Analysis of the effectiveness of ROX index in predicting tracheal intubation in elderly patients with severe community-acquired pneumonia
-
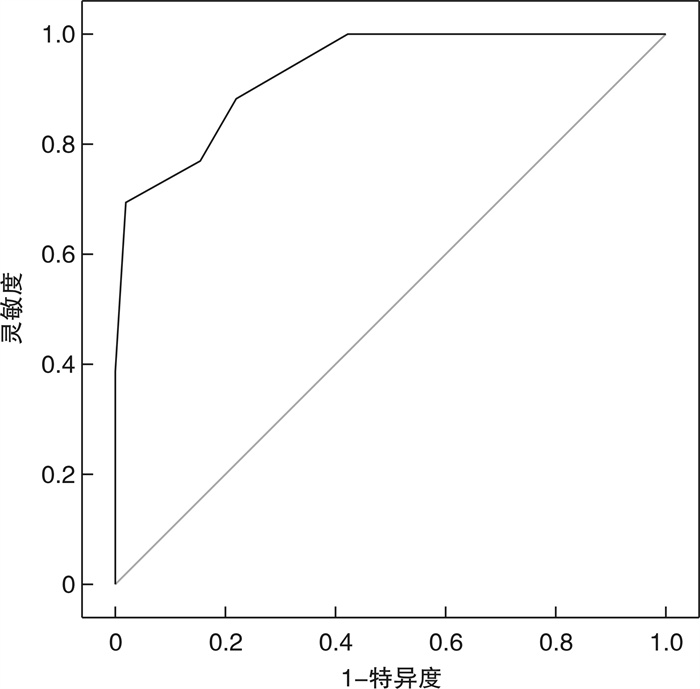
摘要: 目的 探讨ROX指数预测老年重症社区获得性肺炎(SCAP)患者气管插管的有效性。方法 选取既往于2022年1月1日—2022年9月1日新疆维吾尔自治区人民医院EICU收治的71例老年SCAP患者作为研究对象,根据患者住院期间是否进行气管插管,将其分为未插管组46例和插管组25例。比较2组一般资料:年龄、性别、体重指数(BMI)、基础疾病构成比、入院时APACHE Ⅱ评分、SOFA评分、CURB-65评分、白细胞计数、血小板计数、C反应蛋白(CRP)、降钙素原(PCT)、动脉血氧分压(PaO2)、氧合指数(PaO2/FiO2)、平均动脉压(MAP)、入院30 min内最差ROX指数、插管前30 min内最差ROX指数;并采用多因素logistic回归分析气管插管的独立显著预测因子;采用受试者工作曲线(ROC)确定最佳的气管插管预测截断值。结果 共计纳入研究的患者71例(男45例,女26例),非插管组46例(中位数年龄76岁),插管组25例(中位数年龄75岁);2组患者的年龄、性别、BMI、CURB-65评分、既往基础疾病构成比、入院时白细胞计数、血小板计数、CRP、MAP对比差异无统计学意义(均P>0.05);2组患者入院时的APACHE Ⅱ评分(t=-2.925,P=0.005)、SOFA评分(t=-2.411,P=0.019)、合并3种以上基础疾病构成比(χ2=-4.610,P=0.032)、PCT(t=-2.238,P=0.028)、PaO2(t=2.688,P=0.009)、PaO2/FiO2(t=2.881,P=0.005)、入院30 min内最差ROX指数(t=5.816,P<0.001)、插管前30 min内最差ROX指数(t=7.930,P<0.001)对比,差异有统计学意义(均P < 0.05)。多因素二元logistic回归分析显示,插管前30 min内最差ROX指数为是否插管的独立影响因素(OR=0.06,P=0.02)。插管前30 min内最差ROX指数对气管插管预测的ROC曲线下面积为0.93(95%CI:0.01~0.60,P<0.001)。最大约登指数为0.67,最佳截断值ROX指数=5.5时,对气管插管预测的灵敏度为0.67,特异度为0.97。结论 插管前ROX指数对预测老年SCAP患者气管插管的准确性较高,动态监测ROX指数有助于临床医师把握老年SCAP患者的插管时机。Abstract: Objective To investigate the effectiveness of ROX index in predicting tracheal intubation in elderly patients with Serious community acquired pneumonia(SCAP).Methods Seventy-one elderly SCAP patients previously admitted to the EICU of the People's Hospital of Xinjiang Uygur Autonomous Region from January 1, 2022 to September 1, 2022 were selected as study subjects and were divided into non-intubated group (46 cases) and intubated group (25 cases) according to whether the patients were intubated or not during hospitalization. The general data of the two groups were compared: age, gender, BMI, basic disease constituent ratio, APACHE Ⅱ score at admission, SOFA score, CURB-65 score, white blood cell count, platelet count, CRP, PCT, PaO2, PaO2/FiO2, MAP, worst ROX index within 30 min of admission, and worst ROX index within 30 min before intubation; and independent significant predictors of tracheal intubation were analyzed using multifactorial logistic regression; the subject operating curve (ROC) was used to determine the best predictive cutoff value for tracheal intubation.Results A total of 71 patients(45 males and 26 females) were included in the study, 46 in the non-intubated group(median age 76 years) and 25 in the intubated group(median age 75 years); there were no significant differences in age, gender, BMI, CURB-65 score, previous basic disease constituent ratio, white blood cell count at admission, platelet count, CRP, and MAP between the two groups(all P>0.05); the APACHE Ⅱ score(t=-2.925, P=0.005), SOFA score(t=-2.411, P=0.019), combined three or more basic disease constituent ratio(χ2=-4.610, P=0.032), PCT(t=-2.238, P=0.028), PaO2(t=2.688, P=0.009), PaO2/FiO2(t=2.881, P=0.005), worst ROX index within 30 min of admission(t=5.816, P < 0.001), and worst ROX index within 30 min before intubation(t=7.930, P < 0.001) were significantly different in comparison(all P < 0.05). Multi-factor binary logistic regression analysis showed that the worst ROX index within 30 min before intubation was an independent factor influencing whether to intubate(OR=0.06, P=0.02). The area under the ROC curve of the worst ROX index for predicting tracheal intubation within 30 min before intubation was 0.93, with a 95% confidence interval of 0.01-0.60, P < 0.001. The maximum Jorden index was 0.67 and the best cut-off value of ROX index was 5.5. The sensitivity for predicting tracheal intubation was 0.67 and the specificity was 0.97.Conclusion ROX index has a high accuracy in predicting the elderly SCAP patients before intubation. Dynamic monitoring of ROX index is helpful for clinicians to grasp the intubation opportunity of elderly SCAP patients.
-
Key words:
- severe community-acquired pneumonia /
- ROX index /
- tracheal intubation /
- prediction
-

-
表 1 2组患者的一般资料比较
特征 非插管组(46例) 插管组(25例) t/χ2/Z P 年龄/岁 76.0(74.0,79.3) 75.0(74.0,78.0) -0.728 0.467 男性/例(%) 29(65.9) 16(64.0) 0.026 0.873 BMI 22.1±4.4 21.1±4.3 0.932 0.355 入院时APACHE Ⅱ评分 14.8±3.9 18.1±5.2 -2.925 0.005 SOFA评分 4.7±1.3 5.8±2.5 -2.411 0.019 CURB-65评分 3.7±1.2 4.1±1.3 -1.195 0.236 既往基础疾病/例(%) 高血压 17(41.3) 9(36.0) 0.191 0.662 糖尿病 11(23.9) 5(20.0) 0.142 0.706 冠心病 10(21.7) 5(20.0) 0.029 0.864 慢性心功能不全 7(15.2) 6(24.0) 0.835 0.361 慢性支气管炎 5(10.9) 3(12.0) 0.021 0.886 合并两种以上上述疾病 9(20.0) 8(32.0) 1.259 0.262 合并3种以上上述疾病 4(8.7) 7(28.0) 4.610 0.032 入院时相关化验指标 白细胞计数/(×109·L-1) 10.9±6.0 11.5±6.1 -0.388 0.699 血小板计数/(×109·L-1) 153.8±97.4 134.8±98.1 0.783 0.436 CRP/(mg·L-1) 39.6±8.9 41.5±11.2 -0.924 0.237 PCT(ng·mL-1) 6.9±7.1 11.8±11.2 -2.238 0.028 PaO2/mmHg 64.0±3.9 60.5±7.3 2.688 0.009 PaO2/FiO2/mmHg 159.8±41.4 132.4±31.2 2.881 0.005 MAP/mmHg 85.3±17.9 77.8±20.9 1.599 0.114 入院30 min内最差ROX指数 8.7±2.2 5.9±1.4 5.816 0.000 插管前30 min内最差ROX指数 9.2±2.2 5.2±1.5 7.930 0.000 表 2 气管插管危险因素的二元logistic回归分析
危险因素 β 标准误 Wald 自由度 P OR 95%置信区间(CI) 下限值 上限值 APACHEⅡ评分 0.42 0.36 1.36 1 0.24 1.51 0.75 3.05 SOFA评分 -0.89 0.64 1.96 1 0.16 0.41 0.12 1.43 合并3种以上基础疾病 0.36 1.79 0.04 1 0.84 1.43 0.04 47.73 PCT -0.01 0.09 0.02 1 0.89 0.99 0.82 1.19 PaO2 -0.17 0.23 0.56 1 0.45 0.85 0.54 1.31 PaO2/FiO2 0.01 0.06 0.09 1 0.76 1.01 0.96 1.06 入院30 min内最差ROX指数 1.54 1.07 2.09 1 0.15 4.66 0.58 37.57 插管前30 min最差ROX指数 -2.75 1.17 5.54 1 0.02 0.06 0.01 0.63 常量 15.04 19.24 0.61 1 0.43 -
[1] 瞿介明, 曹彬. 中国成人社区获得性肺炎诊断和治疗指南(2016年版)修订要点[J]. 中华结核和呼吸杂志, 2016, 39(4): 241-242. doi: 10.3760/cma.j.issn.1001-0939.2016.04.001
[2] Lim WS, Baudouin SV, George RC, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009[J]. Thorax, 2009, 64(Suppl 3): iii1-iii55.
[3] Ao XX. The epidemiology of hospital death following pediatric severe community acquired pneumonia[J]. Ital J Pediatr, 2021, 47(1): 25. doi: 10.1186/s13052-021-00966-0
[4] 刘慧, 肖新才, 陆剑云, 等. 2009—2012年广州市社区获得性肺炎流行特征和病原学研究[J]. 中华预防医学杂志, 2013, 47(12): 1089-1094. doi: 10.3760/cma.j.issn.0253-9624.2013.12.005
[5] Marrie TJ, Shariatzadeh MR. Community-acquired pneumonia requiring admission to an intensive care unit: a descriptive study[J]. Medicine, 2007, 86(2): 103-111. doi: 10.1097/MD.0b013e3180421c16
[6] Ferreira-Coimbra J, Sarda C, Rello J. Burden of community-acquired pneumonia and unmet clinical needs[J]. Adv Ther, 2020, 37(4): 1302-1318. doi: 10.1007/s12325-020-01248-7
[7] Prower E, Grant D, Bisquera A, et al. The ROX index has greater predictive validity than NEWS2 for deterioration in Covid-19[J]. EClinicalMedicine, 2021, 35: 100828. doi: 10.1016/j.eclinm.2021.100828
[8] Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index[J]. J Crit Care, 2016, 35: 200-205. doi: 10.1016/j.jcrc.2016.05.022
[9] Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy[J]. Am J Respir Crit Care Med, 2019, 199(11): 1368-1376. doi: 10.1164/rccm.201803-0589OC
[10] Chen Z, Yu J, Song YT, et al. Aging Beijing: challenges and strategies of health care for the elderly[J]. Ageing Res Rev, 2010, 9(Suppl 1): S2-S5.
[11] 刘霜, 朱华栋, 于学忠, 等. 经鼻高流量氧疗和无创正压通气对于肺源性中重度急性呼吸窘迫综合征患者初始治疗的效果评价[J]. 临床急诊杂志, 2020, 21(3): 181-187. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202003001.htm
[12] Cutuli SL, Grieco DL, Menga LS, et al. Noninvasive ventilation and high-flow oxygen therapy for severe community-acquired pneumonia[J]. Curr Opin Infect Dis, 2021, 34(2): 142-150. doi: 10.1097/QCO.0000000000000715
[13] Nishikimi M, Nishida K, Shindo Y, et al. Failure of non-invasive respiratory support after 6 hours from initiation is associated with ICU mortality[J]. PLoS One, 2021, 16(4): e0251030. doi: 10.1371/journal.pone.0251030
[14] Vera M, Kattan E, Born P, et al. Intubation timing as determinant of outcome in patients with acute respiratory distress syndrome by SARS-CoV-2 infection[J]. J Crit Care, 2021, 65: 164-169. doi: 10.1016/j.jcrc.2021.06.008
[15] Ferrer M, Travierso C, Cilloniz C, et al. Severe community-acquired pneumonia: characteristics and prognostic factors in ventilated and non-ventilated patients[J]. PLoS One, 2018, 13(1): e0191721. doi: 10.1371/journal.pone.0191721
[16] Zhu YL, Zheng XB, Huang KZ, et al. Mortality prediction using clinical and laboratory features in elderly patients with severe community-acquired pneumonia[J]. Ann Palliat Med, 2021, 10(10): 10913-10921. doi: 10.21037/apm-21-2537
[17] Shashikumar SP, Wardi G, Paul P, et al. Development and prospective validation of a deep learning algorithm for predicting need for mechanical ventilation[J]. Chest, 2021, 159(6): 2264-2273. doi: 10.1016/j.chest.2020.12.009
[18] 吴玉丹, 吴美景, 陈英诗, 等. qSOFA评分、MNA评分联合血清降钙原对老年重症社区获得性肺炎患者的预后预测价值[J]. 中华老年多器官疾病杂志, 2021, 20(7): 488-493. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLQG202107004.htm
[19] Lee H, Kim I, Kang BH, et al. Prognostic value of serial neutrophil-to-lymphocyte ratio measurements in hospitalized community-acquired pneumonia[J]. PLoS One, 2021, 16(4): e0250067. doi: 10.1371/journal.pone.0250067
[20] 张立涛, 马佳倩, 齐惠军, 等. 动脉血乳酸/血清白蛋白比值预测老年重症社区获得性肺炎患者预后的回顾性研究[J]. 临床急诊杂志, 2021, 22(5): 297-300. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202105001.htm
[21] Chandel A, Patolia S, Brown AW, et al. High-Flow Nasal Cannula Therapy in COVID-19: Using the ROX Index to Predict Success. Respir Care[J]. Respir Care, 2021, 66(6): 909-919. doi: 10.4187/respcare.08631
[22] Lee CU, Jo YH, Lee JH, et al. The index of oxygenation to respiratory rate as a prognostic factor for mortality in sepsis[J]. Am J Emerg Med, 2021, 45: 426-432. doi: 10.1016/j.ajem.2020.09.052
[23] Ferrer S, Sancho J, Bocigas I, et al. ROX index as predictor of high flow nasal cannula therapy success in acute respiratory failure due to SARS-CoV-2[J]. Respir Med, 2021, 189: 106638. doi: 10.1016/j.rmed.2021.106638
[24] Patel M, Chowdhury J, Mills N, et al. Utility of the ROX index in predicting intubation for patients with COVID-19-related hypoxemic respiratory failure receiving high-flow nasal therapy: retrospective cohort study[J]. JMIRx Med, 2021, 2(3): e29062. doi: 10.2196/29062
[25] 李玉芳, 李正达, 郭艳霞, 等. ROX指数预测流感相关肺炎患者气管插管的有效性分析[J]. 医学信息, 2022, 35(5): 131-133. https://www.cnki.com.cn/Article/CJFDTOTAL-YXXX202205034.htm
[26] Lemiale V, Dumas G, Demoule A, et al. Performance of the ROX index to predict intubation in immunocompromised patients receiving high-flow nasal cannula for acute respiratory failure[J]. Ann Intensive Care, 2021, 11(1): 17. doi: 10.1186/s13613-021-00801-z
-




 下载:
下载: