The predictive value of systemic immune inflammation index for early acute kidney injury in patients undergoing adult cardiac surgery with cardiopulmonary bypass
-
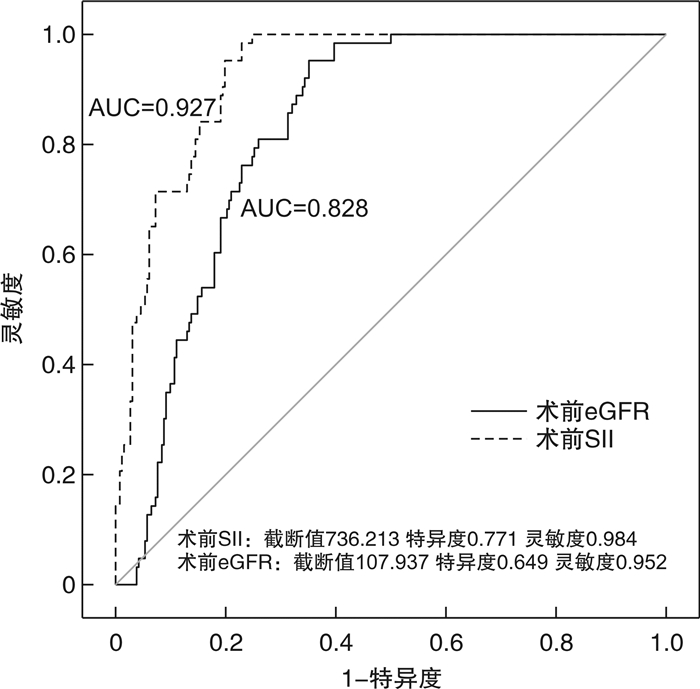
摘要: 目的 探讨全身免疫炎症指数(systemic immune-inflammation index,SII)对成人体外循环心脏术后早期急性肾损伤(acute kidney injury,AKI)的预测价值。方法 回顾性收集2020年1月—2021年12月在南京医科大学第一附属医院接受体外循环成人心脏手术患者的临床资料,按照术后48 h内是否发生AKI,分为AKI组和非AKI组。最终共325例患者纳入本研究,其中术后48 h内发生AKI的患者共63例纳入AKI组,AKI发生率19.4%,其余262例纳入非AKI组。分析比较两组患者的临床资料,采用多元逐步logistic回归分析成人体外循环心脏手术术后发生AKI的独立危险因素,并使用ROC曲线分析SII对术后早期AKI的预测价值。结果 AKI组和非AKI组患者在高血压病史、服用利尿剂、术前SII、血清尿素氮、手术持续时间、估算的肾小球滤过率(estimated glomerular filtration rate,eGFR)、术后机械通气时间、体外循环持续时间、术中失血量和术后24 h尿量等方面比较均差异有统计学意义(均P<0.05),多因素logistic分析显示体外循环持续时间、术前SII和eGFR是术后AKI的独立危险因素(P<0.05)。ROC曲线分析显示,术前SII和eGFR预测术后AKI的AUC分别为0.927(95%CI:1.009~1.041)和0.828(95%CI:0.959~0.998),对应的灵敏度分别为98.4%和95.2%,特异度分别为77.1%和64.9%。结论 术前SII是成人体外循环心脏外科术后发生AKI的独立危险因素,术前及时评估SII对预测AKI的发生具有非常好的价值。Abstract: Objective To investigate the predictive value of the systemic immune-inflammation index(SII) for early acute kidney injury(AKI) in adult patients after cardiac surgery with cardiopulmonary bypass.Methods Clinical data of adult patients undergoing cardiac surgery with cardiopulmonary bypass in the First Affiliated Hospital of Nanjing Medical University from January 2020 to December 2021 were retrospectively collected. Patients were grouped into AKI group and non-AKI group according to whether AKI occurred within 48 hours after surgery. Clinical information of the two groups were researched and compared. Multivariate logistic regression was used to analyze independent risk factors for postoperative AKI after cardiopulmonary bypass surgery. Receiver operating characteristic(ROC) curve was used to investigate the value of SII in predicting the occurrence of AKI.Results A total of 325 patients were involved in this research, among which, 63 patients with postoperative AKI within 48 hours were included in the AKI group, with an incidence of 19.4%, and the remaining 262 patients were grouped in the non-AKI group. There were statistical significance in the history of hypertension, the history of taking diuretics, preoperative SII, plasma urea nitrogen, estimated glomerular filtration rate(eGFR), duration of operation, extracorporeal circulation time, intraoperative blood loss, duration of mechanical ventilation time, and postoperative 24-hour urine volume between the two group, there were significantly different in two groups(all P < 0.05). Multiple-factor logistic analysis revealed that extracorporeal circulation time, preoperative SII and eGFR were independent risk factors for postoperative AKI after cardiopulmonary bypass surgery(P < 0.05). ROC curve analysis demonstrated that the AUC of preoperative SII and eGFR in predicting postoperative AKI after cardiopulmonary bypass surgery were 0.927(95%CI: 1.009-1.041), and 0.828(95%CI: 0.959-0.998), the corresponding sensitivity was 98.4% and 95.2% respectively, and the specificity was 77.1% and 64.9%, severally.Conclusion Preoperative SII is an independent risk factor for postoperative AKI after cardiopulmonary bypass surgery and timely assessment of preoperative SII is of great value in predicting the occurrence of AKI in adult patients undergoing cardiac surgery with cardiopulmonary bypass.
-

-
表 1 两组患者临床情况比较
X±S,M(P25,P75) 项目 AKI组(63例) 对照组(262例) 统计值 P 性别/例 2.381 0.123 男 43 151 女 20 111 年龄/岁 61.5±11.2 60.3±10.4 0.82 0.413 机械通气时间/h 6(3,9) 2(1,4) 4388 <0.001 吸烟史/例 3.05 0.081 有 20 56 无 43 206 高血压/例 112/150 4.243 0.039 有 36 112 无 27 150 糖尿病/例 3.398 0.065 有 3 34 无 60 228 利尿剂/例 10.323 0.001 有 27 170 无 36 92 收缩压/mmHga) 135.0±22.4 129.7±18.3 1.737 0.086 舒张压/mmHg 75.7±13.9 75.7±13.4 0.018 0.986 术前血红蛋白/(g/L) 134.9±20.3 136.4±15.9 0.511 0.611 术前SII 1 192.5±412.6 405.8±194.3 14.747 <0.001 术前尿素氮/(mmol/L) 7.3±2.7 6.5±1.7 2.253 0.027 术前eGFR/(mL/min/1.73 m2) 68.7(54.9,81.8) 205.7(88.3,375.7) 13.874 <0.001 手术持续时间/h 6.8±2.2 5.6±1.4 3.994 <0.001 体外循环时间/h 3.2±1.1 2.6±0.9 3.718 <0.001 术中最大量去甲肾上腺素/(μg/kg/min) 0.02(0.00,0.04) 0.02(0.00,0.06) 8 062 0.807 术中出血量/mL 1 000(800,1 500) 800(600,1 000) 5 945.5 0.001 术后24 h尿量/mL 1 430(535,2 220) 2 317(1 900,2 832) 4 256.5 <0.001 a)1 mmHg=0.133 kPa。 表 2 多因素logistic回归分析
项目 β SE Wald P OR(95%CI) 术前SII 0.025 0.008 9.221 0.002 1.025(1.009~1.041) 术前eGFR -0.022 0.01 4.761 0.029 0.978(0.959~0.998) 体外循环时间 2.895 1.451 3.982 0.046 18.087(1.053~310.738) -
[1] 吴婷婷, 王红, 邵涓涓, 等. 尿酸对非体外循环冠状动脉旁路移植术后急性肾损伤的影响[J]. 中华胸心血管外科杂志, 2019, 35(5): 294-298. doi: 10.3760/cma.j.issn.1001-4497.2019.05.009
[2] Yuan SM. Acute Kidney Injury after Cardiac Surgery: Risk Factors and Novel Biomarkers[J]. Braz J Cardiovasc Surg, 2019, 34(3): 352-360.
[3] 谢彩蝶, 刘康, 严陈燕, 等. 尿胰岛素样生长因子结合蛋白7和金属蛋白酶2组织抑制剂联合检测对心脏术后急性肾损伤早期诊断及预后的价值[J]. 中华肾脏病杂志, 2021, 37(2): 95-104. doi: 10.3760/cma.j.cn441217-20200326-00017
[4] Maekawa H, Inagi R. Pathophysiological Role of Organelle Stress/Crosstalk in AKI-to-CKD Transition[J]. Semin Nephrol, 2019, 39(6): 581-588. doi: 10.1016/j.semnephrol.2019.10.007
[5] Li Q, Shi S, Lu X, et al. Effect of kidney disease on all-cause and cardiovascular mortality in patients undergoing coronary angiography[J]. Ren Fail, 2023, 45(1): 2195950. doi: 10.1080/0886022X.2023.2195950
[6] Kemmner S, Bachmann Q, Steiger S, et al. STAT1 regulates macrophage number and phenotype and prevents renal fibrosis after ischemia-reperfusion injury[J]. Am J Physiol Renal Physiol, 2019, 316(2): F277-F291. doi: 10.1152/ajprenal.00004.2018
[7] Chen X, Zhou J, Fang M, et al. Procalcitonin, Interleukin-6 and C-reactive Protein Levels Predict Renal Adverse Outcomes and Mortality in Patients with Acute Type A Aortic Dissection[J]. Front Surg, 2022, 9: 902108. doi: 10.3389/fsurg.2022.902108
[8] Tian BW, Yang YF, Yang CC, et al. Systemic immune-inflammation index predicts prognosis of cancer immunotherapy: systemic review and meta-analysis[J]. Immunotherapy, 2022, 14(18): 1481-1496. doi: 10.2217/imt-2022-0133
[9] Li X, Gu L, Chen Y, et al. Systemic immune-inflammation index is a promising non-invasive biomarker for predicting the survival of urinary system cancers: a systematic review and meta-analysis[J]. Ann Med, 2021, 53(1): 1827-1838. doi: 10.1080/07853890.2021.1991591
[10] Liu X, Guan G, Cui X, et al. Systemic Immune-Inflammation Index(SII)Can Be an Early Indicator for Predicting the Severity of Acute Pancreatitis: A Retrospective Study[J]. Int J Gen Med, 2021, 14: 9483-9489. doi: 10.2147/IJGM.S343110
[11] Schoppmann SF, Jomrich G. Response to the Comment on "High Systemic Immune-inflammation Index Is an Adverse Prognostic Factor for Patients With Gastroesophageal Adenocarcinoma"[J]. Ann Surg, 2021, 274(6): e669-e670. doi: 10.1097/SLA.0000000000003681
[12] 李峰, 刘春生. 全身免疫炎症指数对重症胰腺炎并发急性肾损伤早期预测价值的研究[J]. 临床急诊杂志, 2022, 23(2): 100-105. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.02.005
[13] 申国旗, 马凯, 李晶, 等. 全身免疫炎症指数与非ST段抬高型急性冠脉综合征患者PCI治疗后对比剂诱导急性肾损伤相关性分析[J]. 江苏医药, 2022, 48(4): 375-380. https://www.cnki.com.cn/Article/CJFDTOTAL-YIYA202204013.htm
[14] Khwaja A. KDIGO clinical practice guidelines for acute kidney injury[J]. Nephron Clin Pract, 2012, 120(4): c179-84. doi: 10.1159/000339789
[15] Prowle JR, Forni LG, Bell M, et al. Postoperative acute kidney injury in adult non-cardiac surgery: joint consensus report of the Acute Disease Quality Initiative and PeriOperative Quality Initiative[J]. Nat Rev Nephrol, 2021, 17(9): 605-618. doi: 10.1038/s41581-021-00418-2
[16] 杨晓梅, 王春生, 刘岚, 等. 成人体外循环心脏手术后急性肾损伤的危险因素分析[J]. 中华胸心血管外科杂志, 2013, 29(3): 147-150. https://www.cnki.com.cn/Article/CJFDTOTAL-WUXB202107017.htm
[17] Rubino AS, De Santo LS, Montella AP, et al. Prognostic Implication of Preoperative Anemia in Redo Cardiac Surgery: A Single-Center Propensity-Matched Analysis[J]. J Cardiovasc Dev Dis, 2023, 10(4).
[18] Karkouti K, Wijeysundera DN, Yau TM, et al. Influence of erythrocyte transfusion on the risk of acute kidney injury after cardiac surgery differs in anemic and nonanemic patients[J]. Anesthesiology, 2011, 115(3): 523-530. doi: 10.1097/ALN.0b013e318229a7e8
[19] Amini S, Najafi MN, Karrari SP, et al. Risk Factors and Outcome of Acute Kidney Injury after Isolated CABG Surgery: a Prospective Cohort Study[J]. Braz J Cardiovasc Surg, 2019, 34(1): 70-75.
[20] Jia L, Li C, Bi X, et al. Prognostic Value of Systemic Immune-Inflammation Index among Critically Ill Patients with Acute Kidney Injury: A Retrospective Cohort Study[J]. J Clin Med, 2022, 11(14).
[21] Tadagavadi R, Reeves WB. Neutrophils in cisplatin AKI-mediator or marker?[J]. Kidney Int, 2017, 92(1): 11-13. doi: 10.1016/j.kint.2017.03.023
[22] Jansen M, Florquin S, Roelofs J. The role of platelets in acute kidney injury[J]. Nat Rev Nephrol, 2018, 14(7): 457-471. doi: 10.1038/s41581-018-0015-5
[23] Wu M, Luan YY, Lu JF, et al. Platelet count as a new biomarker for acute kidney injury induced by hemorrhagic shock[J]. Platelets, 2020, 31(1): 94-102. doi: 10.1080/09537104.2019.1581921
[24] Godi I, De Rosa S, Martino F, et al. Urinary[TIMP-2]x[IGFBP7]and serum procalcitonin to predict and assess the risk for short-term outcomes in septic and non-septic critically ill patients[J]. Ann Intensive Care, 2020, 10(1): 46.
[25] Jiang H, Li D, Xu T, et al. Systemic Immune-Inflammation Index Predicts Contrast-Induced Acute Kidney Injury in Patients Undergoing Coronary Angiography: A Cross-Sectional Study[J]. Front Med(Lausanne), 2022, 9: 841601.
[26] Massoth C, Zarbock A. Diagnosis of Cardiac Surgery-Associated Acute Kidney Injury[J]. J Clin Med, 2021, 10(16).
[27] 罗卫红, 李佳欣, 蒋建平, 等. 急性肾损伤进展至慢性肾脏病的临床特征和危险因素——前瞻性、观察性队列研究[J]. 中华肾脏病杂志, 2020, 36(8): 625-630.
-




 下载:
下载: