Clinical study on intravenous iron sucrose in elderly patients with iron deficiency and heart failure with reduced ejection fraction
-
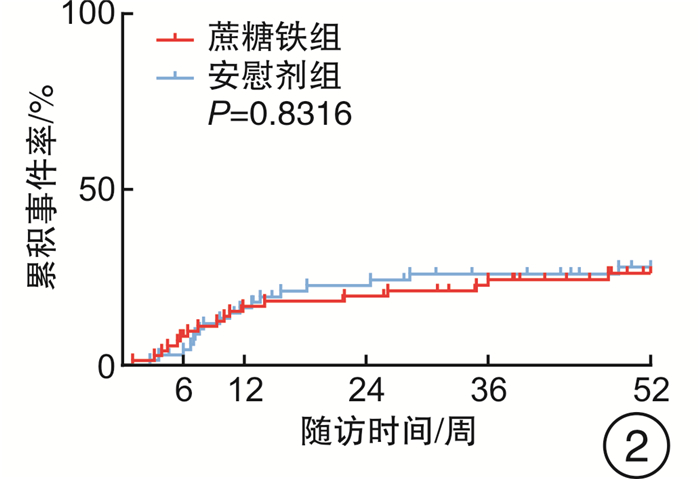
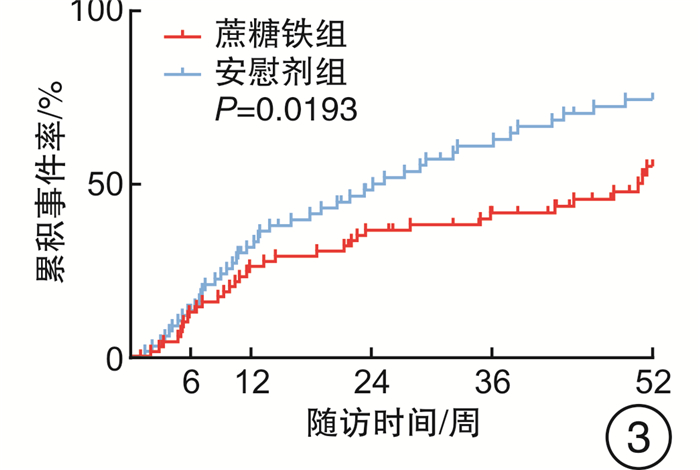
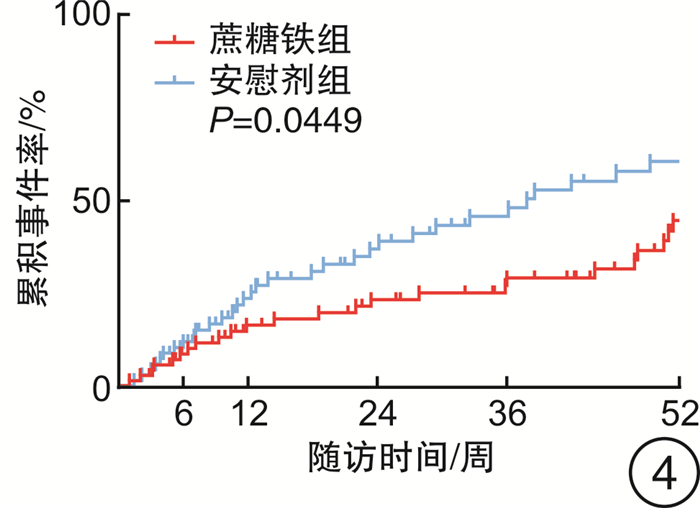
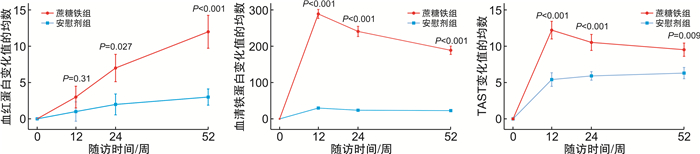
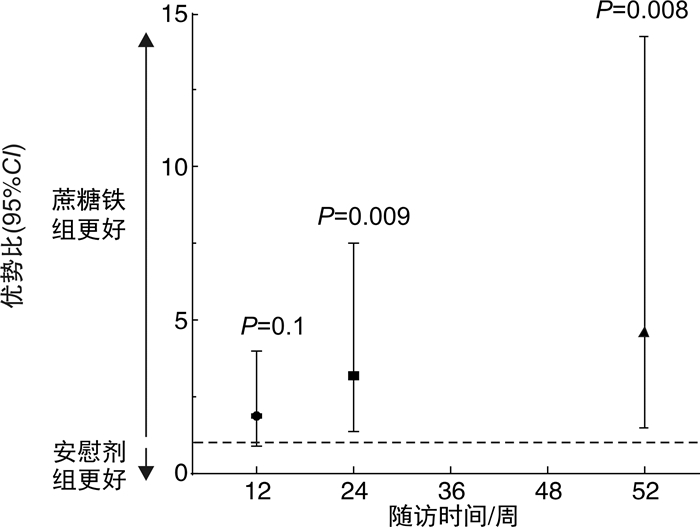
摘要: 目的 评估急性射血分数下降心力衰竭(HFrEF)合并铁缺乏(ID)的老年住院患者出院前静脉应用蔗糖铁的安全性和远期影响。方法 连续入选2017年8月—2019年5月青岛市市立医院急诊科因急性HFrEF住院且合并ID的老年患者140例,出院前随机给予蔗糖铁(n=72)或安慰剂(n=68),测量并评估2组患者出院前及出院后第6、12、24、36、52周的血红蛋白、铁蛋白、纽约心脏协会(NYHA)分级等指标和不良心血管事件(心衰再入院和心血管死亡),并在治疗开始后进行安全性分析。结果 蔗糖铁组和安慰剂组患者临床基线资料差异均无统计学意义(均P>0.05)。蔗糖铁组有40例(55.6%)患者发生心力衰竭(心衰)再入院和心血管死亡复合终点,安慰剂组58例(85.3%),有下降趋势,但差异无统计学意义(P=0.05);2组累积心血管死亡率亦差异无统计学意义[蔗糖铁组18例(25.0%),安慰剂组18例(26.5%),P=0.83]。蔗糖铁组有34例(47.2%)患者发生心衰再入院,安慰剂组有45例(66.2%),蔗糖铁组累积事件率明显低于安慰剂组(P=0.02)。蔗糖铁组患者累积首次心力衰竭住院或心血管死亡的复合终点率明显低于安慰剂组[蔗糖铁组24例(33.3%),安慰剂组32例(47.1%),P=0.04]。2组患者不良事件发生情况差异无统计学意义(P=0.653)。回归分析结果显示,早期静脉应用蔗糖铁的患者心功能从第24周起显著好转(24周P=0.009,52周P=0.008)。结论 早期静脉应用蔗糖铁可持续改善老年HFrEF合并ID患者的心功能,降低心衰再入院的风险,且安全性良好,但对心血管死亡风险无明显影响。
-
关键词:
- 射血分数下降心力衰竭,急性 /
- 蔗糖铁 /
- 铁缺乏
Abstract: Objective To evaluate the efficacy and safety of intravenous iron sucrose, compared with placebo, before hospital discharge among patients hospitalized for iron deficiency(ID) and acute heart failure with reduced ejection fraction(HFrEF).Methods A total of 140 hospitalized patients with acute HFrEF and ID in Department of Emergency of Qingdao Municipal Hospital from August 2017 to May 2019 were randomly assigned (1∶1) to receive intravenous iron sucrose(n=72) or placebo(n=68) before hospital discharge. Haemoglobin, serum ferritin, New York Heart Association(NYHA) class, major adverse cardiovascular events(heart failure hospitalizations and cardiovascular death) and so on were analyzed before discharge and at weeks 6, 12, 24, 36 and 52 after discharge. Safety was assessed in all patients for whom treatment was started.Results The clinical baseline characteristics were similar between iron sucrose group and placebo group(all P>0.05). There were 40(55.6%) cases with total heart failure hospitalizations and cardiovascular death occurred in the iron sucrose group and 58(85.3%) occurred in the placebo group(P=0.05). There was no difference in cardiovascular death rates between the two groups(18[25.0%]in the iron sucrose group vs.18[26.5%]in the placebo group, P=0.83). There were 34(47.2%) cases with total heart failure hospitalizations and cardiovascular death occurred in the iron sucrose group and 45(66.2%) occurred in the placebo group, and cumulative incidence rates in the iron sucrose group were significantly lower than those in the placebo group(P=0.02). Cumulative rates of first heart failure hospitalization or cardiovascular death were lower with iron sucrose than with placebo(24[33.3%]in the iron sucrose group vs.32[47.1%]in the placebo group, P=0.04). There was no dereference in advent events between the two groups(P=0.653). The use of iron sucrose, when compared with placebo, showed a significant benefit in NYHA class from week 24 onwards(P=0.009 at week 24 and P=0.008 at week 52).Conclusion Treatment of elderly, iron-deficient, HFrEF patients with iron sucrose resulted in sustainable improvement in cardiac function, and which was safe and reduced the risk of heart failure hospitalizations, with no apparent effect on the risk of cardiovascular death. -

-
表 1 2组急性HFrEF患者的临床基线资料表
X±S,M(P25,P75),例(%) 临床资料 蔗糖铁组(n=72) 安慰剂组(n=68) t/χ2/Z P 年龄/岁 78.82±8.09 76.88±7.78 1.442 0.151 男性 41(56.9) 35(51.5) 0.422 0.516 体质量指数 24.80±6.31 25.35±4.54 -0.602 0.548 收缩压/mmHga) 126.82±21.41 124.92±19.54 0.547 0.585 舒张压/mmHg 69.71±12.89 72.80±14.25 -1.346 0.181 心率/(次·min-1) 78.81±14.23 80.01±15.62 -0.477 0.634 NYHA心功能分级 Ⅱ级 5(7.0) 7(10.3) Ⅲ级 50(69.4) 50(73.5) -1.222 0.222 Ⅳ级 17(23.6) 11(16.2) 超声心动图指标 左心房前后径/mm 42.69±5.00 42.21±5.55 0.540 0.590 左心室舒张末期内径/mm 59.03±7.46 58.35±8.70 0.495 0.622 左心室射血分数/% 33.68±7.09 34.88±7.60 -0.968 0.335 缺血性心脏病 31(43.1) 28(41.2) 0.051 0.822 按心衰发生时间分类 新诊断心衰 20(27.8) 20(29.4) 0.046 0.831 因心衰首次住院>12个月 35(48.6) 32(47.1) 0.034 0.854 因心衰首次住院 < 12个月 17(23.6) 16(23.5) < 0.010 0.991 合并症 既往心肌梗死 28(38.9) 24(35.3) 0.194 0.660 既往脑卒中 6(8.3) 3(4.4) 0.894 0.344 糖尿病 33(45.8) 26(38.2) 0.828 0.363 高血压 29(40.3) 23(33.8) 0.624 0.430 心房颤动/扑动 15(20.8) 19(27.9) 0.961 0.327 瓣膜病 11(15.3) 7(10.3) 0.775 0.379 慢性肾功能不全 15(20.8) 20(29.4) 1.373 0.241 吸烟史 14(19.4) 12(17.6) 0.075 0.785 临床用药 ACEI/ARB 47(65.3) 49(72.1) 0.746 0.388 ARNI 11(15.3) 13(19.1) 0.363 0.547 β受体阻滞剂 51(70.8) 56(82.4) 2.576 0.108 螺内酯 56(77.8) 58(85.3) 1.306 0.253 髓袢利尿剂 49(68.1) 54(79.4) 2.320 0.128 洋地黄类药物 18(25.0) 21(30.9) 0.602 0.438 非药物治疗 冠状动脉血运重建术 18(25.0) 15(22.1) 0.168 0.682 心脏再同步化治疗/植入式心脏复律除颤器 1(1.4) 2(2.9) 0.399 0.528 实验室检查 NT-proBNP/(pg·mL-1) 5062.72(2119.25,7307.25) 4997.21(1691.05,7126.75) -0.913 0.361 血红蛋白/(g·L-1) 122.04±15.05 124.16±12.68 -0.899 0.370 贫血 23(31.9) 20(29.4) 0.105 0.745 铁蛋白/(μg·L-1) 88.94±51.01 91.79±54.25 -0.321 0.749 转铁蛋白饱和度/% 18.72±11.67 19.73±11.53 -0.514 0.608 肌酐清除率/(mL·min-1) 67.71±17.05 70.05±22.45 -0.691 0.491 注:a)1 mmHg=0.133 kPa。 表 2 2组患者不良事件发生情况的对比
例(%) 不良事件发生情况 蔗糖铁组
(n=72)安慰剂组
(n=68)χ2 P 至少发生一次药物相关的不良事件 3(4.2) 1(1.5) 0.202 0.653 皮肤潮红或瘙痒 2(2.8) 0 恶心 1(1.4) 0 胸闷和(或)心悸 1(1.4) 1(1.5) 因不良事件再入院或死亡 0 0 -
[1] Klip IT, Comin-Colet J, Voors AA, et al. Iron deficiency in chronic heart failure: an international pooled analysis[J]. Am Heart J, 2013, 165(4): 575-582. e3. doi: 10.1016/j.ahj.2013.01.017
[2] Beale A, Carballo D, Stirnemann J, et al. Iron deficiency in acute decompensated heart failure[J]. J Clin Med, 2019, 8(10): 1569. doi: 10.3390/jcm8101569
[3] Savarese G, von Haehling S, Butler J, et al. Iron deficiency and cardiovascular disease[J]. Eur Heart J, 2023, 44(1): 14-27. doi: 10.1093/eurheartj/ehac569
[4] Kalra PR, Cleland JGF, Petrie MC, et al. Intravenous ferric derisomaltose in patients with heart failure and iron deficiency in the UK(IRONMAN): an investigator-initiated, prospective, randomised, open-label, blinded-endpoint trial[J]. Lancet, 2022, 400(10369): 2199-2209. doi: 10.1016/S0140-6736(22)02083-9
[5] Ponikowski P, van Veldhuisen DJ, Comin-Colet J, et al. Rationale and design of the CONFIRM-HF study: a double-blind, randomized, placebo-controlled study to assess the effects of intravenous ferric carboxymaltose on functional capacity in patients with chronic heart failure and iron deficiency[J]. ESC Heart Fail, 2014, 1(1): 52-58. doi: 10.1002/ehf2.12006
[6] Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015[J]. Eur J Heart Fail, 2019, 21(11): 1329-1337. doi: 10.1002/ejhf.1629
[7] 中国医疗保健国际交流促进会急诊医学分会, 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 等. 急性心力衰竭中国急诊管理指南(2022)[J]. 临床急诊杂志, 2022, 23(8): 519-547. doi: 10.13201/j.issn.1009-5918.2022.08.001 https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.08.001
[8] Ponikowski P, van Veldhuisen DJ, Comin-Colet J, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency[J]. Eur Heart J, 2015, 36(11): 657-668. doi: 10.1093/eurheartj/ehu385
[9] Alnuwaysir RIS, Hoes MF, van Veldhuisen DJ, et al. Iron deficiency in heart failure: mechanisms and pathophysiology[J]. J Clin Med, 2021, 11(1): 125. doi: 10.3390/jcm11010125
[10] Beattie JM, Khatib R, Phillips CJ, et al. Iron deficiency in 78 805 people admitted with heart failure across England: a retrospective cohort study[J]. Open Heart, 2020, 7(1): e001153. doi: 10.1136/openhrt-2019-001153
[11] Simon S, Ioannou A, Deoraj S, et al. Audit of the prevalence and investigation of iron deficiency anaemia in patients with heart failure in hospital practice[J]. Postgrad Med J, 2020, 96(1134): 206-211. doi: 10.1136/postgradmedj-2019-136867
[12] Ambrosy AP, Lewis GD, Malhotra R, et al. Identifying responders to oral iron supplementation in heart failure with a reduced ejection fraction: a post-hoc analysis of the IRONOUT-HF trial[J]. J Cardiovasc Med(Hagerstown), 2019, 20(4): 223-225. doi: 10.2459/JCM.0000000000000736
[13] Lewis GD, Malhotra R, Hernandez AF, et al. Effect of oral iron repletion on exercise capacity in patients with heart failure with reduced ejection fraction and iron deficiency: the IRONOUT HF randomized clinical trial[J]. JAMA, 2017, 317(19): 1958-1966. doi: 10.1001/jama.2017.5427
[14] van Veldhuisen DJ, Ponikowski P, van der Meer P, et al. Effect of ferric carboxymaltose on exercise capacity in patients with chronic heart failure and iron deficiency[J]. Circulation, 2017, 136(15): 1374-1383. doi: 10.1161/CIRCULATIONAHA.117.027497
[15] Macdougall IC, Comin-Colet J, Breymann C, et al. Iron Sucrose: A wealth of experience in treating iron deficiency[J]. Adv Ther, 2020, 37(5): 1960-2002. doi: 10.1007/s12325-020-01323-z
[16] Loncar G, Obradovic D, Thiele H, et al. Iron deficiency in heart failure[J]. ESC Heart Fail, 2021, 8(4): 2368-2379. doi: 10.1002/ehf2.13265
[17] Xu HT, Duan YB, Yuan X, et al. Intravenous iron versus placebo in the management of postoperative functional iron deficiency anemia in patients undergoing cardiac valvular surgery: a prospective, single-blinded, randomized controlled trial[J]. J Cardiothorac Vasc Anesth, 2019, 33(11): 2941-2948. doi: 10.1053/j.jvca.2019.01.063
[18] MacDougall IC, White C, Anker SD, et al. Intravenous iron in patients undergoing maintenance hemodialysis[J]. N Engl J Med, 2019, 380(5): 447-458. doi: 10.1056/NEJMoa1810742
[19] MacDougall IC, Comin-Colet J, Breymann C, et al. Iron sucrose: a wealth of experience in treating iron deficiency[J]. Adv Ther, 2020, 37(5): 1960-2002. doi: 10.1007/s12325-020-01323-z
[20] Ponikowski P, Kirwan BA, Anker SD, et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial[J]. Lancet, 2020, 396(10266): 1895-1904. doi: 10.1016/S0140-6736(20)32339-4
[21] McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-3726. doi: 10.1093/eurheartj/ehab368
[22] Becher PM, Schrage B, Benson L, et al. Phenotyping heart failure patients for iron deficiency and use of intravenous iron therapy: data from the Swedish Heart Failure Registry[J]. Eur J Heart Fail, 2021, 23(11): 1844-1854. doi: 10.1002/ejhf.2338
[23] 中华医学会血液学分会红细胞疾病(贫血)学组. 静脉铁剂应用中国专家共识(2019年版)[J]. 中华血液学杂志, 2019, 40(5): 358-362.
[24] Okonko DO, Grzeslo A, Witkowski T, et al. Effect of intravenous iron sucrose on exercise tolerance in anemic and nonanemic patients with symptomatic chronic heart failure and iron deficiency FERRIC-HF: a randomized, controlled, observer-blinded trial[J]. J Am Coll Cardiol, 2008, 51(2): 103-112. doi: 10.1016/j.jacc.2007.09.036
-





 下载:
下载: