Effect of serum phosphorus level on illness and prognosis of elderly patients with community acquired pneumonia
-
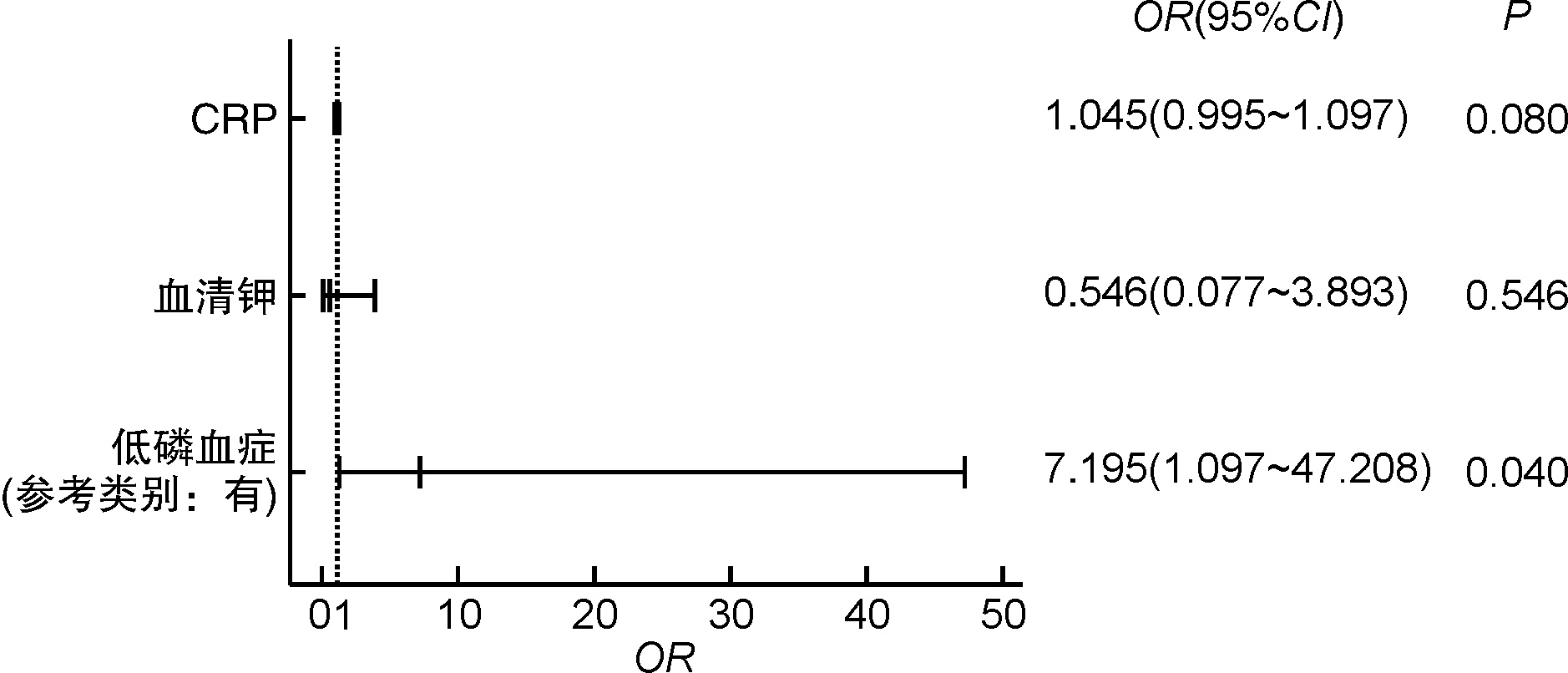
摘要: 目的 探讨老年社区获得性肺炎患者早期血清磷水平的变化及对患者病情及预后的影响。方法 回顾性选取2020年2月1日—2021年10月31日于东部战区总医院确诊的62例社区获得性肺炎的老年患者,根据患者住院期间疾病严重程度分为普通型组和重症组,统计2组患者的入院时人口统计学资料、临床资料和低磷血症发生情况,通过logistic回归分析重症发生的危险因素,Spearman检验进行重症发生的相关性分析,并比较低磷血症组和非低磷血症组的病情严重程度、ICU住院率、机械通气使用率以及住院期间生存情况。结果 重症组患者CRP水平高于对照组(P < 0.05),氧合指数、血清钾、血清磷水平低于普通型组患者(P < 0.05),通过单因素logistic回归分析初筛示CRP、血清钾、血清磷以及氧合指数是重症发生的风险因素;进一步通过多因素logistic回归分析示低磷血症是发生重症的风险因素(OR=7.195,95%CI:1.097~47.208)。低磷血症组的重症发生率、机械通气使用率、ICU住院率以及病死率均高于非低磷血症组(P < 0.05)。结论 在老年社区获得性肺炎患者中常见血清磷水平的下降,而低磷血症的发生与老年社区获得性肺炎患者的病情严重程度和不良预后具有一定相关性。Abstract: Objective To investigate the changes of serum phosphorus level in elderly patients with community acquired pneumonia in the early stage and its influence on the patients' condition and prognosis.Methods 62 elderly patients diagnosed with community acquired pneumonia from February 1, 2020 to October 31, 2021 were retrospectively analyzed. According to the severity of disease during hospitalization, the patients were divided into the general group and the severe group. The demographic data, clinical data and incidence of hypophosphatemia at admission of the two groups were statistically analyzed. Logistic regression analysis was used to analyze the risk factors for severe status. Spearman's analysis was conducted for the correlation analysis with severe status. We also compared the severity of illness, ICU hospitalization rate, mechanical ventilation utilization rate, and motality during hospitalization between the hypophosphatemia group and the non-hypophosphatemia group.Results CRP level in severe group was higher than that in the control group (P < 0.05), and the levels of oxygenation index, serum potassium and serum phosphorus were lower than those in the general group (P < 0.05). Univariate logistic regression analysis showed that CRP, serum potassium, serum phosphorus and oxygenation index were the risk factors for severe disease. Further multivariate logistic regression analysis showed that the occurrence of hypophosphatemia was a risk factor for severe disease (OR: 7.195, 95%CI: 1.097-47.208). The incidence of severe status, mechanical ventilation utilization rate, ICU hospitalization rate and mortality in the hypophosphatemia group were higher than those in the non-hypophosphatemia group (P < 0.05).Conclusion Hypophosphatemia is common in elderly patients with community acquired pneumonia. It is associated with the severity and poor prognosis of elderly patients with community acquired pneumonia.
-
Key words:
- hypophosphatemia /
- elderly /
- community acquired pneumonia /
- prognosis
-

-
表 1 2组患者基线资料比较
例(%),X±S 基线资料 严重程度 普通型组(n=44) 重症组(n=18) t/χ2 P 年龄/岁 67.73±6.892 71.67±8.731 2.105 0.064 男性 16(36.4) 10(55.6) 1.932 0.165 体重指数/(kg/m2) 22.34±4.47 22.49±2.69 -0.130 0.897 既往基础疾病 高血压 18(40.9) 8(44.4) 0.066 0.798 糖尿病 11(25.0) 2(11.1) 0.767 0.381 冠心病 7(15.9) 4(22.2) 0.050 0.822 慢性阻塞性肺病 4(9.1) 3(16.7) 0.171 0.679 检验指标 淋巴细胞计数/(×109·L-1) 1.36±0.53 1.10±0.54 1.733 0.088 谷丙转氨酶/(U·L-1) 31.16±29.42 41.44±36.86 -1.159 0.251 肌酐/(μmol·L-1) 58.41±14.41 62.56±31.57 -0.535 0.599 脑利钠肽/(pg·mL-1) 265.88±450.49 465.83±729.57 -1.00 0.325 CRP/(mg·L-1) 7.28±10.89 47.89±47.34 -3.456 0.030 白介素6/(pg·mL-1) 18.66±23.85 27.33±24.80 -1.084 0.286 氧合指数/mmHg 409.15±79.69 195.25±96.98 9.00 <0.001 血清钾/(mmol·L-1) 4.36±0.41 4.07±0.56 2.348 0.022 血清钠/(mmol·L-1) 140.68±2.15 142.68±6.95 -1.198 0.246 血清氯/(mmol·L-1) 102.13±3.95 101.61±6.59 0.312 0.758 血清钙/(mmol·L-1) 2.21±0.11 2.15±0.15 1.843 0.070 血清磷/(mmol·L-1) 1.09±0.18 0.94±0.24 2.665 0.010 低磷血症 8(18.18) 13(72.22) 16.655 < 0.010 注:1 mmHg=0.133 kPa。 表 2 单因素logistic回归分析
自变量 P OR 95%CI 年龄 0.106 1.059 0.988~1.134 CRP 0.012 1.069 1.015~1.126 血清钾 0.031 0.229 0.060~0.871 血清磷 < 0.010 11.700 3.238~42.283 氧合指数 < 0.010 0.977 0.967~0.987 注:OR,优势比;95%CI,95%置信区间。 表 3 2组患者临床资料比较
例(%) 指标 非低磷血症组(n=41) 低磷血症组(n=21) χ2 P 重症例数情况 5(12.2) 13(61.9) 16.655 < 0.010 机械通气使用 5(12.2) 12(57.1) 14.098 < 0.010 ICU住院 6(14.6) 13(61.9) 14.600 < 0.010 住院期间死亡预后 1(2.4) 5(23.8) 5.017 0.025 -
[1] 李鹏, 张兴厅, 尹芳, 等. 医疗大数据对老年肺炎患者预后的预测价值: 基于北京市朝阳医院医联体朝阳急诊病房数据结果[J]. 中华危重病急救医学, 2021, 33(3): 338-343. doi: 10.3760/cma.j.cn121430-20200611-00461
[2] Cillóniz C, Dominedò C, Pericàs JM, et al. Community-acquired pneumonia in critically ill very old patients: a growing problem[J]. Eur Respir Rev, 2020, 29(155): 190126. doi: 10.1183/16000617.0126-2019
[3] Chang AR, Anderson C. Dietary Phosphorus intake and the kidney[J]. Annu Rev Nutr, 2017, 37: 321-346. doi: 10.1146/annurev-nutr-071816-064607
[4] Shah S, Lodha R. Respiratory muscle weakness, a major contributor to pediatric extubation failure: does low serum Phosphorus contribute to muscle weakness?[J]. Crit Care Med, 2017, 45(12): e1303-e1304. doi: 10.1097/CCM.0000000000002709
[5] Fiaccadori E, Coffrini E, Fracchia C, et al. Hypophosphatemia and Phosphorus depletion in respiratory and peripheral muscles of patients with respiratory failure due to COPD[J]. Chest, 1994, 105(5): 1392-1398. doi: 10.1378/chest.105.5.1392
[6] 中国医师协会急诊医师分会, 中国急性感染联盟. 2015年中国急诊社区获得性肺炎临床实践指南[J]. 中华急诊医学杂志, 2015, 24(12): 1324-1344. doi: 10.3760/cma.j.issn.1671-0282.2015.12.004
[7] Chen YY, Klein SL, Garibaldi BT, et al. Aging in COVID-19: vulnerability, immunity and intervention[J]. Ageing Res Rev, 2021, 65: 101205. doi: 10.1016/j.arr.2020.101205
[8] Al Harbi SA, Al-Dorzi HM, Al Meshari AM, et al. Association between phosphate disturbances and mortality among critically ill patients with sepsis or septic shock[J]. BMC Pharmacol Toxicol, 2021, 22: 30. doi: 10.1186/s40360-021-00487-w
[9] Naffaa ME, Mustafa M, Azzam M, et al. Serum inorganic phosphorus levels predict 30-day mortality in patients with community acquired pneumonia[J]. BMC Infect Dis, 2015, 15: 332. doi: 10.1186/s12879-015-1094-6
[10] Chen ZJ, Gao CN, Yu HJ, et al. Hypophosphatemia is an independent risk factor for AKI among hospitalized patients with COVID-19 infection[J]. Ren Fail, 2021, 43(1): 1329-1337. doi: 10.1080/0886022X.2021.1979039
[11] Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy[J]. JAMA Intern Med, 2020, 180(10): 1345-1355. doi: 10.1001/jamainternmed.2020.3539
[12] Craddock PR, Yawata Y, VanSanten L, et al. Acquired phagocyte dysfunction. A complication of the hypophosphatemia of parenteral hyperalimentation[J]. N Engl J Med, 1974, 290(25): 1403-1407. doi: 10.1056/NEJM197406202902504
[13] Kim BK, Kim CY, Kim S, et al. Associations between Phosphate Concentrations and Hospital Mortality in Critically Ill Patients Receiving Mechanical Ventilation[J]. J Clin Med, 2022, 11(7): 1897. doi: 10.3390/jcm11071897
[14] Orr CL, Hutcheson DP, Grainger RB, et al. Serum copper, zinc, calcium and phosphorus concentrations of calves stressed by bovine respiratory disease and infectious bovine rhinotracheitis[J]. J Anim Sci, 1990, 68(9): 2893-2900. doi: 10.2527/1990.6892893x
[15] 李萍, 林桦, 张爱丽, 等. 血清磷水平与老年慢性阻塞性肺疾病合并Ⅱ型呼吸衰竭患者机械通气撤机结局的相关性分析[J]. 中华老年医学杂志, 2020, 39(6): 613-617. doi: 10.3760/cma.j.issn.0254-9026.2020.06.002
[16] Galanopoulos M, Gkeros F, Doukatas A, et al. COVID-19 pandemic: Pathophysiology and manifestations from the gastrointestinal tract[J]. World J Gastroenterol, 2020, 26(31): 4579-4588. doi: 10.3748/wjg.v26.i31.4579
[17] Janssens JP, Krause KH. Pneumonia in the very old[J]. Lancet Infect Dis, 2004, 4(2): 112-124. doi: 10.1016/S1473-3099(04)00931-4
[18] Simoni C, Camozzi P, Faré PB, et al. yositis and acute kidney injury in bacterial atypical pneumonia: Systematic literature review[J]. J Infect Public Health, 2020, 13(12): 2020-2024. doi: 10.1016/j.jiph.2020.10.007
[19] Chen DW, Yuan HB, Cao CC, et al. Impact of acute kidney injury on in-hospital outcomes in Chinese patients with community acquired pneumonia[J]. BMC Pulm Med, 2021, 21(1): 143. doi: 10.1186/s12890-021-01511-9
[20] Florenzano P, Cipriani C, Roszko KL, et al. Approach to patients with hypophosphataemia[J]. Lancet Diabetes Endocrinol, 2020, 8(2): 163-174. doi: 10.1016/S2213-8587(19)30426-7
[21] Kalantar-Zadeh K, Ganz T, Trumbo H, et al. Parenteral iron therapy and phosphorus homeostasis: a review[J]. Am J Hematol, 2021, 96(5): 606-616. doi: 10.1002/ajh.26100
[22] Morimoto Y, Ishiguro T, Uozumi R, et al. Significance of hypophosphatemia in patients with pneumonia[J]. Intern Med, 2022, 61(7): 979-988. doi: 10.2169/internalmedicine.6949-20
[23] Pistolesi V, Zeppilli L, Fiaccadori E, et al. Hypophosphatemia in critically ill patients with acute kidney injury on renal replacement therapies[J]. J Nephrol, 2019, 32(6): 895-908. doi: 10.1007/s40620-019-00648-5
[24] Schaefer B, Tobiasch M, Wagner S, et al. Hypophosphatemia after intravenous iron therapy: comprehensive review of clinical findings and recommendations for management[J]. Bone, 2022, 154: 116202. doi: 10.1016/j.bone.2021.116202
[25] Tebben PJ. Hypophosphatemia: a practical Guide to evaluation and management[J]. Endocr Pract, 2022, 28(10): 1091-1099. doi: 10.1016/j.eprac.2022.07.005
-




 下载:
下载: