Evaluation of the prognostic value of qSOFA score combined with shock index in patients with sepsis
-
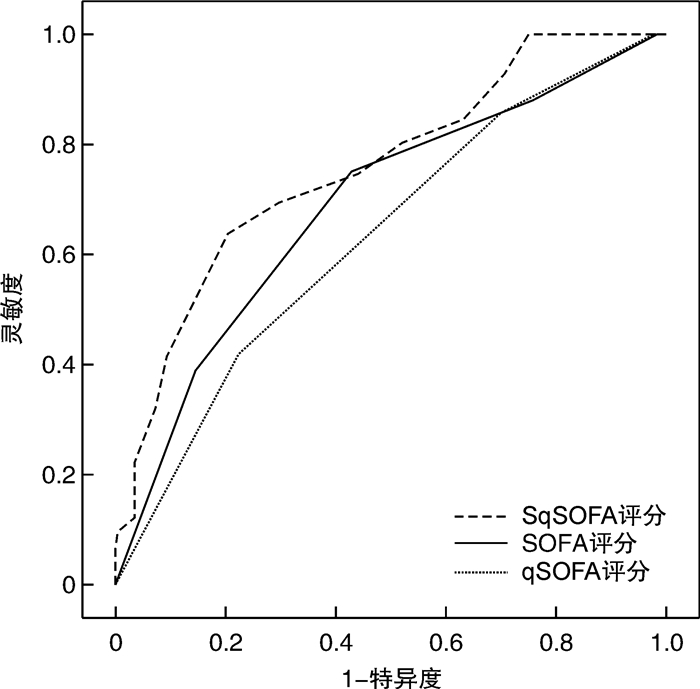
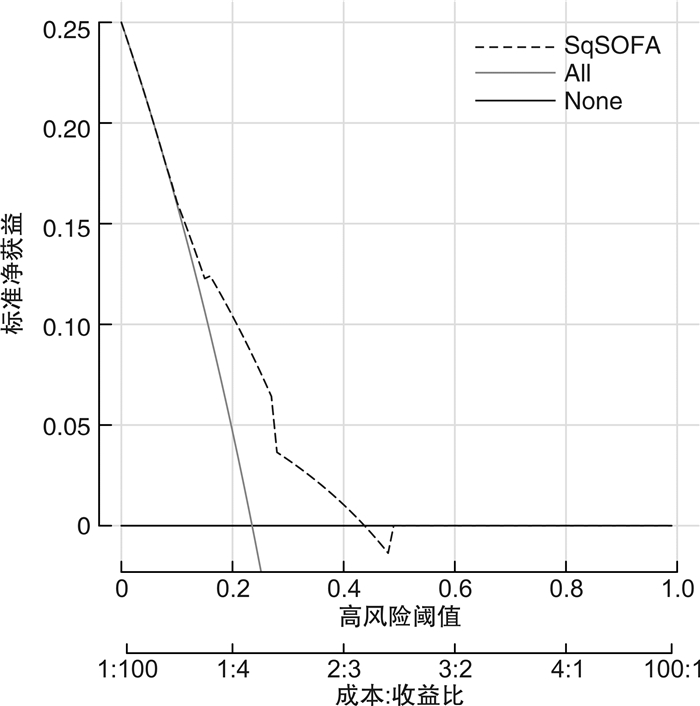
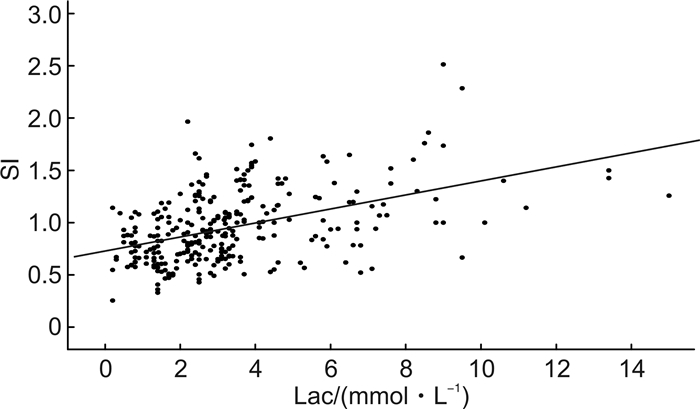
摘要: 目的 探讨快速序贯器官衰竭(qSOFA)评分联合休克指数(SI)在预测脓毒症患者预后的价值。方法 回顾性队列研究,收集3家区域医疗中心收治的306例脓毒症患者的临床资料,根据患者住院期间生存状态分存活组和死亡组,使用受试者工作曲线下面积(AUC)和决策曲线分析(DCA)评价qSOFA评分联合SI评估患者预后的价值。结果 SI与乳酸呈正相关(r=0.465,P < 0.001)。SI的最佳截断值为1.0,SI≥1.0为1分,联合qSOFA评分形成SqSOFA评分,其预测患者的预后AUC是0.694(95%CI:0.639~0.745),优于qSOFA评分0.631(95%CI:0.574~0.685),差异有统计学意义(Z=3.867,P < 0.001),决策曲线分析显示SqSOFA评分具有较好的临床应用效能。结论 qSOFA评分联合SI评估脓毒症患者住院病死率有一定价值。
-
关键词:
- 脓毒症 /
- 评分 /
- 休克指数 /
- 快速序贯器官衰竭评分
Abstract: Objective To explore the value of qSOFA score combined with shock index(SI) in predicting the prognosis of sepsis patients.Methods A retrospective cohort study from three regional medical centers collected clinical data of 306 sepsis patients, followed up the patients' survival status during hospitalization and divided them into a survival group and a death group. Assessing the efficacy of the combined qSOFA score and SI in predicting patient prognosis using the area under the receiver operating curve(AUC) and decision curve analysis(DCA).Results SI was positively correlated with lactate(r=0.465, P < 0.001). The optimal cut-off value for SI was 1.0, and a SI ≥1.0 was 1 point combined with the qSOFA score to form the SqSOFA score. AUC of SqSOFA score was 0.694(95%CI: 0.639-0.745), which was better than qSOFA score of 0.631(95%CI: 0.574-0.685), and the difference was statistically significant(Z=3.867, P < 0.001). Decision curve analysis showed that SqSOFA had high clinical benefit in the test group.Conclusion qSOFA score combined with SI has a certain value in predicting in-hospital mortality in sepsis patients.-
Key words:
- sepsis /
- score /
- shock index /
- quick sequential organ failure assessment
-

-
表 1 脓毒症患者存活组和死亡组基线资料的比较
例(%),X±S 基线资料 存活组(n=234) 死亡组(n=72) χ2/t P 年龄/岁 66.56±13.71 72.19±10.29 3.220 0.001 性别(男/女) 147/87 42/30 0.469 0.493 基础疾病 高血压 74(31.62) 22(30.56) 0.029 0.864 冠状动脉粥样硬化性心脏病 48(20.51) 26(36.11) 7.306 0.007 慢性阻塞性肺疾病 53(22.65) 23(31.94) 2.548 0.110 脑血管疾病 35(14.96) 17(23.61) 2.923 0.087 2型糖尿病 54(23.08) 15(20.83) 0.159 0.690 慢性肾脏疾病 21(8.97) 8(11.11) 0.293 0.588 感染部位 肺部 116(49.57) 33(45.83) 0.308 0.579 腹腔 48(20.51) 23(31.94) 4.038 0.044 泌尿系统 55(23.50) 8(11.11) 5.172 0.023 血源性 4(1.71) 3(4.17) 0.591 0.442 皮肤软组织 10(4.27) 2(2.78) 0.050 0.822 其他 1(0.43) 3(4.17) 3.421 0.064 急诊首诊生命体征 T/℃ 36.87±0.61 36.64±0.85 2.444 0.015 HR/(次·min-1) 105.04±26.34 112.57±30.83 2.034 0.043 RR/(次·min-1) 21.59±5.46 23.54±5.58 2.643 0.009 SBP/mmHg 109.35±24.30 120.64±24.10 3.470 0.001 DBP/mmHg 63.56±15.79 68.43±15.91 2.278 0.023 实验室检查 WBC/(×109·L-1) 14.12±6.44 16.28±10.78 2.088 0.038 Hb/(g·L-1) 115.95±26.30 108.92±24.76 2.011 0.045 PLT/(×109·L-1) 183.86±84.02 181.01±113.51 0.230 0.818 BUN/(mmol·L-1) 10.64±6.84 14.36±8.11 3.845 < 0.001 Cr/(mmol·L-1) 115.24±86.15 155.65±108.78 3.262 0.001 TBIL/(μmol·L-1) 13.02±5.82 21.55±11.25 8.491 < 0.001 ALB/(g·L-1) 31.21±6.12 28.47±5.46 3.387 0.001 Lac/(mmol·L-1) 2.86±1.80 4.72±3.22 6.217 < 0.001 qSOFA评分/分 1.91±0.76 2.28±0.70 3.707 < 0.001 SOFA评分/分 6.75±3.54 10.76±4.62 7.797 < 0.001 SI 0.91±0.31 1.08±0.39 3.805 < 0.001 表 2 脓毒症患者不同SI截断值的Youden指数
Cutoff值 灵敏度/% 特异度/% 阳性似然比 阴性似然比 Youden指数 0.7 79.17 27.78 1.10 0.75 0.0695 0.8 70.83 39.32 1.17 0.74 0.1015 0.9 63.89 53.85 1.38 0.67 0.1774 1.0 54.17 69.66 1.79 0.66 0.2383 1.1 43.06 77.35 1.90 0.74 0.2041 1.2 33.33 82.48 1.90 0.81 0.1581 1.3 26.39 89.32 2.47 0.82 0.1571 表 3 SI及Lac对脓毒症患者住院病死率的预测价值
参数 AUC 95%CI Cutoff值 灵敏度/% 特异度/% 阳性似然比 阴性似然比 约登指数 SI 0.626 0.570~0.681 >1.0 54.17 69.66 1.79 0.66 0.2383 Lac 0.679 0.623~0.731 >4.7 40.28 90.17 4.10 0.66 0.3045 表 4 3种评分对脓毒症患者住院病死率预测能力的比较
参数 AUC 95%CI 最佳诊断阈值 灵敏度/% 特异度/% 阳性似然比 阴性似然比 约登指数 SqSOFA评分 0.694 0.639~0.745 >2 75.00 58.97 1.83 0.42 0.3397 qSOFA评分 0.631 0.574~0.685 >2 41.67 77.78 1.88 0.75 0.1944 SOFA评分 0.758 0.706~0.804 >9 63.89 79.49 3.11 0.45 0.4338 -
[1] 张琼, 梁哲, 苑艺, 等. 血清淀粉样蛋白A结合qSOFA评分对脓毒性休克的预测价值研究[J]. 临床急诊杂志, 2019, 20(12): 971-975. doi: 10.13201/j.issn.1009-5918.2019.12.013
[2] 张健峰, 顾晓蕾, 李斌, 等. 血乳酸联合qSOFA评分对早期筛选诊断脓毒症患者的价值[J]. 临床急诊杂志, 2021, 22(5): 344-347. doi: 10.13201/j.issn.1009-5918.2021.05.011
[3] Ueno R, Masubuchi T, Shiraishi A, et al. Quick sequential organ failure assessment score combined with other sepsis-related risk factors to predict in-hospital mortality: Post-hoc analysis of prospective multicenter study data[J]. PLoS One, 2021, 16(7): e0254343. doi: 10.1371/journal.pone.0254343
[4] Suttapanit K, Wisan M, Sanguanwit P, et al. Prognostic accuracy of VqSOFA for predicting 28-day mortality in patients with suspected sepsis in the emergency department[J]. Shock, 2021, 56(3): 368-373.
[5] Liu SJ, He CQ, He WL, et al. Lactate-enhanced-qSOFA(LqSOFA)score is superior to the other four rapid scoring tools in predicting in-hospital mortality rate of the sepsis patients[J]. Ann Transl Med, 2020, 8(16): 1013. doi: 10.21037/atm-20-5410
[6] Sinto R, Suwarto S, Lie KC, et al. Prognostic accuracy of the quick Sequential Organ Failure Assessment(qSOFA)-lactate criteria for mortality in adults with suspected bacterial infection in the emergency department of a hospital with limited resources[J]. Emerg Med J, 2020, 37(6): 363-369. doi: 10.1136/emermed-2018-208361
[7] 姜辉, 杨柳, 向洁, 等. 休克指数与血气乳酸水平预测院前创伤性休克患者预后的对比分析[J]. 临床急诊杂志, 2022, 23(2): 95-99. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.02.004
[8] Gupta S, Alam A. Shock index is better than conventional vital signs for assessing higher level of care and mortality in severe sepsis or shock[J]. Am J Emerg Med, 2021, 46: 545-549. doi: 10.1016/j.ajem.2020.11.014
[9] Shahid W, Noman A, Sidra S, et al. Shock index as a predictor of hyperlactatemia for early detection of severe sepsis in patients presenting to the emergency department of A low to middle income country[J]. J Ayub Med Coll Abbottabad, 2020, 32(4): 465-469.
[10] Althunayyan SM, Alsofayan YM, Khan AA. Shock index and modified shock index as triage screening tools for sepsis[J]. J Infect Public Health, 2019, 12(6): 822-826. doi: 10.1016/j.jiph.2019.05.002
[11] Koch E, Lovett S, Nghiem T, et al. Shock index in the emergency department: utility and limitations[J]. Open Access Emerg Med, 2019, 11: 179-199. doi: 10.2147/OAEM.S178358
[12] Sheng Y, Zheng WL, Shi QF, et al. Clinical characteristics and prognosis in patients with urosepsis from intensive care unit in Shanghai, China: a retrospective bi-centre study[J]. BMC Anesthesiol, 2021, 21(1): 296. doi: 10.1186/s12871-021-01520-5
[13] Shi QF, Xu Y, Zhang BY, et al. External validation and comparison of two versions of simplified sequential organ failure assessment scores to predict prognosis of septic patients[J]. Int J Clin Pract, 2021, 75(12): e14865.
[14] Jayaprakash N, Gajic O, Frank RD, et al. Elevated modified shock index in early sepsis is associated with myocardial dysfunction and mortality[J]. J Crit Care, 2018, 43: 30-35. doi: 10.1016/j.jcrc.2017.08.019
[15] Lee K, Jang JS, Kim J, et al. Age shock index, shock index, and modified shock index for predicting postintubation hypotension in the emergency department[J]. Am J Emerg Med, 2020, 38(5): 911-915. doi: 10.1016/j.ajem.2019.07.011
[16] Jiang L, Caputo ND, Chang BP. Respiratory adjusted shock index for identifying occult shock and level of Care in sepsis Patients[J]. Am J Emerg Med, 2019, 37(3): 506-509. doi: 10.1016/j.ajem.2019.01.026
[17] Hashemian AM, Baghshani Z, Farzaneh R, et al. Comparison of the relationship between SI and RASI scores with the outcome of sepsis patients[J]. Front Med(Lausanne), 2022, 9: 872725.
[18] Guarino M, Gambuti E, Alfano F, et al. Predicting in-hospital mortality for sepsis: a comparison between qSOFA and modified qSOFA in a 2-year single-centre retrospective analysis[J]. Eur J Clin Microbiol Infect Dis, 2021, 40(4): 825-831.
[19] Guarino M, Perna B, de Giorgi A, et al. A 2-year retrospective analysis of the prognostic value of MqSOFA compared to lactate, NEWS and qSOFA in patients with sepsis[J]. Infection, 2022, 50(4): 941-948.
[20] Hu H, Jiang JY, Yao N. Comparison of different versions of the quick sequential organ failure assessment for predicting in-hospital mortality of sepsis patients: A retrospective observational study[J]. World J Emerg Med, 2022, 13(2): 114-119.
[21] Shen YF, Zhu LH, Yan J. Stability of SpO2/FiO2 and respiratory rate-oxygenation indexes in critical respiratory disorders[J]. Crit Care Med, 2022, 50(8): e694-e695.
[22] Carvalho EB, Leite TRS, Sacramento RFM, et al. Rationale and limitations of the SpO2/FiO2 as a possible substitute for PaO2/FiO2 in different preclinical and clinical scenarios[J]. Rev Bras Ter Intensiva, 2022, 34(1): 185-196.
[23] Silverston P, Ferrari M, Quaresima V. Pulse oximetry in primary care: factors affecting accuracy and interpretation[J]. Br J Gen Pract, 2022, 72(716): 132-133.
-




 下载:
下载: