Prognostic value of early monitoring of PCT, CAR, D-dimer combined with ISS and APACHE Ⅱ score in EICU trauma patients
-
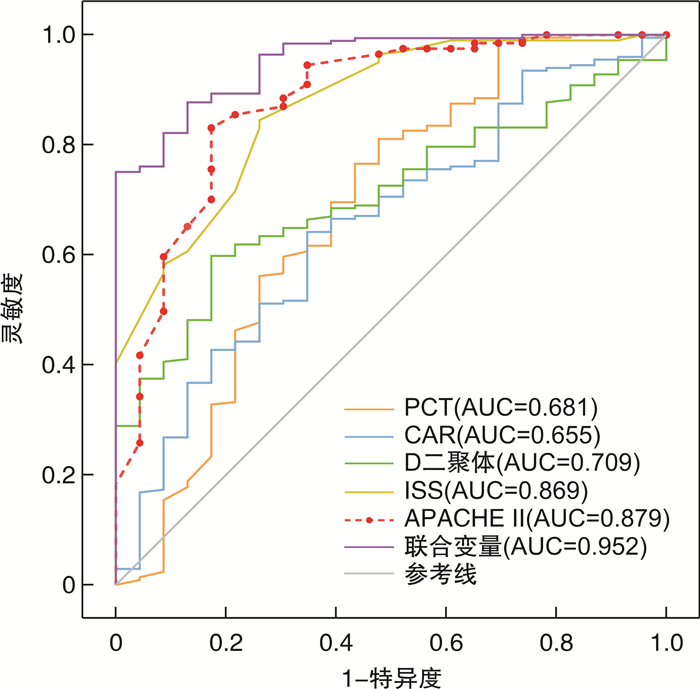
摘要: 目的 评估降钙素原(PCT)、C-反应蛋白/白蛋白比值(CAR)、D-二聚体及损伤严重度评分(ISS评分)联合急性生理与慢性健康评分(APACHE Ⅱ)在预测EICU创伤患者的预后和病死率方面的价值。方法 选取2020年1月—2022年3月联勤保障部队第九二〇医院EICU共收治的224例符合纳入标准的创伤患者,对其临床资料进行观察性研究。根据28 d生存状态进行分组,比较2组患者入住EICU首日的基本资料、PCT、CAR、D-二聚体和ISS、APACHE Ⅱ评分;采用多因素logistic回归分析筛选出影响创伤患者死亡的危险因素;并绘制上述参数的受试者工作特征曲线(ROC曲线),分析其对创伤患者的预测价值。结果 纳入研究的224例EICU创伤患者28 d病死率为10.3%。最常见的致伤因素为车祸伤。死亡组的PCT、CAR、D-二聚体值和ISS、APACHE Ⅱ评分均显著高于存活组(P < 0.05)。logistic回归分析结果显示,头颈部受伤、CRP、PCT、D-二聚体、ISS评分和APACHE Ⅱ评分是影响EICU创伤患者28 d死亡的独立危险因素。ROC曲线分析显示,PCT、CAR、D-二聚体、ISS、APACHE Ⅱ评分均对创伤患者预后具有一定的预测价值,ROC曲线下面积(AUC)分别为0.681、0.655、0.709、0.869、0.879(均P < 0.05),且五者联合预测的AUC高达0.952,灵敏度为100%,特异度为75.1%,提示联合变量预测创伤患者死亡的准确性更高。APACHE Ⅱ评分与PCT、CAR、D-二聚体及ISS评分呈正相关(P < 0.05)。结论 EICU创伤死亡者早期具有PCT、CAR、D-二聚体高值及ISS、APACHE Ⅱ高评分,以上独立危险因素有助于评估创伤患者病情的严重程度;且5项指标联合变量对创伤患者预后的预测能力最佳。
-
关键词:
- 创伤 /
- 损伤严重程度评分 /
- 急性生理与慢性健康评分Ⅱ /
- 降钙素原 /
- C-反应蛋白/白蛋白比值 /
- D-二聚体
Abstract: Objective To evaluate the prognostic value of procalcitonin (PCT), C-reactive protein/albumin ratio (CAR), D-dimer and injury severity score (ISS score) combined with acute physiology and chronic health evaluation scoring system (APACHE Ⅱ) in predicting the prognosis and mortality of trauma patients in EICU.Methods The clinical data of 224 trauma patients admitted to EICU of 920th Hospital of Joint Logistics Support Force from January 2020 to March 2022, conforming to the inclusion criteria, were observed for analysis. The patients were divided into two groups according to 28-day survival status, the basic data, PCT, CAR, D-dimer, ISS and APACHE Ⅱ score of the two groups on the first day of EICU admission were compared. The risk factors of trauma patients were screened by multivariate logistic regression analysis, and receiver operating characteristic curve (ROC curve) of the above parameters was drawn to analyze its predictive value for trauma patients.Results The 28-day mortality in EICU of 224 patients included in this study was 10.2%. The most common cause of injury was motor vehicle injury. The PCT, CAR, D-dimer, ISS and APACHE Ⅱ scores in the death group were significantly higher than those in the survival group(P < 0.05). Logistic regression analysis showed that head and neck injury, CRP, PCT, D-dimer, ISS score and APACHE Ⅱ score were independent risk factors for 28 d death in EICU trauma patients. The analysis of ROC curve showed that PCT, CAR, D-dimer, ISS, APACHE Ⅱ score had certain predictive values for the prognosis of trauma patients, and the area under the ROC curve (AUC) was 0.681, 0.655, 0.709, 0.869, 0.879, respectively (all P < 0.05). The AUC of the combined prediction of the five variables was up to 0.952, the sensitivity was 100%, and the specificity was 75.1%, which indicates that the combined variables has a higher accuracy in predicting the death of trauma patients. APACHE Ⅱ scores were positively correlated with PCT, CAR, D-dimer and ISS score(P < 0.05).Conclusion EICU trauma deaths had high PCT, CAR, D-dimer value and high ISS, APACHE Ⅱ score in the early stage. The above independent risk factors are beneficial to evaluating disease severity of trauma patients, and the combined variables of the five indexes has better predictive ability for the prognosis of trauma patients. -

-
表 1 存活组与死亡组EICU创伤患者基本资料比较
例(%),M(P25,P75) 项目 存活组(n=201) 死亡组(n=23) t/χ2/Z P 性别 4.158 0.041 男 146(72.6) 12(52.2) 女 55(27.4) 11(47.8) 年龄/岁 45.28±16.88 49.96±19.20 -1.241 0.216 伤后入院时间/h 8(5,12) 7(5,12) -0.888 0.375 受伤部位 头颈 91(45.3) 22(95.7) 20.494 < 0.001 面部 44(21.9) 11(47.8) 7.494 0.006 胸部或胸椎 133(66.2) 22(95.7) 8.417 0.004 腹部或腰椎 77(38.3) 13(56.5) 2.841 0.091 四肢或骨盆 172(85.6) 18(78.3) 0.383 0.536 致伤原因 6.823 0.448 车祸伤 71(35.3) 13(56.5) 高坠伤 44(21.9) 4(17.4) 重物砸伤 26(12.9) 2(8.7) 摔伤 24(11.9) 1(4.3) 机器绞伤 21(10.4) 1(4.3) 锐器伤 7(3.5) 0 爆炸伤 3(1.5) 1(4.3) 其他 5(2.5) 1(4.3) T/℃ 36.8(36.5,3.2) 36.8(36.4,38.5) -1.105 0.269 HR/(次·min-1) 96.15±23.86 111.39±27.53 -2.856 0.005 RR/(次·min-1) 19(18,21) 20(15,22) -0.026 0.979 SBP/mmHga) 105(91,117) 93(79,110) -2.699 0.007 DBP/mmHg 60(55,70) 53(43,69) -2.515 0.012 注:a)1 mmHg=0.133 kPa;SBP,收缩压;DBP,舒张压。 表 2 EICU入院首日2组间预后参数的比较
X±S,M(P25,P75) 预后参数 存活组(n=201) 死亡组(n=23) t/χ2/Z P 白蛋白/(g·L-1) 29.60±7.01 25.94±9.86 2.259 0.025 CRP/(mg·L-1) 41.3(16.1,72.4) 60(42.5,10.5) -1.987 0.047 PCT/(μg·L-1) 0.54(0.25,2.49) 5.01(0.50,40.01) -2.843 0.004 CAR 1.42(0.54,0.60) 2.37(1.27,4.67) -2.429 0.015 D-二聚体/(mg·L-1) 3.94(1.22,9.94) 9.57(6.67,1.14) -3.275 < 0.001 Lac/(mmol·L-1) 2.3(1.4,4.6) 4.5(1.5,9.7) -2.613 0.009 ISS/分 22(17,29) 38(29,45) -5.832 < 0.001 APACHE Ⅱ/分 8(4,11) 19(14,32) -5.932 < 0.001 表 3 EICU创伤患者预后多因素logistic回归
危险因素 β 标准误 Waldχ2 P OR 95%CI 下限 上限 性别 -2.119 1.110 3.645 0.056 0.120 0.014 1.058 头颈 4.528 2.172 4.344 0.037 92.557 1.310 6539.402 面部 -0.902 1.003 0.808 0.369 0.406 0.057 2.900 胸部或胸椎 -2.162 1.604 1.817 0.178 0.115 0.005 2.667 HR 0.009 0.020 0.213 0.644 1.009 0.970 1.050 SBP 0.035 0.036 0.905 0.341 1.035 0.964 1.112 DBP 0.006 0.058 0.011 0.918 1.006 0.898 1.127 Lac 0.136 0.167 0.664 0.415 1.146 0.826 1.591 白蛋白 0.091 0.092 0.967 0.326 1.095 0.914 1.312 CRP -0.066 0.032 4.382 0.036 0.936 0.880 0.996 CAR 0.902 0.603 2.238 0.135 2.464 0.756 8.029 PCT 0.073 0.032 5.147 0.023 1.076 1.010 1.146 D-二聚体 -0.097 0.038 6.353 0.012 0.908 0.842 0.979 ISS 0.250 0.083 9.126 0.003 1.284 1.092 1.510 APACHE Ⅱ 0.245 0.093 6.986 0.008 1.278 1.065 1.533 表 4 预测病死率的预后参数ROC分析
预测指标 AUC P 最佳截断值 95%CI 灵敏度/% 特异度/% 约登指数 PCT 0.681 0.005 5.005 0.546~0.817 52.2 81.1 0.333 CAR 0.655 0.015 1.913 0.539~0.770 65.2 64.2 0.294 D-二聚体 0.709 0.001 6.225 0.621~0.796 82.6 59.9 0.425 ISS 0.869 < 0.001 33.500 0.796~0.942 73.9 84.6 0.585 APACHE Ⅱ 0.879 < 0.001 17.500 0.798~0.961 65.2 94.5 0.597 联合变量 0.952 < 0.001 0.917~0.987 100.0 75.1 0.751 表 5 基于预后参数最佳截断值分组的影响
例(%) 预测指标 存活组
(n=201)死亡组
(n=23)χ2 P PCT/(μg·L-1) 13.174 < 0.001 >5.005 38(18.9) 12(52.2) ≤5.005 163(81.1) 11(47.8) CAR 7.508 0.006 >1.913 72(35.8) 15(65.2) ≤1.913 129(64.2) 8(38.8) D-二聚体/(mg·L-1) 15.065 < 0.001 >6.225 79(40.1) 19(82.6) ≤6.225 118(59.9) 4(17.4) ISS评分/分 38.534 < 0.001 >33.5 31(15.4) 17(73.9) ≤33.5 170(84.6) 6(26.1) APACHE Ⅱ评分/分 66.096 < 0.001 >17.5 11(5.5) 15(65.2) ≤17.5 190(94.5) 8(34.8) 表 6 APACHE Ⅱ评分与其余指标的相关性
指标 APACHE Ⅱ评分 r P PCT 0.454 0.001 CAR 0.382 0.001 D-二聚体 0.323 0.001 ISS评分 0.369 0.001 -
[1] James SL, Castle CD, Dingels ZV, et al. Global injury morbidity and mortality from 1990 to 2017: results from the Global Burden of Disease Study 2017[J]. Inj Prev, 2020, 26(Supp 1): i96-i114. doi: 10.1136/injuryprev-2019-043494
[2] Shiraishi A, Otomo Y, Yoshikawa S, et al. Derivation and validation of an easy-to-compute trauma score that improves prognostication of mortality or the Trauma Rating Index in Age, Glasgow Coma Scale, Respiratory rate and Systolic blood pressure(TRIAGES)score[J]. Crit Care, 2019, 23(1): 365. doi: 10.1186/s13054-019-2636-x
[3] 金颖, 王嘉. RDW/ALB和CRP/ALB比值预测重症社区感染性肺炎患者院内死亡的临床价值[J]. 临床急诊杂志, 2022, 23(6): 405-411. doi: 10.13201/j.issn.1009-5918.2022.06.007 https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.06.007
[4] Özcan S, Dönmez E, Yavuz Tuǧrul S, et al. The prognostic value of C-reactive protein/albumin ratio in acute pulmonary embolism[J]. Rev Invest Clin, 2022, 74(2): 97-103.
[5] Özçiftci Yılmaz P, Karacan E. The effects of C-reactive protein/albumin ratio and hematologic parameters on predicting the prognosis for emergency surgical patients in intensive care[J]. Ulus Travma Acil Cerrahi Derg, 2021, 27(1): 67-72.
[6] Deniz M, Ozgun P, Ozdemir E. Relationships between RDW, NLR, CAR, and APACHE Ⅱ scores in the context of predicting the prognosis and mortality in ICU patients[J]. Eur Rev Med Pharmacol Sci, 2022, 26(12): 4258-4267.
[7] Duan LL, Ye PP, Haagsma JA, et al. The burden of injury in China, 1990-2017: findings from the Global Burden of Disease Study 2017[J]. Lancet Public Health, 2019, 4(9): e449-e461. doi: 10.1016/S2468-2667(19)30125-2
[8] Tian W, Meng W. Associations of homocysteine, procalcitonin, and D-dimer levels with severity and prognosis of patients with multiple trauma[J]. Clin Lab, 2022, 68(3).
[9] Wojtaszek M, Staśkiewicz G, Torres K, et al. Changes of procalcitonin level in multiple trauma patients[J]. Anaesthesiol Intensive Ther, 2014, 46(2): 78-82. doi: 10.5603/AIT.2014.0015
[10] AlRawahi AN, AlHinai FA, Doig CJ, et al. The prognostic value of serum procalcitonin measurements in critically injured patients: a systematic review[J]. Crit Care, 2019, 23(1): 390. doi: 10.1186/s13054-019-2669-1
[11] Foaud HMA, Labib JR, Metwally HG, et al. Plasma D-dimer as a prognostic marker in ICU admitted Egyptian children with traumatic brain injury[J]. J Clin Diagn Res, 2014, 8(9): PC01-PC06.
[12] Umebachi R, Taira T, Wakai S, et al. Measurement of blood lactate, D-dimer, and activated prothrombin time improves prediction of in-hospital mortality in adults blunt trauma[J]. Am J Emerg Med, 2018, 36(3): 370-375. doi: 10.1016/j.ajem.2017.08.025
[13] Ishii K, Kinoshita T, Kiridume K, et al. Impact of initial coagulation and fibrinolytic markers on mortality in patients with severe blunt trauma: a multicentre retrospective observational study[J]. Scand J Trauma Resusc Emerg Med, 2019, 27(1): 25. doi: 10.1186/s13049-019-0606-6
[14] Zacho J, Benfield T, Tybjærg-Hansen A, et al. Increased baseline C-reactive protein concentrations are associated with increased risk of infections: results from 2 large Danish population cohorts[J]. Clin Chem, 2016, 62(2): 335-342. doi: 10.1373/clinchem.2015.249680
[15] Xu LB, Yue JK, Korley F, et al. High-sensitivity C-reactive protein is a prognostic biomarker of six-month disability after traumatic brain injury: results from the TRACK-TBI study[J]. J Neurotrauma, 2021, 38(7): 918-927. doi: 10.1089/neu.2020.7177
[16] Balta O, Altınayak H, Gürler Balta M, et al. Can C-reactive protein-based biomarkers be used as predictive of 30-day mortality in elderly hip fractures?A retrospective study[J]. Ulus Travma Acil Cerrahi Derg, 2022, 28(6): 849-856.
[17] Eckart A, Struja T, Kutz A, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study[J]. Am J Med, 2020, 133(6): 713-722. e7. doi: 10.1016/j.amjmed.2019.10.031
[18] Park JE, Chung KS, Song JH, et al. The C-reactive protein/albumin ratio as a predictor of mortality in critically ill patients[J]. J Clin Med, 2018, 7(10): 333. doi: 10.3390/jcm7100333
[19] 邓淑萍, 邱红, 王斌, 等. 重症创伤患者早期死亡危险因素分析[J]. 创伤外科杂志, 2021, 23(10): 771-774, 780. https://www.cnki.com.cn/Article/CJFDTOTAL-CXWK202110018.htm
[20] Atik B, Kilinc G, Yarar V. Predictive value of prognostic factors at multiple trauma patients in intensive care admission[J]. Bratisl Lek Listy, 2021, 122(4): 277-279.
[21] 余倩, 江利冰, 高建波. APACHE Ⅱ评分和TRISS评分预测ICU创伤患者预后的Meta分析[J]. 中华危重病急救医学, 2022, 34(1): 59-63. https://www.cnki.com.cn/Article/CJFDTOTAL-KGHL201501014.htm
-




 下载:
下载: