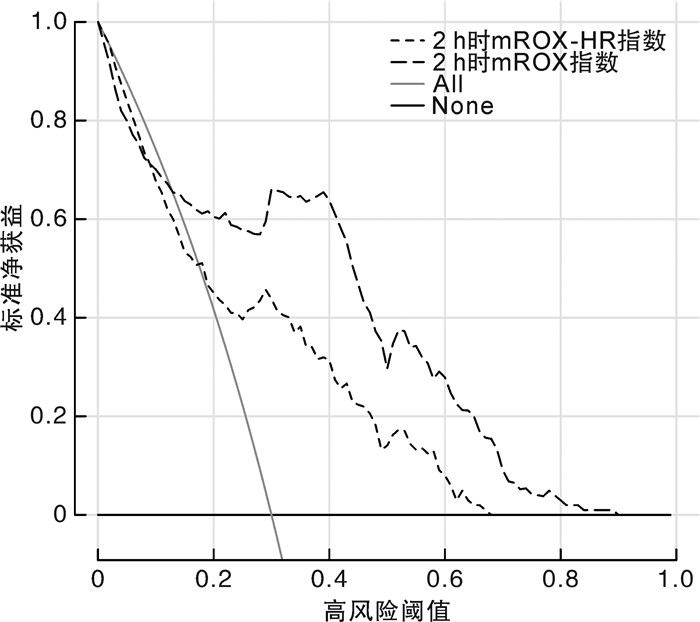
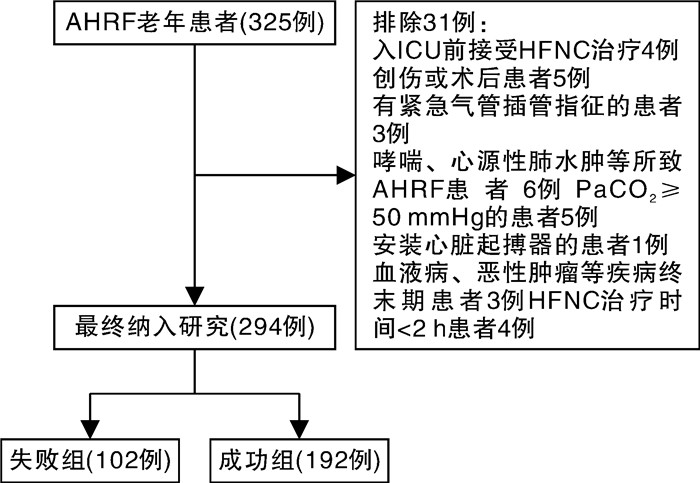
摘要: 目的 探讨呼吸频率氧合(respiratory rate oxygenation,ROX)指数、改良ROX(modifed ROX,mROX)指数、ROX增加心率(ROX-HR)指数和mROX增加心率(mROX-HR)指数对肺炎所致急性低氧性呼吸衰竭(acute hypoxemic respiratory failure,AHRF)老年患者经鼻高流量湿化氧疗(high-flow nasal cannula oxygen therapy,HFNC)治疗失败的预测价值。方法 回顾性研究2021年1月—2023年6月期间收住在海南医学院第二附属医院重症监护病房(intensive care unit,ICU)的294例接受HFNC治疗的肺炎所致AHRF老年患者的临床资料,以后续是否接受机械通气将患者分为失败组(102例)和成功组(192例)。采集2组患者的一般资料、生理参数、血气分析参数、实验室指标,并计算HFNC治疗启动时和HFNC治疗后2 h时的ROX指数、ROX-HR指数、mROX指数和mROX-HR指数。采用单因素分析和多因素logistic回归分析探讨ROX指数相关参数与HFNC治疗失败的关系。采用受试者工作特征(receiver operating characteristic,ROC)曲线和决策曲线分析(decision curve analysis,DCA)评价ROX指数相关参数对HFNC治疗失败的预测价值和临床实用性。结果 本研究中的HFNC治疗失败率为34.69%。失败组患者年龄、合并慢性阻塞性肺疾病比例、合并脑血管疾病比例、序贯器官衰竭估计评分、ICU停留时间、28 d病死率高于(长于)成功组,治疗后2 h时ROX指数、ROX-HR指数、mROX指数和mROX-HR指数低于成功组,差异均有统计学意义(P<0.05)。多因素logistic回归分析显示,经调整其他相关因素后,HFNC治疗2 h时的mROX指数(OR=0.550,95%CI:0.437~0.693)和mROX-HR指数(OR=0.327,95%CI:0.236~0.453)升高分别为AHRF老年患者HFNC治疗失败的独立保护因素(P<0.05)。ROC曲线分析显示,HFNC治疗2 h时的mROX指数预测HFNC治疗失败的曲线下面积(area under the curve,AUC)为0.742(95%CI:0.688~0.791),最佳截断值为5.38,灵敏度为65.69%,特异度为79.17%;HFNC治疗2 h时的mROX-HR指数预测HFNC治疗失败的AUC为0.829(95%CI:0.781~0.870),最佳截断值为5.48,灵敏度为83.33%,特异度为88.02%;mROX-HR指数的AUC大于mROX指数的AUC(Z=4.027,P<0.001)。DCA结果显示,当高风险阈值在0.15~0.90范围内,mROX-HR指数预测HFNC治疗失败的净获益率优于mROX指数预测。结论 HFNC治疗2 h时的mROX指数和mROX-HR指数升高是AHRF老年患者HFNC治疗失败的独立保护因素,并且对HFNC治疗失败有一定的预测价值和临床实用性。Abstract: Objective To investigate the predictive value of respiratory rate oxygenation(ROX) index, modifed ROX(mROX) index, ROX by adding heart rate(ROX-HR) index, and mROX by adding heart rate(mROX-HR) index for high-flow nasal cannula oxygen therapy(HFNC) failure in elderly patients with pneumonia-related acute hypoxemia respiratory failure(AHRF).Methods A retrospective study was conducted to investigate clinical data of 294 elderly patients with pneumonia-related AHRF treated with HFNC in the department of intensive care unit(ICU) of the Second Affiliated Hospital of Hainan Medical University from January 2021 to June 2023. Patients were divided into the failure group(n=102) and the success group(n=192) according to whether they subsequently received mechanical ventilation. The general data, physiological parameters, blood gas analysis parameters and laboratory indicators in the two groups were collected, and the ROX index, ROX-HR index, mROX index and mROX-HR index were calculated at HFNC initiation and 2 h after HFNC. Univariate analysis and multivariate logistic regression analysis were used to explore the relationship between ROX index related parameters and HFNC failure. The receiver operating characteristic(ROC) curve and decision curve analysis(DCA) were used to evaluate the predictive value and clinical practicability of ROX index related parameters for HFNC failure.Results The rate of HFNC failure in this study was 34.69%. The age, proportion of chronic obstructive pulmonary disease, proportion of cardiovascular disease, sequential organ failure assessment score, length of stay in ICU, and 28-days mortality in the failure group were higher/longer than those of the success group, and the ROX index, ROX-HR index, mROX index and mROX-HR index at 2 h after HFNC in the failure group were lower than those of the success group, with the differences were statistically significant(P<0.05). Multivariate logistic regression analysis showed that after adjusting other related factors, the elevated value of mROX index(OR=0.550, 95%CI: 0.437-0.693) and mROX-HR index(OR=0.327, 95%CI: 0.236-0.453) at 2 h after HFNC were independent protective factors for HFNC failure in elderly patients with AHRF(P<0.05). The ROC curve analysis showed that the area under the curve(AUC) for mROX index at 2 h after HFNC to predict HFNC failure curve was 0.742(95%CI: 0.688-0.791), the best cut-off value was 5.38, the sensitivity was 65.69%, and specificity was 79.17%. The AUC for mROX-HR index at 2 h after HFNC to predict HFNC failure curve was 0.829(95%CI: 0.781-0.870), the best cut-off value was 5.48, the sensitivity was 83.33%, and specificity was 88.02%. The AUC of mROX-HR index was greater than that of mROX index(Z=4.027, P<0.001). The DCA results showed that, within the thresholds of 0.15-0.90, the net benefit rate of mROX-HR index to predicted HFNC failure was better than that of the mROX index.Conclusion The elevated value of mROX index and mROX-HR index at 2 h after HFNC are independent protective factors for HFNC failure in elderly patients with AHRF, and have certain predictive value and clinical practicability for HFNC failure.
-

-
表 1 两组患者临床资料比较
X±S,M(P25,P75) 指标 失败组(102例) 成功组(192例) Z/t/χ2 P 性别/例 0.230 0.631 男 64 108 女 38 84 年龄/岁 74.88±6.97 72.76±6.72 -2.547 0.011 BMI/(kg/m2) 25.46±3.71 25.37±3.83 -0.184 0.854 基础疾病/例(%) 慢性心衰 25(24.51) 32(16.67) 2.622 0.105 高血压 47(46.08) 73(38.02) 1.790 0.181 糖尿病 29(28.43) 49(25.52) 0.289 0.591 COPD 44(43.14) 34(17.71) 22.098 <0.001 脑血管疾病 39(38.24) 36(18.75) 13.309 <0.001 肺炎分型/例(%) 0.665 0.415 社区获得性 72(70.59) 144(75.00) 医院获得性 30(29.41) 48(25.00) 病原体分型/例(%) 1.382 0.847 细菌 31(30.39) 53(27.60) 病毒 15(14.71) 38(19.79) 支原体 11(10.78) 22(11.46) 混合 13(12.75) 21(10.94) 病原体阴性 32(30.48) 58(30.21) SOFA评分/分 7.71±2.96 6.72±2.70 -2.898 0.004 实验室指标 WBC/(×109/L) 14.25±6.23 13.68±5.61 -0.792 0.429 NeuC/(×109/L) 13.05±6.79 12.11±5.42 -1.292 0.198 PCT/(μg/L) 5.24(1.43,14.69) 3.74(1.31,12.33) -1.217 0.224 CRP/(mg/L) 27.75(22.84,42.50) 26.00(21.09,39.11) -0.987 0.323 Lac/(mmol/L) 3.40(2.39,4.40) 3.20(1.84,4.20) -1.013 0.311 启动时ROX相关参数 RR/(次/min) 26.31±4.76 26.37±5.10 0.108 0.914 HR/(次/min) 101.87±18.71 99.15±14.90 -1.360 0.175 SpO2/% 92.89±7.08 93.44±5.99 0.704 0.482 PaO2/mmHg 76.78±29.69 81.01±32.09 1.103 0.271 FiO2 0.57±0.19 0.57±0.24 -0.023 0.982 ROX 7.02±2.47 7.44±3.12 1.199 0.232 ROX-HR 7.09±2.60 7.76±3.96 1.535 0.126 mROX 5.68±2.61 6.16±2.46 1.506 0.134 mROX-HR 5.77±2.93 6.39±2.91 1.733 0.084 2 h时ROX相关参数 RR/(次/min) 25.24±5.04 24.31±4.56 -1.600 0.111 HR/(次/min) 99.53±14.22 97.13±13.01 -1.461 0.145 SpO2/% 94.21±2.85 94.63±1.96 1.504 0.134 PaO2/mmHg 80.83±36.49 86.85±21.90 1.765 0.079 FiO2 0.60±0.13 0.58±0.12 -1.194 0.234 ROX 6.77±1.79 7.28±2.02 2.147 0.033 ROX-HR 6.93±2.03 7.67±2.60 2.487 0.013 mROX 5.34±1.67 6.35±1.30 5.721 <0.001 mROX-HR 5.32±1.28 6.56±1.23 8.154 <0.001 预后指标 ICU停留时间/d 6.00(4.00,9.00) 4.00(3.00,7.00) -3.902 <0.001 28 d死亡/例(%) 25(24.51) 24(12.50) 6.918 0.009 表 2 AHRF老年患者HFNC治疗失败的多因素logistic回归分析
自变量 β SE Wald χ2 OR 95%CI P 2 h时ROX指数a) -0.054 0.075 0.530 0.947 0.818~1.096 0.467 2 h时ROX-HR指数a) -0.066 0.062 1.142 0.936 0.829~1.057 0.285 2 h时mROX指数a) -0.597 0.117 25.947 0.550 0.437~0.693 <0.001 2 h时mROX-HR指数a) -1.118 0.167 45.062 0.327 0.236~0.453 <0.001 注:a)调整年龄、COPD、脑血管疾病、SOFA评分。 -
[1] Kwizera A, Nakibuuka J, Nakiyingi L, et al. Acute hypoxaemic respiratory failure in a low-income country: a prospective observational study of hospital prevalence and mortality[J]. BMJ Open Respir Res, 2020, 7(1): e000719. doi: 10.1136/bmjresp-2020-000719
[2] 刘霜, 朱华栋, 于学忠, 等. 经鼻高流量氧疗和无创正压通气对于肺源性中重度急性呼吸窘迫综合征患者初始治疗的效果评价[J]. 临床急诊杂志, 2020, 21(3): 181-187. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2020.03.001
[3] Rochwerg B, Granton D, Wang DX, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis[J]. Intensive Care Med, 2019, 45(5): 563-572.
[4] Yasuda H, Okano H, Mayumi T, et al. Association of noninvasive respiratory support with mortality and intubation rates in acute respiratory failure: a systematic review and network meta-analysis[J]. J Intensive Care, 2021, 9(1): 32. doi: 10.1186/s40560-021-00539-7
[5] Zhou X, Liu J, Pan J, et al. The ROX index as a predictor of high-flow nasal cannula outcome in pneumonia patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis[J]. BMC Pulm Med, 2022, 22(1): 121. doi: 10.1186/s12890-022-01914-2
[6] Karim HMR, Esquinas AM. Success or Failure of High-Flow Nasal Oxygen Therapy: The ROX Index Is Good, but a Modified ROX Index May Be Better[J]. Am J Respir Crit Care Med, 2019, 200(1): 116-117. doi: 10.1164/rccm.201902-0419LE
[7] Frat JP, Ragot S, Coudroy R, et al. Predictors of intubation in patients with acute hypoxemic respiratory failure treated with a noninvasive oxygenation strategy[J]. Crit Care Med, 2018, 46(2): 208-215. doi: 10.1097/CCM.0000000000002818
[8] 中华医学会呼吸病学分会. 中国成人社区获得性肺炎诊断和治疗指南(2016年版)[J]. 中华结核和呼吸杂志, 2016, 39(4): 253-279. doi: 10.3760/cma.j.issn.1001-0939.2016.04.005
[9] 中国医师协会急诊医师分会, 中华医学会急诊医学分会, 中国急诊专科医联体, 等. 急诊成人经鼻高流量氧疗临床应用专家共识[J]. 中国急救医学, 2021, 41(9): 739-749. doi: 10.3969/j.issn.1002-1949.2021.09.002
[10] Kansal A, Ong WJD, Dhanvijay S, et al. Comparison of ROX index(SpO2/FiO2 ratio/respiratory rate)with a modified dynamic index incorporating PaO2/FiO2 ratio and heart rate to predict high flow nasal cannula outcomes among patients with acute respiratory failure: a single centre retrospective study[J]. BMC Pulm Med, 2022, 22(1): 350. doi: 10.1186/s12890-022-02121-9
[11] Zhang C, Ou M. Comparison of hypoxemia, intubation procedure, and complications for non-invasive ventilation against high-flow nasal cannula oxygen therapy for patients with acute hypoxemic respiratory failure: a non-randomized retrospective analysis for effectiveness and safety(NIVaHIC-aHRF)[J]. BMC Emerg Med, 2021, 21(1): 6. doi: 10.1186/s12873-021-00402-w
[12] Rochwerg B, Einav S, Chaudhuri D, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline[J]. Intensive Care Med, 2020, 46(12): 2226-2237. doi: 10.1007/s00134-020-06312-y
[13] Ricard JD, Roca O, Lemiale V, et al. Use of nasal high flow oxygen during acute respiratory failure[J]. Intensive Care Med, 2020, 46(12): 2238-2247. doi: 10.1007/s00134-020-06228-7
[14] 林钊华, 黄霞, 杨叶桂, 等. 经鼻高流量氧疗在老年急性呼吸衰竭患者中应用效果及预后危险因素分析[J]. 临床急诊杂志, 2023, 24(2): 62-67. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2023.02.003
[15] Frat JP, Ricard JD, Quenot JP, et al. Non-invasive ventilation versus high-flow nasal cannula oxygen therapy with apnoeic oxygenation for preoxygenation before intubation of patients with acute hypoxaemic respiratory failure: a randomised, multicentre, open-label trial[J]. Lancet Respir Med, 2019, 7(4): 303-312. doi: 10.1016/S2213-2600(19)30048-7
[16] 王重阳, 王璐, 郭仁楠, 等. ROX指数预测老年重症社区获得性肺炎患者气管插管的有效性分析[J]. 临床急诊杂志, 2022, 23(12): 854-858. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.12.010
[17] Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index[J]. J Crit Care, 2016, 35(1): 200-205.
[18] Junhai Z, Jing Y, Beibei C, et al. The value of ROX index in predicting the outcome of high flow nasal cannula: a systematic review and meta-analysis[J]. Respir Res, 2022, 23(1): 33. doi: 10.1186/s12931-022-01951-9
[19] Prakash J, Bhattacharya PK, Yadav AK, et al. ROX index as a good predictor of high flow nasal cannula failure in COVID-19 patients with acute hypoxemic respiratory failure: A systematic review and meta-analysis[J]. J Crit Care, 2021, 66(1): 102-108.
[20] Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy[J]. Am J Respir Crit Care Med, 2019, 199(11): 1368-1376. doi: 10.1164/rccm.201803-0589OC
[21] Goh KJ, Chai HZ, Ong TH, et al. Early prediction of high flow nasal cannula therapy outcomes using a modified ROX index incorporating heart rate[J]. J Intensive Care, 2020, 8(1): 41. doi: 10.1186/s40560-020-00458-z
[22] Choi SH, Kim DY, Song BY, et al. Analysis of ROX Index, ROX-HR Index, and SpO2/FIO2 Ratio in Patients Who Received High-Flow Nasal Cannula Oxygen Therapy in Pediatric Intensive Care Unit[J]. J Korean Acad Nurs, 2023, 53(4): 468-479. doi: 10.4040/jkan.22152
[23] Ray S, Rogers L, Pagel C, et al. PaO2/FiO2Ratio Derived From the SpO2/FiO2Ratio to Improve Mortality Prediction Using the Pediatric Index of Mortality-3 Score in Transported Intensive Care Admissions[J]. Pediatr Crit Care Med, 2017, 18(3): e131-e136. doi: 10.1097/PCC.0000000000001075
[24] Carvalho EB, Leite TRS, Sacramento RFM, et al. Rationale and limitations of the SpO2/FiO2 as a possible substitute for PaO2/FiO2 in different preclinical and clinical scenarios[J]. Rev Bras Ter Intensiva, 2022, 34(1): 185-196.
[25] Röttgering JG, De Man AME, Schuurs TC, et al. Determining a target SpO2to maintain PaO2within a physiological range[J]. PLoS One, 2021, 16(5): e0250740. doi: 10.1371/journal.pone.0250740
-




 下载:
下载: