Construction of a risk score model for prognosis in pre-hospital emergency patients based on plasma soluble urokinase plasminogen activator receptor levels
-
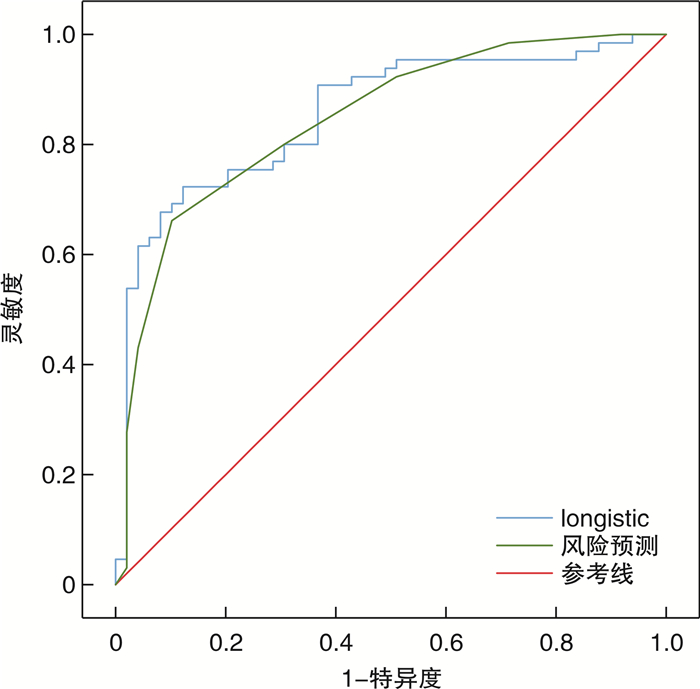
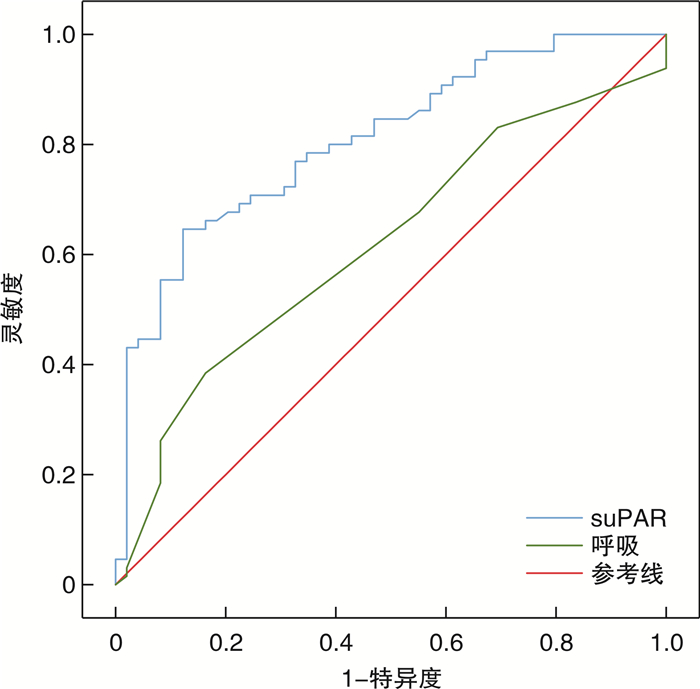
摘要: 目的 研究院前急救患者的血清可溶性尿激酶型纤溶酶原激活物受体(soluble urokinase plasminogen activator receptor,suPAR)水平和变化规律,构建基于血清suPAR水平的院前急诊患者病情预测的风险评分模型。方法 选取2022年4月—2022年7月陆军军医大学第一附属医院120救护车接诊的114例患者作为研究对象,收集患者基本特征数据、生命体征及suPAR血清值,并对其进行7 d的短期随访。根据患者入院后最终是否收入重症监护室分为危重组和非危重组,比较2组间suPAR水平及其他因素的差别,应用多因素logistic回归分析院前急救患者病情预测的影响因素,根据回归方程建立logistic回归模型,并对多因素分析有意义的指标赋分建立院前急救患者病情预测的风险评分模型,采用受试者工作特征(ROC)曲线确定模型的最佳截断值并评估其应用价值。结果 危重组的suPAR血清水平、男性占比、呼吸频率、意识水平明显高于非危重组,危重组的收缩压、GCS评分低于非危重组,差异有明显统计学意义(P < 0.05)。多因素分析提示呼吸频率、收缩压、suPAR、GCS评分是院前急救患者病情的预测影响因素,其中suPAR(OR=4.808,95%CI:2.269~10.189,P < 0.05)和呼吸频率(OR=1.231,95%CI:1.015~1.493,P < 0.05)是院前急救患者病情预测的独立危险因素。logistic回归模型对院前急救患者病情预测的ROC曲线下面积为0.854(95%CI:0.783~0.925),灵敏度、特异度分别为69.1%,91.7%。建立的病情预测风险评分模型对院前急救患者病情预测的ROC曲线下面积为0.845(95%CI:0.773~0.916),灵敏度、特异度分别为66.2%,89.8%,最佳截断值为5.5分。2种模型对院前急救患者病情预测的ROC曲线下面积的比较,差异无统计学意义(Z=0.411,P>0.05)。结论 血清suPAR水平测定可作为一种独立风险因子预测院前急救患者病情的危重性,建立的风险评分模型对院前急救患者病情预测具有良好的应用价值,其分值的高低与疾病严重程度密切相关,分值为5.5分可作为区分危重和非危重的最佳截断点。
-
关键词:
- 院前急救 /
- 可溶性尿激酶型纤溶酶原激活物受体 /
- 风险评分模型 /
- 危险因素 /
- 病情预测
Abstract: Objective To study serum Soluble urokinase plasminogen activator receptor(suPAR) levels and patterns of change in pre-hospital emergency patients; and to construct a risk scoring model for predicting the conditions of pre-hospital emergency patients based on serum suPAR levels.Methods A total of 114 patients received by 120 ambulances in the First Affiliated Hospital of Army Military Medical University from April 2022 to July 2022 were selected as the objects of study, collected the patient's characteristic data, vital signs and the serum values of suPAR, and was followed for 7 days of short-term follow-up. According to whether the patients were finally admitted to the intensive care unit, they were divided into critical group and non-critical group, to compare the differences between the two groups in suPAR levels and other factors, multivariate logistic regression was used to analyze the influencing factors of prehospital emergency patients for condition prediction, The logistic regression model was built according to the regression equation, To assign points to meaningful indicators in multivariate analysis for establish a risk score model for the condition prediction of prehospital emergency patients. The receiver operating characteristic(ROC) curve was used to determine the best cutoff of the model and evaluate its application.Results The serum level of suPAR, percentage of males, respiratory rate, and level of consciousness were significantly higher in the critical group than in the non-critical group, and the systolic blood pressure and GCS score were lower in the critical group than in the non-critical group, with statistically significant differences (P < 0.05).Multivariate analysis showed that respiratory rate, systolic pressure, suPAR, and GCS scores were the factors affecting the prediction of pre-hospital emergency patients, among which suPAR(OR=4.808, 95%CI: 2.269-10.189, P < 0.05) and respiratory rate(OR=1.231, 95%CI: 1.015-1.493, P < 0.05) were independent risk factors affecting the prognosis of pre-hospital emergency patients, and the sensitivity of suPAR in predicting prehospital emergency patients as critically ill patients was 0.646, the specificity was 0.878, the Youden's index was 0.524, and the area under the ROC curve(AUC) was 0.807, P < 0.05.The area under the ROC curve(AUC) predicted by logistic regression model for pre-hospital emergency patients was 0.854(95%CI: 0.783-0.925), and the sensitivity and specificity were 69.1% and 91.7%, respectively. The area under the ROC curve of the multi-index risk scoring model for the prediction of the condition of pre-hospital emergency patients was 0.845(95%CI: 0.773-0.916), and the sensitivity and specificity were 66.2% and 89.8%, respectively. The optimal cut-off is 5.5 points. There was no significant difference in the area under the ROC curve of the two prediction models for the prediction of pre-hospital emergency patients(Z=0.411, P>0.05).Conclusion Measurement of serum suPAR level can be used as an independent risk factor to predict the criticality of pre-hospital emergency patients, and the established risk scoring model has a good application value for predicting the condition of pre-hospital emergency patients, and its score is closely related to the severity of the disease, and a score of 5.5 can be used as the best cut-off to distinguish critical from non-critical. -

-
表 1 非危重组和危重组的基本特征和临床资料比较
指标 非重症组
(49例)重症组
(65例)χ2/t P 性别/例(%) 12.473(χ2) < 0.001 女 28(57.0) 16(24.0) 男 21(42.0) 49(75.0) 年龄/岁 62.67± 15.46 61.79± 15.65 0.725(t) 0.470 合并创伤/例(%) 0.978(χ2) 0.323 是 7(14.0) 14(21.0) 否 42(86.0) 51(79.0) 表 2 院前急救患者早期预后影响因素的单因素分析
指标 非重症组(49例) 重症组(65例) χ2/t/z P 呼吸频率/(次/min) 21(18~28) 21(0~28) -2.033(z) 0.042 收缩压/mmHg 140±26.42 129.84±33.85 2.362(t) 0.020 体温/℃ 36.7(36.3~39) 36.7(35~39.4) -1.119(z) 0.263 心率/(次/min) 86(47~155) 93(55~151) 1.807(z) 0.071 指氧饱和度/% 98(82~100) 97(68~100) -1.961(z) 0.050 意识/分 0(0~2) 0(0~3) 3.211(z) 0.001 GCS评分/分 15(7~15) 15(3~15) -2.953(z) 0.003 suPAR/(ng/mL) 2.32(1.06~10.81) 3.71(1.89~31.64) -5.592(z) < 0.001 心电图/% 1.440(χ2) 0.230 异常 27(55.0) 43(66) 正常 22(45.0) 50(34) 注:1 mmHg=0.133 kPa。 表 3 院前急救患者病情预测的多因素分析
相关因素 β SE Wald P OR 95%CI 呼吸 0.208 0.098 4.479 0.034 1.231 1.015~1.493 收缩压 -0.026 0.012 4.810 0.028 0.974 0.952~0.997 suPAR 1.570 0.383 16.797 < 0.001 4.808 2.269~10.189 GCS评分 -0.379 0.110 11.887 0.001 0.684 0.552~0.849 -
[1] Eugen-Olsen J, Giamarellos-Bourboulis EJ. suPAR: The unspecific marker for disease presence, severity and prognosis[J]. Int J Antimicrob Agents, 2015, 46(Suppl 1): S33-34.
[2] Rasmussen LJ, Ladelund S, Haupt TH, et al. Soluble urokinase plasminogen activator receptor(suPAR)in acute care: a strong marker of disease presence and severity, readmission and mortality. A retrospective cohort study[J]. Emerg Med J, 2016, 33(11): 769-775. doi: 10.1136/emermed-2015-205444
[3] Nasr El-Din A, Abdel-Gawad AR, Abdelgalil W, et al. Evaluation of sTREM1 and suPAR Biomarkers as Diagnostic and Prognostic Predictors in Sepsis Patients[J]. Infect Drug Resist, 2021, 14: 3495-3507. doi: 10.2147/IDR.S314237
[4] Rasmussen LJH, Petersen JEV, Eugen-Olsen J. Soluble Urokinase Plasminogen Activator Receptor(suPAR)as a Biomarker of Systemic Chronic Inflammation[J]. Front Immunol, 2021, 12: 780641. doi: 10.3389/fimmu.2021.780641
[5] Dowsett J, Ferkingstad E, Rasmussen LJH, et al. Eleven genomic loci affect plasma levels of chronic inflammation marker soluble urokinase-type plasminogen activator receptor[J]. Commun Biol, 2021, 4(1): 655. doi: 10.1038/s42003-021-02144-8
[6] Schrauben SJ, Shou H, Zhang X, et al. Association of Multiple Plasma Biomarker Concentrations with Progression of Prevalent Diabetic Kidney Disease: Findings from the Chronic Renal Insufficiency Cohort(CRIC)Study[J]. J Am Soc Nephrol, 2021, 32(1): 115-126. doi: 10.1681/ASN.2020040487
[7] Frary CE, Blicher MK, Olesen T B, et al. Circulating biomarkers for long-term cardiovascular risk stratification in apparently healthy individuals from the MONICA 10 cohort[J]. Eur J Prev Cardiol, 2020, 27(6): 570-578. doi: 10.1177/2047487319885457
[8] Ozdirik B, Maibier M, Scherf M, et al. Soluble Urokinase Plasminogen Activator Receptor Levels Are Associated with Severity of Fibrosis in Patients with Primary Sclerosing Cholangitis[J]. J Clin Med, 2022, 11(9): 2479. doi: 10.3390/jcm11092479
[9] Hayek SS, Leaf DE, Samman Tahhan A, et al. Soluble Urokinase Receptor and Acute Kidney Injury[J]. N Engl J Med, 2020, 382(5): 416-426. doi: 10.1056/NEJMoa1911481
[10] Velissaris D, Dimopoulos G, Parissis J, et al. Prognostic Role of Soluble Urokinase Plasminogen Activator Receptor at the Emergency Department: A Position Paper by the Hellenic Sepsis Study Group[J]. Infect Dis Ther, 2020, 9(3): 407-416. doi: 10.1007/s40121-020-00301-w
[11] Schultz M, Rasmussen LJH, Kallemose T, et al. Availability of suPAR in emergency departments may improve risk stratification: a secondary analysis of the TRIAGE Ⅲ trial[J]. Scand J Trauma Resusc Emerg Med, 2019, 27(1): 43. doi: 10.1186/s13049-019-0621-7
[12] Isola G, Polizzi A, Alibrandi A, et al. Independent impact of periodontitis and cardiovascular disease on elevated soluble urokinase-type plasminogen activator receptor(suPAR)levels[J]. J Periodontol, 2021, 92(6): 896-906. doi: 10.1002/JPER.20-0242
[13] Iversen E, Houlind MB, Kallemose T, et al. Elevated suPAR Is an Independent Risk Marker for Incident Kidney Disease in Acute Medical Patients[J]. Front Cell Dev Biol, 2020, 8: 339. doi: 10.3389/fcell.2020.00339
[14] Rovina N, Akinosoglou K, Eugen-Olsen J, et al. Soluble urokinase plasminogen activator receptor(suPAR)as an early predictor of severe respiratory failure in patients with COVID-19 pneumonia[J]. Crit Care, 2020, 24(1): 187. doi: 10.1186/s13054-020-02897-4
[15] 赵胤杰, 李杨, 沈亚静, 等. 血浆可溶性尿激酶型纤溶酶原激活物受体在急诊严重创伤患者病情评估中的应用研究[J]. 临床急诊杂志, 2021, 22(2): 82-86. doi: 10.13201/j.issn.1009-5918.2021.02.001 https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2021.02.001
[16] Haupt TH, Petersen J, Ellekilde G, et al. Plasma suPAR levels are associated with mortality, admission time, and Charlson Comorbidity Index in the acutely admitted medical patient: a prospective observational study[J]. Crit Care, 2012, 16(4): R130. doi: 10.1186/cc11434
[17] Rasmussen LJH, Ladelund S, Haupt TH, et al. Combining National Early Warning Score With Soluble Urokinase Plasminogen Activator Receptor(suPAR)Improves Risk Prediction in Acute Medical Patients: A Registry-Based Cohort Study[J]. Crit Care Med, 2018, 46(12): 1961-1968. doi: 10.1097/CCM.0000000000003441
[18] Alstrup M, Meyer J, Schultz M, et al. Soluble Urokinase Plasminogen Activator Receptor(suPAR)as an Added Predictor to Existing Preoperative Risk Assessments[J]. World J Surg, 2019, 43(3): 780-790. doi: 10.1007/s00268-018-4841-1
[19] Thuno M, Macho B, Eugen-Olsen J. suPAR: the molecular crystal ball[J]. Dis Markers, 2009, 27(3): 157-172.
[20] Ljunggren M, Castren M, Nordberg M, et al. The association between vital signs and mortality in a retrospective cohort study of an unselected emergency department population[J]. Scand J Trauma Resusc Emerg Med, 2016, 24: 21. doi: 10.1186/s13049-016-0213-8
[21] Lamantia MA, Stewart PW, Platts-Mills TF, et al. Predictive value of initial triage vital signs for critically ill older adults[J]. West J Emerg Med, 2013, 14(5): 453-460. doi: 10.5811/westjem.2013.5.13411
[22] 牟雪枫, 时彦莹, 郭伟, 等. NEWS评分对急诊抢救室患者7 d全因死亡率预警能力的评价[J]. 临床急诊杂志, 2021, 22(4): 246-251.
-




 下载:
下载: