Effect of Nicorandil on Tp-Te interval and Tp-Te/QT and prognosis in patients with acute ST-segment elevation myocardial infarction
-
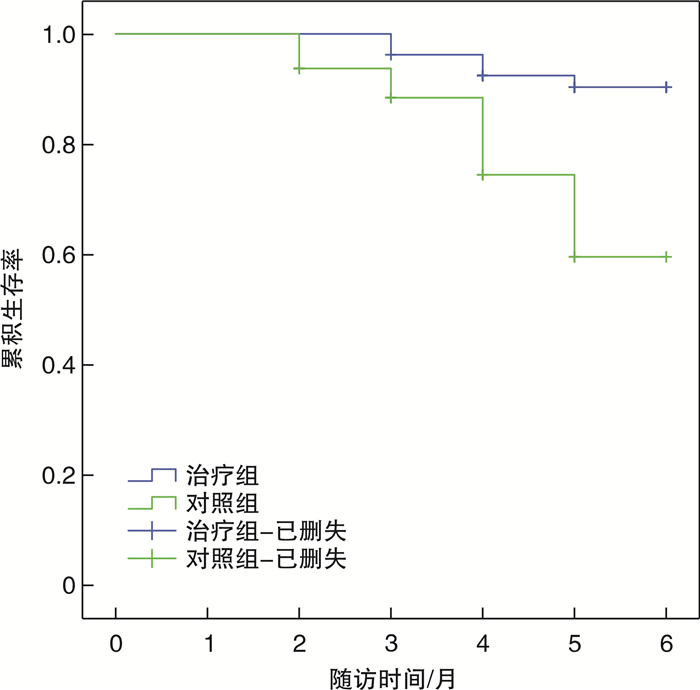
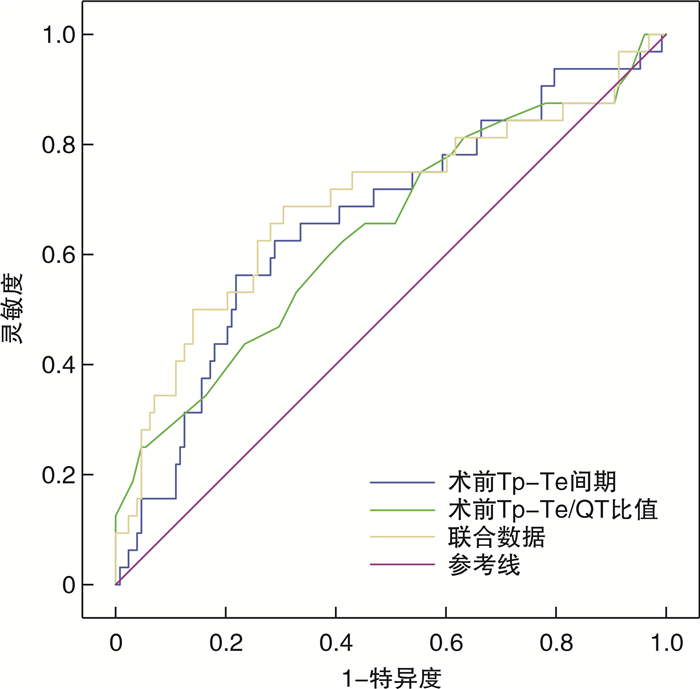
摘要: 目的 分析尼可地尔对急性ST段抬高型心肌梗死(ST-segment elevation myocardial infarction,STEMI)患者Tp-Te间期、Tp-Te/QT及预后的影响。方法 选取2021年9月—2023年1月在潍坊市益都中心医院接受急诊介入治疗的STEMI患者160例,以数表法随机分成治疗组(尼可地尔治疗,80例)和对照组(常规药物治疗,80例);比较两组术前及术后48 h、1周、2周、4周的Tp-Te间期、Tp-Te/QT比值;随访6个月,比较两组主要不良心血管事件(major adverse cardiovascular events,MACE)发生率及全因死亡率,并根据有无MACE发生将患者分成MACE组和无MACE组,比较两组临床资料,分析STEMI预后危险因素。结果 治疗组与对照组Tp-Te间期、Tp-Te/QT比值在时间及组间上,差异有统计学意义(P<0.05);术前,两组Tp-Te间期、Tp-Te/QT比值比较差异无统计学意义(P>0.05);术后48 h、1周、2周、4周,治疗组Tp-Te间期、Tp-Te/QT比值均低于对照组(P<0.05);随访6个月,治疗组MACE共发生10例(12.50%),死亡7例(8.75%),低于对照组的22例(27.50%)和12例(15.00%)(P<0.05)。MACE组射血分数低于无MACE组,术前Tp-Te间期、术前Tp-Te/QT比值高于无MACE组(均P<0.05)。logistic回归分析显示:低射血分数、术前高Tp-Te间期、术前高Tp-Te/QT比值是STEMI预后危险因素(均P<0.05)。ROC分析显示:Tp-Te间期、Tp-Te/QT比值预测MACE的AUC为0.663、0.643,联合预测为0.693。结论 尼可地尔可显著缩短STEMI患者介入术后Tp-Te间期及Tp-Te/QT比值,减少不良心血管事件,改善患者预后。低射血分数、术前高Tp-Te间期、术前高Tp-Te/QT比值与急性STEMI患者术后MACE的发生相关密切,其中Tp-Te间期、Tp-Te/QT比值对STEMI的预后有重要的预警意义。
-
关键词:
- 急性ST段抬高型心肌梗死 /
- 尼可地尔 /
- Tp-Te /
- Tp-Te/QT /
- 预后
Abstract: Objective To analyze the effects of Nicorandil on Tp-Te interval, Tp-Te/QT and prognosis in patients with acute ST-segment elevation myocardial infarction(STEMI).Methods A total of 160 STEMI patients receiving emergency interventional treatment in Yidu Central Hospital of Weifang City from September 2021 to January 2023 were selected and randomly divided into treatment group(Nicorandil treatment, n=80) and control group(conventional drug treatment, n=80) by numerical table method. The Tp-Te interval and Tp-Te/QT ratio before and 48 hours, 1 week, 2 weeks and 4 weeks after operation were compared between the two groups. After 6 months of follow-up, the incidence of major adverse cardiovascular events(MACE) and all-cause mortality were compared between the two groups, and the patients were divided into MACE group and non-MACE group according to the occurrence of MACE. The clinical data of the two groups were compared, and the prognostic risk factors of STEMI were analyzed.Results Tp-Te interval and Tp-Te/QT ratio between treatment group and control group were significantly different(P < 0.05). Before surgery, there was no significant difference in the Tp-Te interval and Tp-Te/QT ratio between the two groups(P > 0.05). At 48 h, 1 week, 2 weeks and 4 weeks after operation, the Tp-Te interval and Tp-Te/QT ratio in the treatment group were lower than those in the control group, there were significantly different in two groups(P < 0.05). After 6 months of follow-up, there were 10 cases(12.50%) of MACE and 7 cases(8.75%) of death in the treatment group, which were lower than 22 cases(27.50%) and 12 cases(15.00%) in the control group, there were significantly different in two groups(P < 0.05). The ejection fraction of MACE group was lower than that of non-MACE group, and the preoperative Tp-Te interval and Tp-Te/QT ratio were higher than those of non-MACE group(P < 0.05). logistic regression analysis showed that low ejection fraction, high preoperative Tp-Te interval and high preoperative Tp-Te/QT ratio were risk factors for STEMI prognosis(all P < 0.05). ROC analysis showed that the AUC of Tp-Te interval and Tp-Te/QT ratio were 0.663 and 0.643 for MACE and 0.693 for combined prediction.Conclusion Nicorandil can significantly shorten the Tp-Te interval and Tp-Te/QT ratio after intervention in STEMI patients, reduce adverse cardiovascular events, and improve the prognosis of patients. Low ejection fraction, high preoperative Tp-Te interval, and high preoperative Tp-Te/QT ratio are closely related to the occurrence of postoperative MACE in acute STEMI patients, and the Tp-Te interval and Tp-Te/QT ratio have important prognostic significance for STEMI.-
Key words:
- acute ST-segment elevation myocardial infarction /
- Nicorandil /
- Tp-Te /
- Tp-Te/QT /
- prognosis
-

-
表 1 治疗组和对照组患者Tp-Te间期比较
X±S 组别 Tp-Te间期/ms 术前 术后48 h 术后1周 术后2周 术后4周 治疗组(80例) 124.05±29.88 114.09±17.31 110.01±14.12 102.55±13.56 98.84±9.96 对照组(80例) 123.74±29.69 120.79±18.04 116.54±15.24 110.65±14.07 106.66±10.11 t 0.066 2.397 2.811 3.708 4.928 P 0.948 0.018 0.006 <0.001 <0.001 F组别/时点/交互 6.748/58.192/1.212 P组别/时点/交互 0.010/<0.001/0.308 表 2 治疗组和对照组患者Tp-Te/QT比值比较
X±S 组别 Tp-Te/QT比值 术前 术后48 h 术后1周 术后2周 术后4周 治疗组(80例) 0.32±0.07 0.29±0.05 0.26±0.04 0.24±0.04 0.21±0.04 对照组(80例) 0.33±0.06 0.32±0.07 0.32±0.05 0.30±0.04 0.28±0.05 t 0.971 3.113 8.440 9.567 9.801 P 0.333 0.002 <0.001 <0.001 <0.001 F组别/时点/交互 50.541/96.199/13.957 P组别/时点/交互 <0.001/<0.001/<0.001 表 3 治疗组和对照组患者MACE发生情况比较
例(%) 组别 例数 室性心律失常 严重心力衰竭 心源性休克 再发急性心肌梗死 MACE总发生 治疗组 80 3(3.75) 2(2.50) 3(3.75) 2(2.50) 10(12.50) 对照组 80 8(10.00) 5(6.25) 5(6.25) 4(5.00) 22(27.50) χ2 - - 5.625 P - - 0.018 表 4 STEMI预后单因素分析
X±S 因素 MACE组(32例) 无MACE组(128例) t/χ2 P 性别/例(%) 0.509 0.476 男 19(59.38) 67(52.34) 女 13(40.62) 61(47.66) 年龄/岁 60.63±9.84 58.21±8.55 1.386 0.168 收缩压基线值/mmHga) 129.94±10.10 130.32±10.15 0.191 0.849 舒张压基线值/mmHg 72.06±7.34 72.54±7.96 0.307 0.759 高脂血症/例(%) 0.059 0.808 是 13(40.63) 49(38.28) 否 19(59.37) 79(61.72) 糖尿病史/例(%) 0.122 0.727 是 10(31.25) 36(28.13) 否 22(68.75) 92(71.87) 冠心病史/例(%) 0.035 0.853 是 8(25.00) 30(23.44) 否 24(75.00) 98(76.56) Killip分级/例(%) 3.669 0.055 Ⅰ~Ⅱ级 24(75.00) 113(88.28) Ⅲ~Ⅳ级 8(25.00) 15(11.72) 射血分数/% 50.88±6.14 58.65±5.16 7.333 <0.001 术前Tp-Te间期/ms 136.68±29.45 120.70±28.99 2.780 0.006 术后4周Tp-Te间期/ms 104.34±9.97 102.35±10.93 0.937 0.350 术前Tp-Te/QT比值 0.35±0.07 0.32±0.06 2.758 0.007 术后4周Tp-Te/QT比值 0.26±0.07 0.24±0.05 1.777 0.077 a)1 mmHg=0.133 kPa。 表 5 STEMI预后多因素logistic回归分析
因素 B 标准误 Wald 自由度 P Exp(B) 95%CI 射血分数 0.264 0.050 28.392 1 <0.001 1.302 1.182~1.435 术前Tp-Te间期 -0.019 0.007 7.075 1 0.008 0.981 0.967~0.995 术前Tp-Te/QT比值 -8.662 3.277 6.986 1 0.008 <0.001 0.000~0.107 表 6 Tp-Te间期、Tp-Te/QT比值预测STEMI患者预后的效能分析
参数 AUC 标准误 P 95%CI 截断值 约登指数 灵敏度/% 特异度/% Tp-Te间期 0.663 0.056 0.004 0.553~0.772 148.84 0.344 56.3 78.1 Tp-Te/QT比值 0.643 0.058 0.012 0.529~0.758 0.34 0.211 62.5 58.6 联合 0.693 0.059 0.001 0.578~0.808 0.79 0.383 68.8 69.5 -
[1] 曹蕊, 李俊峡, 韩硕, 等. 心电图Tp-Te间期、Tp-Te/QT比值与恶性室性心律失常的关系[J]. 中国循证心血管医学杂志, 2021, 13(3): 366-368. https://www.cnki.com.cn/Article/CJFDTOTAL-PZXX202103027.htm
[2] 林茹秀, 符艾文, 欧哲聪. 心电图Tp-Te、Tp-Tec、QTc、Tp-Te/QT比值与AMI病人急性期发生室性心律失常的相关性[J]. 中西医结合心脑血管病杂志, 2021, 19(14): 2403-2405. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202114024.htm
[3] Zhu H, Xu X, Fang X, et al. Effects of the Antianginal Drugs Ranolazine, Nicorandil, and Ivabradine on Coronary Microvascular Function in Patients With Nonobstructive Coronary Artery Disease: A Meta-analysis of Randomized Controlled Trials[J]. Clin Ther, 2019, 41(10): 2137-2152.e12. doi: 10.1016/j.clinthera.2019.08.008
[4] 黄静静, 陈浩, 李霖睿, 等. 麝香保心丸联合冠脉内注射尼可地尔对STEMI患者PPCI术后心肌血流灌注及近期预后的影响[J]. 药学实践杂志, 2022, 40(1): 79-83 https://www.cnki.com.cn/Article/CJFDTOTAL-YXSJ202201014.htm
[5] 赵倜. 口服尼可地尔联合瑞替普酶溶栓治疗对急性ST段抬高型心肌梗死患者TIMI血流分级及血清心肌酶水平的影响[J]. 检验医学与临床, 2021, 18(24): 3623-3625. https://www.cnki.com.cn/Article/CJFDTOTAL-JYYL202124034.htm
[6] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南[J]. 中华心血管病杂志, 2010, 38(8): 675-690. doi: 10.3760/cma.j.issn.0253-3758.2010.08.002
[7] Aker A, Saliba W, Schnaider S, et al. The Impact of Smoking Status 1 Year After ST-Segment Elevation Myocardial Infarction on Cardiovascular Events and Mortality in Patients Aged=60 Years[J]. Am J Cardiol, 2022, 175: 52-57. doi: 10.1016/j.amjcard.2022.04.019
[8] 郭福佳, 袁正强, 施尚鹏, 等. 早发与晚发冠心病患者临床及冠状动脉病变特点的性别差异分析[J]. 临床心血管病杂志, 2021, 37(1): 28-31. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202101006.htm
[9] Dharma S, Dakota I, Andriantoro H, et al. Association of gender with clinical outcomes of patients with acute ST-segment elevation myocardial infarction presenting with acute heart failure[J]. Coron Artery Dis, 2021, 32(1): 17-24.
[10] 刘安恒, 李利军, 王莹, 等. 早期应用尼可地尔对STEMI患者行急诊介入治疗中慢血流的预防价值[J]. 中国循证心血管医学杂志, 2022, 14(1): 75-78 https://www.cnki.com.cn/Article/CJFDTOTAL-PZXX202201017.htm
[11] 李彬彬, 徐锋, 王景武, 等. 尼可地尔联合PCI对STEMI患者心肌血流灌注, 心功能和预后的影响[J]. 川北医学院学报, 2023, 38(5): 692-696. https://www.cnki.com.cn/Article/CJFDTOTAL-NOTH202305027.htm
[12] Matsumoto H, Mikuri M, Masaki R, et al. Feasibility of intracoronary nicorandil for inducing hyperemia on fractional flow reserve measurement: Comparison with intracoronary papaverine[J]. Int J Cardiol, 2020, 314: 1-6.
[13] 岳慧娟, 杨盼盼, 王昆阳. 静脉注射尼可地尔对不稳定型心绞痛患者PCI术后心脏自主神经功能和心肌微循环的影响[J]. 中国循证心血管医学杂志, 2021, 13(11): 1383-13861389. https://www.cnki.com.cn/Article/CJFDTOTAL-PZXX202111025.htm
[14] Sánchez-Duarte S, Márquez-Gamiño S, Montoya-Pérez R, et al. Nicorandil Decreases Oxidative Stress in Slow and Fast Twitch Muscle Fibers of Diabetic Rats by Improving the Glutathione System Functioning[J]. J Diabet Invest, 2021.
[15] 徐启明, 刘军华, 苏红英, 等. 尼可地尔对抑郁模型大鼠心肌K_(ATP)通道的影响[J]. 中西医结合心脑血管病杂志, 2021, 19(8): 1300-1303. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202108012.htm
[16] Maslov L, Popov S, Naryzhnaya N, et al. KATP channels are regulators of programmed cell death and targets for creation of novel drugs against ischemia/reperfusion cardiac injury. [J]. Fundam Clin Pharmacol, 2023: 12924.
[17] 李阳春, 张敏, 雷蓉. 扩张型心肌病预警恶性心律失常的心电指标Tp-Te间期与左室射血分数的相关性分析[J]. 中西医结合心脑血管病杂志, 2022, 20(14): 2619-2623. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202214025.htm
[18] 刘晓慧, 闫兴国, 张学萍. AMI病人心电图Tp-Te、Tp-Te/QT与室性心律失常及心功能的关系[J]. 中西医结合心脑血管病杂志, 2022, 20(13): 2491-2493. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202213041.htm
[19] 曹蕊, 李俊峡, 韩硕, 等. 心电图Tp-Te间期、Tp-Te/QT比值与恶性室性心律失常的关系[J]. 中国循证心血管医学杂志, 2021, 13(3): 366-368 https://www.cnki.com.cn/Article/CJFDTOTAL-PZXX202103027.htm
[20] Wang W, Zhang X, Chen K, et al. Effects of nicorandil infusion on ECG parameters in patients with unstable angina pectoris and percutaneous coronary intervention[J]. Ann Noninvasive Electrocardiol, 2020, 25(4): e12736.
[21] 刘明涛. 尼可地尔在ST段抬高型心肌梗死患者介入治疗中对患者微血管功能障碍的影响[J]. 中国药物与临床, 2021, 21(22): 3712-3714 https://www.cnki.com.cn/Article/CJFDTOTAL-YWLC202122026.htm
[22] 卢昊阳, 戎成振, 肖慧, 等. 冠脉内注射用尼可地尔联合稳心颗粒对STEMI患者PCI术后MACE发生率及相关预后指标的影响[J]. 安徽医科大学学报, 2022, 57(8): 1323-1327. https://www.cnki.com.cn/Article/CJFDTOTAL-YIKE202208028.htm
[23] 尤红俊, 赵倩倩, 任淑婷, 等. 基于高通量测序数据挖掘探讨小鼠射血分数保留心力衰竭的发病机制[J]. 中西医结合心脑血管病杂志, 2022, 20(22): 4102-4109. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYY202222012.htm
[24] 赵丹莉, 王宪沛, 张智文, 等. 频发房性期前收缩与老年急性ST段抬高型心肌梗死患者新发心房颤动的关系及其预测价值研究[J]. 临床心血管病杂志, 2021, 37(1): 57-61. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202101013.htm
[25] 朱明辉, 杨磊, 殷珺妹, 等. QTc、Tp-Tec间期联合血清CTRP9水平对急性心肌梗死后室性心律失常发生的预测价值[J]. 山东医药, 2022, 62(13): 24-28. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202213004.htm
-




 下载:
下载: