Risk factors for urosepsis in patients with ureteral calculi complicated with acute pyelonephritis
-
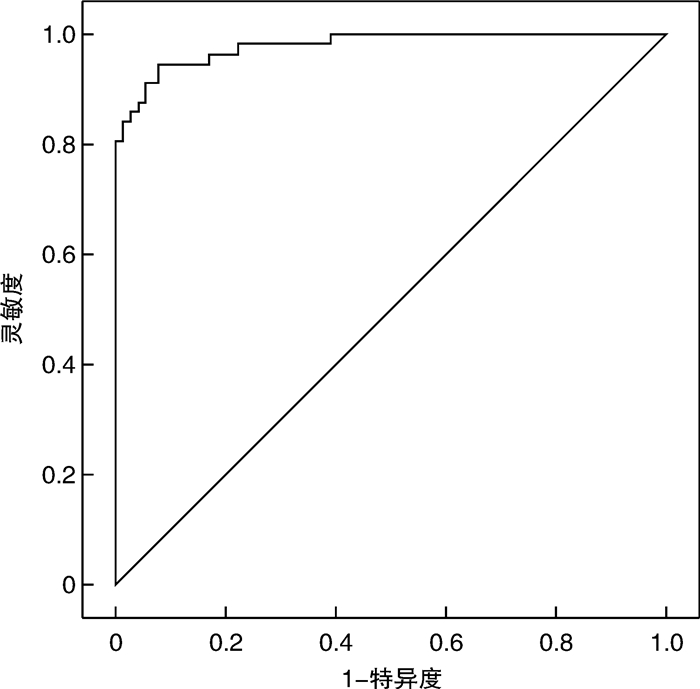
摘要: 目的 探讨输尿管结石合并APN患者进展为尿脓毒症的危险因素,为临床识别高危患者提供线索。方法 回顾性收集2014年8月—2022年11月期间承德市中心医院收治的输尿管结石合并APN患者的临床资料,根据患者是否发生脓毒症组分为病例组和对照组,分别对性别、年龄、BMI、既往病史、结石特点、实验室资料、APACHEⅡ评分等影响因素进行单因素分析,并对单因素分析中具有统计学意义的变量进行多因素分析。结果 输尿管结石合并APN患者发生尿脓毒症的比例为42.5%。单因素分析发现结石最大长径、结石最大横径、血WBC、Lymph#、Neut#、Neut%、Hb、RDW、PLT、MPV、血Na+、PT、PTA、INR、ALB、TBIL、DBIL、SCR、尿培养、NLR、RPR、MLR、RAR、APACHEⅡ评分等差异具有统计学意义(P < 0.05);多因素分析发现结石最大长径>10.0 mm(P=0.026)、TBIL>20.4 μmol/L(P=0.003)、SCR>106 μmol/L(P < 0.001)、PLT较低(P < 0.001)、RAR(P=0.018)以及APACHEⅡ评分(P=0.001)较高是输尿管结石合并APN患者进展为尿脓毒症的独立危险因素。结论 输尿管结石合并APN患者发生尿脓毒症的比例为42.5%。在输尿管结石合并APN的患者中,结石较大、TBIL、SCR、RAR以及APACHEⅡ评分较高、PLT较低是其进展为尿脓毒症的独立危险因素。
-
关键词:
- 输尿管结石 /
- 急性肾盂肾炎 /
- 尿脓毒症 /
- 危险因素 /
- 红细胞分布宽度与白蛋白比值
Abstract: Objective To explore the risk factors of urosepsis in patients with ureteral calculi complicated with APN and to provide clues for clinical identification of high-risk patients.Methods Clinical data of patients with ureteral calculi complicated with APN treated in Chengde Central Hospital during the priod of August 2014 to November 2022 were collected retrospectively. Patients with sepsis were divided into case group and control group according to whether sepsis occurred. Univariate analysis was performed on sex, age, BMI, previous medical history, stone characteristics, laboratory data, APACHEⅡ score and other influencing factors, and multivariate analysis was performed on the statistically significant variables in univariate analysis.Results The incidence of urinary sepsis in patients with ureteral calculi complicated with APN was 42.5%. In the univariate analysis, variables have statistically significant in maximum length diameter, maximum transverse diameter, blood leukocyte count, Lymph#, Neut#, Neut%, Hb, RDW, PLT, MPV, serum sodium, PT, PTA, INR, ALB, TBIL, DBIL, creatinine, urine culture, NLR, RPR, MLR, RAR, APACHEⅡ scores. Multifactorial analysis revealed that maximum stone length>10.0 mm(P=0.026), total bilirubin>20.4 μmol/L(P=0.003), creatinine>106 μmol/L(P < 0.001), lower platelet count(P < 0.001), RAR(P=0.018), and higher APACHEⅡ score(P=0.001) were independent risk factors for progression to urosepsis in patients with ureteral calculi complicated with APN.Conclusion The percentage of patients with ureteral calculi complicated with APN who developed urosepsis was 42.5%. In patients with ureteral stones combined with APN, larger stones, higher total bilirubin as well as creatinine, RAR, and APACHEⅡ scores, and lower PLT were independent risk factors for progression to urinary sepsis. -

-
表 1 两组患者一般资料的单因素分析
例(%) 项目 脓毒症组
(57例)非脓毒症组
(77例)t/F/χ2 P 性别 2.136 0.144 男 11(19.3) 8(10.4) 女 46(80.7) 69(89.6) 年龄/岁 1.760 0.185 <60 29(50.9) 48(62.3) ≥60 28(49.1) 29(37.7) BMI/(kg/m2) 0.674 0.412 <24.0 27(47.4) 31(40.3) ≥24.0 30(52.6) 46(59.7) 结石手术史 0.318 0.573 有 11(19.3) 12(15.6) 无 46(80.7) 65(84.4) 高血压 0.724 0.395 有 21(36.8) 34(44.2) 无 36(63.2) 43(55.8) 糖尿病 0.105 0.746 有 17(29.8) 21(27.3) 无 40(70.2) 56(72.7) 冠心病 0.687 0.407 有 6(10.5) 4(5.2) 无 51(89.5) 73(94.8) 表 2 两组患者结石相关资料的单因素分析
例(%) 项目 脓毒症组
(57例)非脓毒症组
(77例)t/F/χ2 P 结石部位 0.958 0.619 上段 35(61.4) 52(67.5) 中段 6(10.5) 9(11.7) 下段 16(28.1) 16(20.8) 结石患侧 2.963 0.085 左侧 33(57.9) 33(42.9) 右侧 24(42.1) 44(57.1) 同侧肾结石 0.001 0.992 有 23(40.4) 31(40.3) 无 34(59.6) 46(59.7) 最大长径/mm 5.466 0.019 ≤10.0 32(56.1) 58(75.3) >10.0 25(43.9) 19(24.7) 最大横径/mm 6.356 0.012 ≤6.5 23(40.4) 48(62.3) >6.5 34(59.6) 29(37.7) 表 3 两组患者实验室相关资料的单因素分析
X±S,M(P25,P75),例(%) 项目 脓毒症组(57例) 非脓毒症组(77例) t/F/χ2 P 血常规 WBC/(×109/L) 15.5±6.9 13.0±4.6 -2.304 0.023 Lymph#/(×109/L) 0.68(0.38,0.87) 1.01(0.61,1.46) 1271.000 < 0.001 Mono#/(×109/L) 0.73(0.36,0.97) 0.67(0.50,1.00) 2131.500 0.777 Neut#/(×109/L) 13.40±6.48 10.92±4.36 -2.506 0.014 Neut% 89.6(86.5,91.8) 84.6(80.9,88.2) 1162.000 < 0.001 Hb/(g/L) 116(106,126) 122(114,131) 1697.000 0.025 HCT/(L/L) 0.351±0.052 0.364±0.049 1.562 0.121 RDW/% 13.4(12.3,14.9) 12.3(11.4,13.7) 1638.000 0.012 PLT/(×109/L) 135±63 224±78 7.070 < 0.001 MPV/fL 8.6(7.8,9.5) 7.9(7.3,8.7) 1540.500 0.003 血Na+/(mmol/L) 136(133,138) 138(136,140) 1469.000 0.001 血K+/(mmol/L) 3.40(3.10,3.95) 3.47(3.06,3.78) 2165.500 0.896 PT/s 13.1(12.4,14.6) 12.5(11.8,13.5) 1596.500 0.007 PTA/% 79(72,89) 86(77,95) 1636.000 0.012 INR 1.15(1.09,1.27) 1.10(1.03,1.18) 1562.500 0.004 APTT/s 30.0(28.0,32.7) 29.3(27.5,30.9) 1866.000 0.139 FIB/(g/L) 5.73(4.22,7.17) 4.90(4.33,6.45) 2024.500 0.444 ALB/(g/L) 8.524 0.004 ≤30 36(63.2) 29(37.7) >30 21(36.8) 48(62.3) TBIL/(μmol/L) 6.964 0.008 ≤20.4 41(71.9) 69(89.6) >20.4 16(28.1) 8(10.4) DBIL/(μmol/L) 9.284 0.002 ≤6.8 38(66.7) 68(88.3) >6.8 19(33.3) 9(11.7) SCR/(μmol/L) 64.617 < 0.001 ≤106 14(24.6) 71(92.2) >106 43(75.4) 6(7.8) 尿潜血 0.234 0.629 <2+ 17(29.8) 26(33.8) ≥2+ 40(70.2) 51(66.2) 尿亚硝酸盐 1.927 0.165 阴性 35(61.4) 56(72.7) 阳性 22(38.6) 21(27.3) 尿WBC 0.532 0.466 <2+ 18(31.6) 29(37.7) ≥2+ 39(68.4) 48(62.3) 尿培养 8.874 0.003 阳性 34(59.6) 26(33.8) 阴性 23(40.4) 51(66.2) 表 4 两组患者衍生指标的单因素分析
M(P25,P75) 项目 脓毒症组(57例) 非脓毒症组(77例) t/F/χ2 P NLR 20.88(12.42,28.27) 10.54(6.23,14.55) 1066.000 < 0.001 PLR 211.11(126.32,302.89) 211.17(146.02,314.12) 2049.000 0.513 RPR 0.10(0.08,0.16) 0.06(0.04,0.07) 749.000 < 0.001 MLR 1.02(0.55,1.52) 0.68(0.37,1.14) 1533.500 0.003 RAR 0.45(0.39,0.52) 0.39(0.34,0.53) 1425.500 0.001 APACHEⅡ评分 9(8,14) 6(5,9) 898.000 < 0.001 表 5 输尿管结石合并APN患者发生脓毒症的多因素分析结果
影响因素 β P OR 95%CI 结石最大长径 1.908 0.026 6.738 1.250~36.335 PLT -0.028 < 0.001 0.972 0.959~0.986 TBIL 4.113 0.003 61.101 4.040~924.203 SCR 5.061 < 0.001 157.749 15.933~1 561.823 RAR 10.550 0.018 38 164.832 6.319~230 491 354.100 APACHEⅡ评分 0.583 0.001 1.791 1.254~2.558 常量 -18.971 < 0.001 < 0.001 - -
[1] Belyayeva M, Jeong JM. Acute Pyelonephritis[M]. StatPearls. Treasure Island(FL): StatPearls Publishing Copyright© 2023, StatPearls Publishing LLC, 2023.
[2] Bonkat G, Bartoletti R, Bruyère F, et al. EAU Guidelines on Urological Infections[J]. 2023.
[3] Yoo KH, Choi T, Lee HL. Blood culture for complicated acute pyelonephritis with ureteral stone: are they unnecessary?[J]. Infect Dis (Lond), 2019, 51(1): 75-76. doi: 10.1080/23744235.2018.1510184
[4] Umbehr MH, Müntener M. [Urinary stone disease-size isn't all that matters][J]. Ther Umsch, 2021, 78(5): 215-221. doi: 10.1024/0040-5930/a001263
[5] Grossmann NC, Schuettfort VM, Betschart J, et al. Risk factors for concomitant positive midstream urine culture in patients presenting with symptomatic ureterolithiasis[J]. Urolithiasis, 2022, 50(3): 293-302. doi: 10.1007/s00240-022-01323-4
[6] Srougi V, Moscardi PR, Marchini GS, et al. Septic Shock Following Surgical Decompression of Obstructing Ureteral Stones: A Prospective Analysis[J]. J Endourol, 2018, 32(5): 446-450. doi: 10.1089/end.2017.0896
[7] Lu X, Zhou B, Hu D, et al. Emergency decompression for patients with ureteral stones and SIRS: a prospective randomized clinical study[J]. Ann Med, 2023, 55(1): 965-972. doi: 10.1080/07853890.2023.2169343
[8] Chugh S, Pietropaolo A, Montanari E, et al. Predictors of Urinary Infections and Urosepsis After Ureteroscopy for Stone Disease: a Systematic Review from EAU Section of Urolithiasis(EULIS)[J]. Curr Urol Rep, 2020, 21(4): 16. doi: 10.1007/s11934-020-0969-2
[9] Jarry É, Garot M, Marlière F, et al. Predictive factors of postoperative septic complications after flexible ureteroscopy for urinary stones[J]. Prog Urol, 2022, 32(2): 85-91. doi: 10.1016/j.purol.2021.07.010
[10] Yamamichi F, Shigemura K, Kitagawa K, et al. Comparison between non-septic and septic cases in stone-related obstructive acute pyelonephritis and risk factors for septic shock: A multi-center retrospective study[J]. J Infect Chemother, 2018, 24(11): 902-906. doi: 10.1016/j.jiac.2018.08.002
[11] Kakinoki H, Tobu S, Kakinoki Y, et al. Risk Factors for Uroseptic Shock in Patients with Urolithiasis-Related Acute Pyelonephritis[J]. Urol Int, 2018, 100(1): 37-42. doi: 10.1159/000481801
[12] Abi Tayeh G, Safa A, Sarkis J, et al. Determinants of pyelonephritis onset in patients with obstructive urolithiasis[J]. Urologia, 2022, 89(1): 100-103. doi: 10.1177/03915603211035244
[13] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[14] Yue S, Li S, Huang X, et al. Construction and Validation of a Risk Prediction Model for Acute Kidney Injury in Patients Suffering from Septic Shock[J]. Dis Markers, 2022, 2022: 9367873.
[15] 王友铭, 许长宝, 王晓甫, 等. 河南省泌尿系结石住院患者流行病学特点及分析[J]. 临床泌尿外科杂志, 2021, 36(6): 458-463. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202106007.htm
[16] Lee SH, Choi T, Choi J, et al. Differences between Risk Factors for Sepsis and Septic Shock in Obstructive Urolithiasis[J]. J Korean Med Sci, 2020, 35(43): e359. doi: 10.3346/jkms.2020.35.e359
[17] Jeon K, Na SJ, Oh DK, et al. Characteristics, management and clinical outcomes of patients with sepsis: a multicenter cohort study in Korea[J]. Acute Crit Care, 2019, 34(3): 179-191. doi: 10.4266/acc.2019.00514
[18] Pietropaolo A, Geraghty RM, Veeratterapillay R, et al. A Machine Learning Predictive Model for Post-Ureteroscopy Urosepsis Needing Intensive Care Unit Admission: A Case-Control YAU Endourology Study from Nine European Centres[J]. J Clin Med, 2021, 10(17): 388.
[19] Liu M, Zhu Z, Cui Y, et al. Correction to: The value of procalcitonin for predicting urosepsis after mini-percutaneous nephrolithotomy or flexible ureteroscopy based on different organisms[J]. World J Urol, 2022, 40(2): 529-535. doi: 10.1007/s00345-021-03845-9
[20] Partin AW, Dmochowski RR, Kavoussi LR, et al. Campbell-Walsh-Wein Urology[M]. 12th ed. Philadelphia: Elsevier, 2021.
[21] 苏晓伟, 王大明, 丁德茂, 等. 感染性结石的相关临床易感因素研究[J]. 临床泌尿外科杂志, 2021, 36(4): 284-287. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMW202104008.htm
[22] Kino M, Hayashi T, Hino D, et al. Patients' poor performance status is an independent risk factor for urosepsis induced by kidney and ureteral stones[J]. Urolithiasis, 2021, 49(5): 477-484. doi: 10.1007/s00240-021-01256-4
[23] Zhao L, Zhao L, Wang YY, et al. Platelets as a prognostic marker for sepsis: A cohort study from the MIMIC-Ⅲ database[J]. Medicine(Baltimore), 2020, 99(45): e23151.
[24] Jiang L, Lin SH, Wang J, et al. Prognostic values of procalcitonin and platelet in the patient with urosepsis[J]. Medicine(Baltimore), 2021, 100(27): e26555.
[25] Jacobi J. The pathophysiology of sepsis-2021 update: Part 1, immunology and coagulopathy leading to endothelial injury[J]. Am J Health Syst Pharm, 2022, 79(5): 329-337. doi: 10.1093/ajhp/zxab380
[26] Christensen MG, Johnsen N, Skals M, et al. Prevention of P2 Receptor-Dependent Thrombocyte Activation by Pore-Forming Bacterial Toxins Improves Outcome in A Murine Model of Urosepsis[J]. Int J Mol Sci, 2020, 21(16): 5652. doi: 10.3390/ijms21165652
[27] Efat A, Shoeib S, Ebrahim E, et al. Impact of indirect bilirubin and uric acid on outcomes of sepsis-associated acute kidney injury(sAKI)[J]. Int Urol Nephrol, 2022, 54(11): 3009-3016. doi: 10.1007/s11255-022-03232-2
[28] Wu Y, Huang S, Chang X. Understanding the complexity of sepsis mortality prediction via rule discovery and analysis: a pilot study[J]. BMC Med Inform Decis Mak, 2021, 21(1): 334. doi: 10.1186/s12911-021-01690-9
[29] Wang S, Feng R, Wang SS, et al. FOXA2 prevents hyperbilirubinaemia in acute liver failure by maintaining apical MRP2 expression[J]. Gut, 2023, 72(3): 549-559. doi: 10.1136/gutjnl-2022-326987
[30] Wagner M, Zollner G, Trauner M. Nuclear receptors in liver disease[J]. Hepatology(Baltimore, Md), 2011, 53(3): 1023-1034.
[31] Yue S, Li S, Huang X, et al. Machine learning for the prediction of acute kidney injury in patients with sepsis[J]. J Transl Med, 2022, 20(1): 215. doi: 10.1186/s12967-022-03364-0
[32] de Oliveira FS, Freitas FG, Ferreira EM, et al. Positive fluid balance as a prognostic factor for mortality and acute kidney injury in severe sepsis and septic shock[J]. J Crit Care, 2015, 30(1): 97-101. doi: 10.1016/j.jcrc.2014.09.002
[33] Kuwabara S, Goggins E, Okusa MD. The Pathophysiology of Sepsis-Associated AKI[J]. Clin J Am Soc Nephrol, 2022, 17(7): 1050-1069. doi: 10.2215/CJN.00850122
[34] Poston JT, Koyner JL. Sepsis associated acute kidney injury[J]. BMJ, 2019, 364: k4891.
[35] Wang TH, Hsu YC. Red Cell Distribution Width as a Prognostic Factor and Its Comparison with Lactate in Patients with Sepsis[J]. Diagnostics(Basel), 2021, 11(8): 1474.
[36] Deniz M, Ozgun P, Ozdemir E. Relationships between RDW, NLR, CAR, and APACHE Ⅱ scores in the context of predicting the prognosis and mortality in ICU patients[J]. Eur Rev Med Pharmacol Sci, 2022, 26(12): 4258-4267.
[37] Bujak K, Wasilewski J, Osadnik T, et al. The Prognostic Role of Red Blood Cell Distribution Width in Coronary Artery Disease: A Review of the Pathophysiology[J]. Dis Markers, 2015, 2015: 824624.
[38] Pstras L, Waniewski J, Lindholm B. Transcapillary transport of water, small solutes and proteins during hemodialysis[J]. Sci Rep, 2020, 10(1): 18736. doi: 10.1038/s41598-020-75687-1
[39] Bihari S, Bannard-Smith J, Bellomo R. Albumin as a drug: its biological effects beyond volume expansion[J]. Crit Care Resusc, 2020, 22(3): 257-265.
[40] Omiya K, Sato H, Sato T, et al. Albumin and fibrinogen kinetics in sepsis: a prospective observational study[J]. Crit Care, 2021, 25(1): 436. doi: 10.1186/s13054-021-03860-7
[41] Ertekin B, Acar T. The Relationship Between Prognosis and Red Cell Distribution Width(RDW)and RDW-Albumin Ratio(RAR)in Patients with Severe COVID-19 Disease[J]. Int J Gen Med, 2022, 15: 8637-8645. doi: 10.2147/IJGM.S392453
[42] Ni Q, Wang X, Wang J, et al. The red blood cell distribution width-albumin ratio: A promising predictor of mortality in heart failure patients-A cohort study[J]. Clin Chim Acta, 2022, 527: 38-46. doi: 10.1016/j.cca.2021.12.027
[43] Jian L, Zhang Z, Zhou Q, et al. Red Cell Distribution Width/Albumin Ratio: A Predictor of In-Hospital All-Cause Mortality in Patients with Acute Myocardial Infarction in the ICU[J]. Int J Gen Med, 2023, 16: 745-756. doi: 10.2147/IJGM.S393393
[44] Huang Y, Jiang S, Li W, et al. Establishment and Effectiveness Evaluation of a Scoring System-RAAS(RDW, AGE, APACHE Ⅱ, SOFA)for Sepsis by a Retrospective Analysis[J]. J Inflamm Res, 2022, 15: 465-474. doi: 10.2147/JIR.S348490
[45] Lorente L, Martín MM, Argueso M, et al. Association between red blood cell distribution width and mortality of COVID-19 patients[J]. Anaesth Crit Care Pain Med, 2021, 40(1): 100777. doi: 10.1016/j.accpm.2020.10.013
[46] Kharaba A, Algethamy H, Hussein MA, et al. Predictors of survival from Acinetobacter in Saudi Arabian intensive care units: A prospective, one-year, six-city, ten-center cohort study[J]. J Infect Public Health, 2022, 15(6): 677-684. doi: 10.1016/j.jiph.2022.05.007
-




 下载:
下载: