Clinical characteristics of 73 patients with hemorrhagic fever with renal syndrome at emergency treatment stage
-
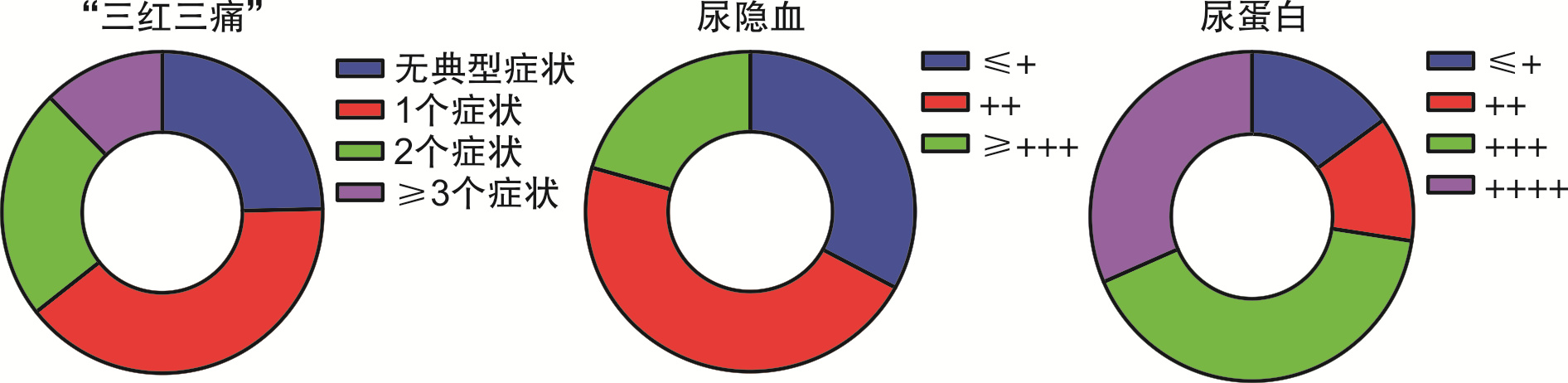
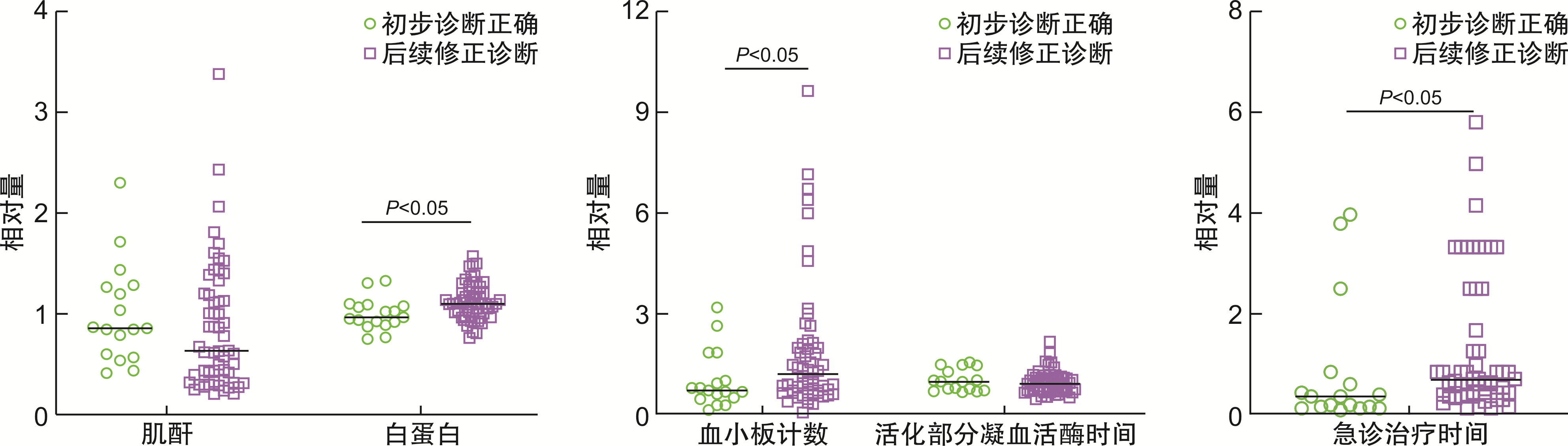
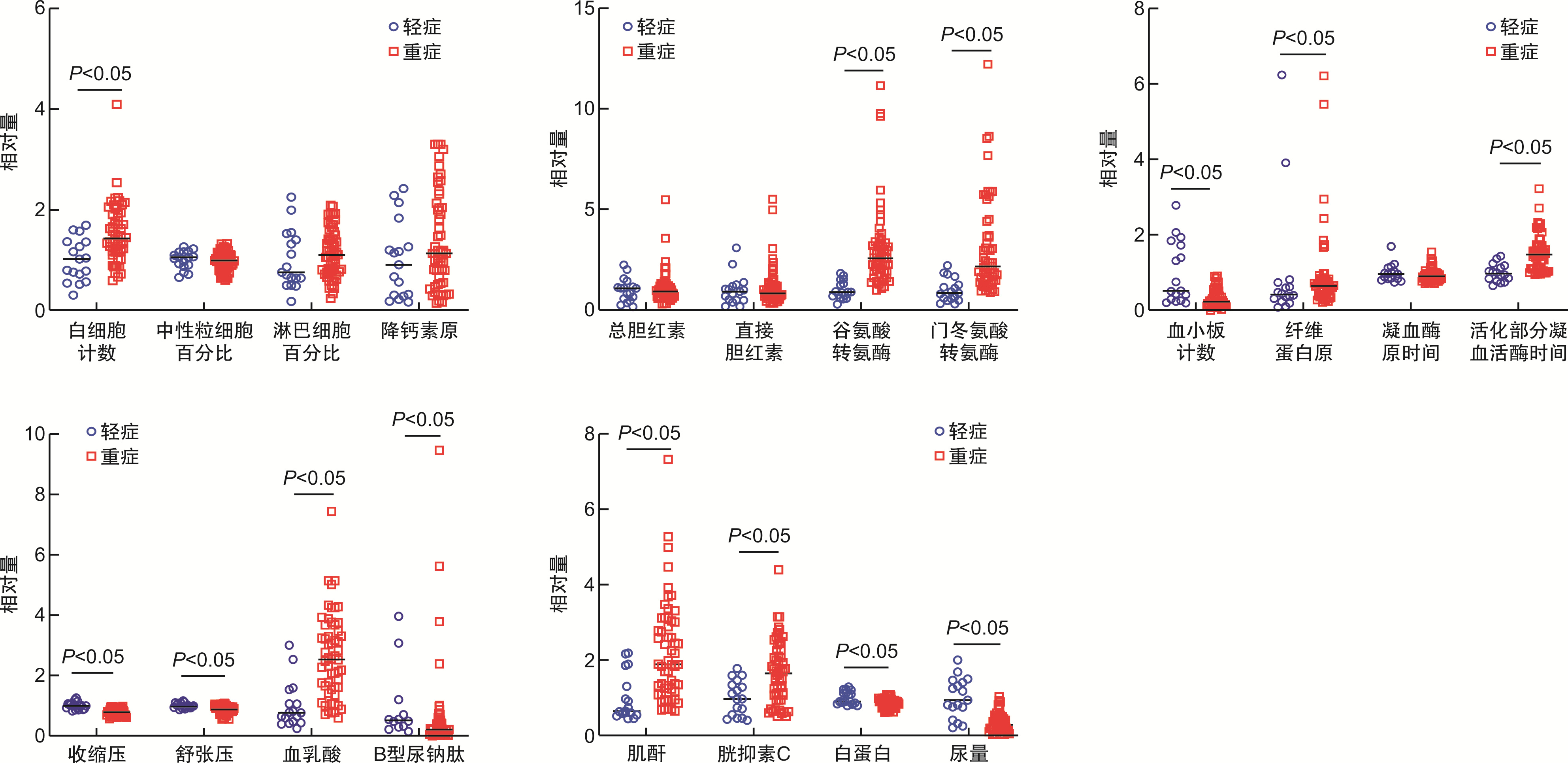
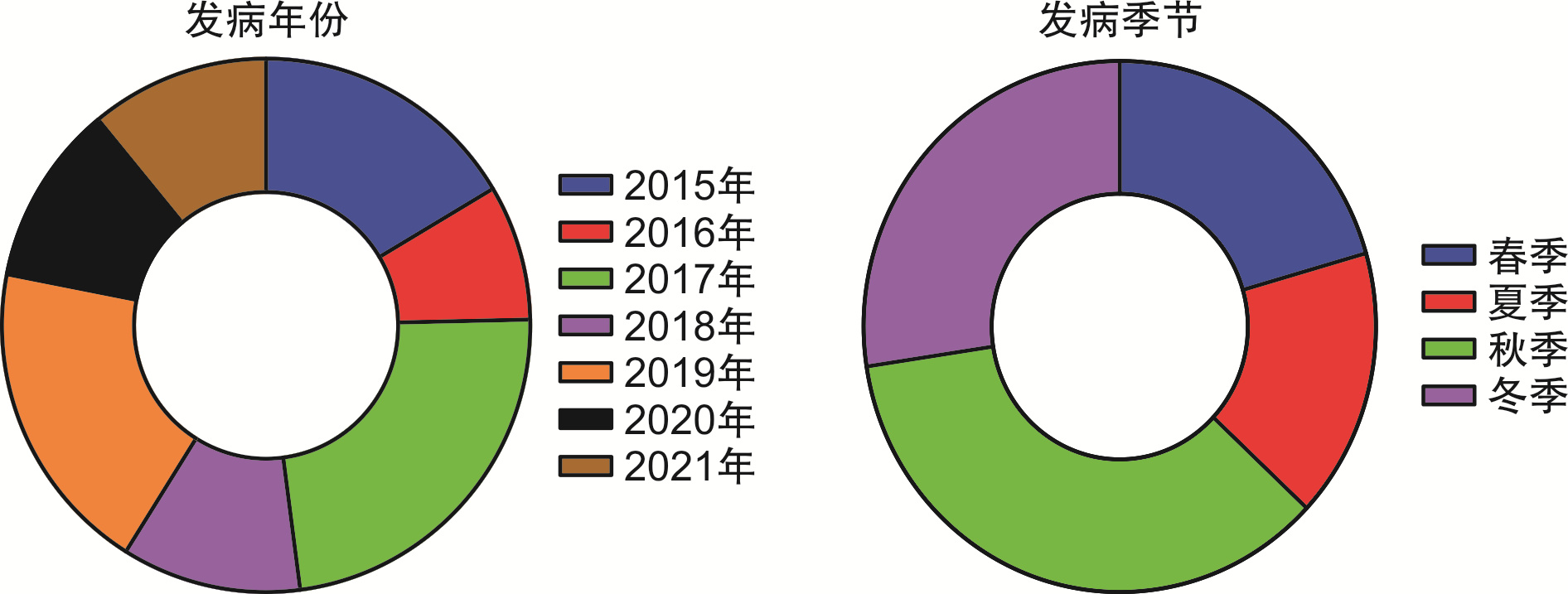
摘要: 目的 肾综合征出血热是一种急性自然疫源性疾病,低血压休克期和少尿期的患者多伴有代谢性酸中毒和肾脏功能障碍,重症者合并弥散性血管内凝血而危及生命,需要急诊抢救;然而部分患者“三红三痛”症状不典型,导致初诊正确率低和治疗的延误。分析出血热患者急诊救治阶段的临床特征和存在的问题,有助于优化出血热的早期救治策略。方法 本研究纳入一家三级甲等区域中心医院急诊科2015年1月—2021年12月收治的出血热患者。调查流行病学和急诊救治阶段的临床资料,包括患者典型症状、微循环功能、凝血功能、肾脏损伤、初诊正确率、抗病毒用药、急诊科治疗时间和患者预后等信息。比较轻症与重症、首诊正确与后续修正诊断组患者的临床特征。结果 ① 本组出血热患者共73例,平均年龄(44.6±17.5)岁,男性占71.2%,秋冬季发病占63.0%。39.7%的患者有明确或可疑鼠类接触史,确诊病例占86.3%;随访90 d,2例(2.7%)患者死亡。②急诊救治阶段平均17(10,42) h,24.7%就诊时无“三红三痛”症状,仅12.3%出现3个以上典型症状。67.1%患者血乳酸>2.0 mmol/L,34.2%患者血小板最低值< 20×109/L,50.7%的患者接受CRRT治疗,6.9%的患者入室24 h内接受抗病毒治疗。③初诊正确率仅为23.3%,初诊正确组患者尿蛋白≥(+++)占比76.5%,尿隐血≥(++)占比为88.2%。首次检验PLT 19×109/L,血清白蛋白28.47 g/L,均显著低于后续修正诊断组。④重症患者56例(76.7%),首次检验肌酐335.9 μmol/L,血乳酸4.3 mmol/L,均显著高于轻症组(P < 0.05)。76.8%的重症患者超声检查提示肾周积液,76.8%尿隐血≥(++)。结论 出血热患者急诊救治阶段仅少数有“三红三痛”典型症状,首诊正确率低,延误抗病毒治疗。秋冬季接诊发热伴肾脏损伤、血小板和白蛋白显著降低的患者时,急诊医生应尽早完善出血热抗体检验,优化早期综合救治措施以改善患者预后。Abstract: Objective Hemorrhagic fever with renal syndrome (HFRS) is an acute natural focus disease. Patients in hypotensive shock stage and oliguria stage are often accompanied by metabolic acidosis and renal dysfunction. The severe patients, accompanied by disseminated intravascular coagulation, are life-threatening and require emergency rescue. However, the symptoms of "three reds and three pains" in some patients are not typical, resulting in low accuracy of initial diagnosis and delayed treatment. Analyzing the clinical characteristics and existing problems in the emergency treatment stage of hemorrhagic fever patients is helpful to optimize the early treatment strategy of hemorrhagic fever.Methods Patients with hemorrhagic fever admitted to the emergency department of a tertiary class A regional central hospital from January 2015 to December 2021 were enrolled in this study. We investigated the clinical data at the stage of epidemiological and emergency treatment, including patient's typical symptoms, microcirculation function, blood coagulation function, kidney damage, accuracy of initial diagnosis, antiviral drugs, emergency department treatment time, and patient prognosis. The clinical characteristics of mild and severe patients, correct initial diagnosis and subsequent modified diagnosis were compared.Results ① There were 73 patients with HFRS in this group with an average age of (44.6±17.5) years, 71.2% of whom were male, and 63.0% of whom were infected in autumn and winter. 39.7% of the patients had definite or suspected contact history with rodents, and 86.3% of the confirmed cases. After 90 days of follow-up, 2 patients (2.7%) died. ②In the emergency treatment stage, the average time of emergency treatment was 17 (10, 42) hours. 24.7% of patients had no symptoms of "three reds and three pains", and only 12.3% had more than three typical symptoms. 67.1% of patients with blood lactic acid >2.0 mmol/L, 34.2% of patients with the lowest platelet < 20×109/L, 50.7% of patients received CRRT treatment, and 6.9% of patients received antiviral treatment within 24 hours after admission. ③The correct rate of initial diagnosis was only 23.3%, of which 76.5% were urinary protein content ≥ (+++), and 88.2% were urinary occult blood content ≥ (++). PLT 19×109/L, serum albumin 28.5 g/L and emergency treatment time (10 h) of the patients with correct initial diagnosis were significantly lower than those of the patients with modified diagnosis. ④The creatinine (335.9 μmol/L), blood lactic acid (4.3 mmol/L) were significantly higher in 56 patients with severe disease (76.7%) than those in the mild group (P < 0.05). 76.8% of severe patients showed perirenal effusion and 76.8% urinary occult blood content ≥(++).Conclusion Only a few patients with hemorrhagic fever have typical symptoms of "three reds and three pains" in the emergency treatment stage. The accuracy of the first diagnosis is low, and antiviral treatment is delayed. In autumn and winter, when receiving patients with fever accompanied by kidney damage and significant reduction of platelet and albumin, emergency physicians should arrange the test of hemorrhagic fever antibody as soon as possible to optimize early comprehensive treatment measures to improve the prognosis of patients.
-

-
表 1 73例出血热患者的临床资料和轻重症患者组间比较
项目 总体(n=73) 轻型+中型(n=17) 重型+危重型(n=56) 组间比较 t/Z P 年龄/岁 44.63±17.52 49.76±19.67 43.07±16.69 1.39 0.169 急诊治疗时间/h 17(10,42) 20(13.5,60) 17(9.25,34) 1.01 0.310 循环功能 收缩压/mmHg 115.55±20.16 137.41±16.84 108.91±16.03 6.35 < 0.001 舒张压/mmHg 72.12±11.23 80.18±6.74 69.68±11.22 3.65 < 0.001 血乳酸/(mmol·L-1) 3.52(1.7,5.48) 1.3(0.77,2.21) 4.29(2.63,6.16) 4.65 < 0.001 脑钠肽/(pg·mL-1) 916.6(314,2032) 771(221,1776) 1919(1107,3995) 2.47 0.014 肾脏功能 肌酐/(μmol·L-1) 292.93±198.15 151.29±94.65 335.93±201.77 -3.64 0.001 胱抑素C/(mg·L-1) 2.84±1.51 1.87±0.86 3.14±1.54 -3.24 0.002 血清白蛋白/(g·L-1) 31.15±5.15 34.9±6.04 30.01±4.29 3.72 < 0.001 入室24 h尿量/mL 560(200,1210) 1500(925,2300) 445(197.5,750) -4.58 < 0.001 凝血功能 血小板计数/(×109·L-1) 25(17,53.5) 50(27,169.5) 22.5(15,45.25) 3.68 < 0.001 纤维蛋白原/(mg·L-1) 16.78(10.57,22.68) 11.56(7.01,19.37) 17.69(11.77,23.32) 1.99 0.047 凝血时间/s 12.46±2.41 13.04±3.06 12.29±2.19 1.11 0.273 部分凝血酶原活化时/s 47(35,55.2) 33.5(27.35,40.23) 50.8(38.3,59.6) 4.41 < 0.001 肝脏功能 总胆红素/(μmol·L-1) 19.1(12.3,24.2) 21.8(10.35,26.25) 18.75(12.53,24.3) 0.12 0.901 直接胆红素/(μmol·L-1) 9.3(6.8,13.65) 10.1(5.45,13.4) 9.1(7.4,13.95) 0.56 0.575 丙氨酸氨基转移酶/(U·L-1) 74(47.5,108) 31(22.5,48.5) 88.5(66.25,115) -5.57 < 0.001 门冬氨酸氨基转移酶/(U·L-1) 116(71.5,191) 53(32.5,91) 135(92.5,229.75) -4.83 < 0.001 炎症反应 白细胞计数/(×109·L-1) 14.87±6.32 10.63±4.51 16.16±6.25 3.39 0.001 中性粒细胞/% 0.67±0.13 0.69±0.12 0.67±0.13 0.57 0.570 淋巴细胞/% 0.67±0.13 0.19±0.11 0.22±0.09 0.95 0.347 降钙素原/(ng·mL-1) 2.66(1.15,4.75) 2.13(0.68,3.65) 2.66(1.26,4.81) 1.29 0.199 表 2 初诊正确与修正诊断组出血热患者临床特征的比较
例(%) 临床特征 初诊正确(n=17) 后续修正(n=56) P 急诊治疗时间/h 10(3.5,20.5) 19.5(11.25,66) 0.010 血小板计数/(×109·L-1) 19(12.5,38.5) 32.5(17.5,56.25) 0.048 白蛋白/(g·L-1) 28.47±4.48 31.96±5.10 0.013 肌酐/(μmol·L-1) 327.59±162.65 282.41±207.89 0.414 血乳酸/(mmol·L-1) 3.52(2.1,4.95) 3.4(1.34,5.59) 0.634 谷氨酸转氨酶/(U·L-1) 78(50.5,107) 72.5(44.25,108) 0.589 白细胞计数/(×109·L-1) 17.23±8.26 14.16±5.49 0.079 “三红三痛”症状 0.062 无典型症状 3(17.6) 15(26.8) 1个典型症状 4(23.5) 25(44.6) 2个典型症状 5(29.4) 12(21.4) 3个典型症状 5(29.4) 4(7.1) 疾病程度 0.606 轻症 4(23.5) 13(23.2) 重症 13(76.5) 43(76.8) 鼠类接触史 0.261 无明确接触史 8(47.1) 36(64.3) 有或可疑接触史 9(52.9) 20(35.7) 肾脏超声 0.075 无肾损伤 9(52.9) 15(26.8) 肾脏损伤 8(47.1) 41(73.2) 尿蛋白 0.254 + 1(5.9) 10(17.9) ++ 3(17.6) 6(10.7) +++ 5(29.4) 25(44.6) ++++ 8(47.1) 15(26.8) 尿隐血 < 0.001 + 2(11.8) 22(39.3) ++ 3(17.6) 31(55.4) +++ 12(70.6) 3(5.4) 表 3 轻重症组出血热患者临床特征的比较
例(%) 临床特征 轻症(n=17) 重症(n=56) P “三红三痛”症状 0.014 无典型症状 9(52.94) 9(16.07) 1个典型症状 6(35.29) 23(41.07) 2个典型症状 2(11.76) 15(26.79) 3个典型症状 0 9(16.07) 肾脏超声 0.003 无肾损伤 11(64.71) 13(23.21) 肾周积液 6(35.29) 43(76.79) 胸腔积液 0.004 无胸腔积液 10(58.82) 15(26.79) 单侧胸腔积液 6(35.29) 19(33.93) 双侧胸腔积液 1(5.89) 22(39.29) 尿蛋白 < 0.001 + 7(41.18) 4(7.15) ++ 6(35.29) 3(5.36) +++ 3(17.65) 27(48.21) ++++ 1(5.89) 22(39.29) 尿隐血 0.007 + 11(64.71) 13(23.21) ++ 5(29.41) 29(51.79) +++ 1(5.89) 14(25.0) 初诊正确与否 0.327 初次诊断正确 2(11.76) 15(26.79) 后续修正诊断 15(88.24) 41(73.21) -
[1] 杨爱新, 高志良, 刘静. 《肾综合征出血热防治专家共识》解读[J]. 临床内科杂志, 2021, 38(12): 862-864. https://www.cnki.com.cn/Article/CJFDTOTAL-LCLZ202112023.htm
[2] Tariq M, Kim DM. Hemorrhagic fever with renal syndrome: literature review, epidemiology, clinical picture and pathogenesis[J]. Infect Chemother, 2022, 54(1): 1-19. doi: 10.3947/ic.2021.0148
[3] Liang W, Gu X, Li X, et al. Mapping the epidemic changes and risks of hemorrhagic fever with renal syndrome in Shaanxi Province, China, 2005-2016[J]. Sci Rep, 2018, 8(1): 749-758. doi: 10.1038/s41598-017-18819-4
[4] 王芹, 李建东, 张全福, 等. 2014年全国肾综合征出血热监测总结和疫情分析[J]. 疾病监测, 2016, 31(3): 192-199. https://www.cnki.com.cn/Article/CJFDTOTAL-JBJC201603007.htm
[5] 黄长形, 姜泓, 白雪帆, 等. 肾综合征出血热诊疗陕西省专家共识[J]. 陕西医学杂志, 2019, 48(3): 275-288. doi: 10.3969/j.issn.1000-7377.2019.03.001
[6] 刘天, 童叶青, 刘漫, 等. 2004—2017年全国肾综合征出血热变化趋势分析[J]. 中国人兽共患病学报, 2022, 38(6): 515-522, 547. https://www.cnki.com.cn/Article/CJFDTOTAL-ZRSZ202206010.htm
[7] 宇应涛, 郭争社, 董雯婷, 等. 2003—2019年西安市某三级甲等医院肾综合征出血热患者特征分析[J]. 中国卫生统计, 2021, 38(1): 100-103. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWT202101026.htm
[8] 中华预防医学会感染性疾病防控分会, 中华医学会感染病学分会. 肾综合征出血热防治专家共识[J]. 中华传染病杂志, 2021, 39(5): 257-265. doi: 10.3760/cma.j.cn311365-20210224-00067
[9] 高君兰, 于健, 王之余, 等. 74例肾综合征出血热的流行病学及临床特征分析[J]. 大连医科大学学报, 2019, 41(6): 521-524. https://www.cnki.com.cn/Article/CJFDTOTAL-DLYK201906012.htm
[10] 王姿欢, 孙玉兰, 陈艳伟, 等. 2015—2020年北京市肾综合征出血热流行病学特征分析[J]. 中国人兽共患病学报, 2022, 38(3): 256-259. https://www.cnki.com.cn/Article/CJFDTOTAL-ZRSZ202203011.htm
[11] 何月悦. 流行性出血热流行特征和预防控制措施分析[J]. 中国实用医药, 2022, 17(17): 182-184. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA202217055.htm
[12] 朱妮, 刘峰, 邱琳, 等. 2011—2015年陕西省肾综合征出血热时空聚集性分析[J]. 现代预防医学, 2017, 44(9): 1537-1540, 1552. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF201709001.htm
[13] 杨冰心, 陈小雪, 邢燕, 等. 3例表现为急性胰腺炎的肾综合征出血热的诊断思路及文献复习[J]. 临床急诊杂志, 2019, 20(4): 328-330. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC201904018.htm
[14] 彭昱, 李铁丰, 陈梅, 等. 立克次体感染伴发脾动脉畸形破裂1例[J]. 中华地方病学杂志, 2022, 41(8): 677-678.
[15] 支晓丽, 戴仲秋. 细菌性肝脓肿误诊为肾综合征出血热10例分析[J]. 中西医结合心血管病电子杂志, 2020, 8(33): 189, 198. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXJH202033134.htm
[16] 鲁柏涛, 赵鸣雁. 104例肾病综合征出血热流行病学及临床特点的回顾性分析[J]. 中华地方病学杂志, 2015, 34(10): 769-772.
[17] 张国明, 何溪, 刘昶权, 等. 53例肾综合征出血热的临床特征及误诊分析[J]. 岭南急诊医学杂志, 2021, 26(4): 352-355. https://www.cnki.com.cn/Article/CJFDTOTAL-LNJZ202104007.htm
[18] 郝俊峰, 王丹, 朱海宁. 血常规和尿常规检查在流行性出血热早期诊断应用的效果观察[J]. 健康大视野, 2020(7): 39.
[19] 赵禹. 流行性出血热IgM抗体实验室检测结果分析[J]. 中国现代医生, 2020, 58(12): 147-149. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS202012049.htm
[20] 刘畅, 毛国群, 杨光钊, 等. 78例肾综合征出血热多器官损害的临床特征及影像学表现[J]. 放射学实践, 2021, 36(2): 206-210. https://www.cnki.com.cn/Article/CJFDTOTAL-FSXS202102015.htm
[21] 胡兰苹. 肾综合征出血热患者CT表现及改变及临床应用价值研究[J]. 中国CT和MRI杂志, 2022, 20(7): 121-123. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR202207039.htm
[22] 张克恭, 张野, 武小青, 等. 中性粒细胞与肾综合征出血热危重化关系临床研究[J]. 陕西医学杂志, 2020, 49(6): 695-698, 703. https://www.cnki.com.cn/Article/CJFDTOTAL-SXYZ202006014.htm
[23] 张茹辉, 潘俊均, 洪江. 降钙素原、超敏C-反应蛋白、D-二聚体与血小板联合检测在肾综合征出血热诊断中的应用[J]. 中国社区医师, 2021, 37(11): 110-111. https://www.cnki.com.cn/Article/CJFDTOTAL-XCYS202111052.htm
[24] 杨凯. 流行性出血热患者死亡危险因素的调查分析[J]. 护理实践与研究, 2022, 19(2): 200-203. https://www.cnki.com.cn/Article/CJFDTOTAL-HLSJ202202009.htm
[25] Huggins JW, Hsiang CM, Cosgriff TM, et al. Prospective, double-blind, concurrent, placebo-controlled clinical trial of intravenous ribavirin therapy of hemorrhagic fever with renal syndrome[J]. J Infect Dis, 1991, 164(6): 1119-1127.
[26] Rusnak JM, Byrne WR, Chung KN, et al. Experience with intravenous ribavirin in the treatment of hemorrhagic fever with renal syndrome in Korea[J]. Antiviral Res, 2009, 81(1): 68-76.
[27] Malinin OV, Platonov AE. Insufficient efficacy and safety of intravenous ribavirin in treatment of haemorrhagic fever with renal syndrome caused by Puumala virus[J]. Infect Dis(Lond), 2017, 49(7): 514-520.
[28] Safronetz D, Falzarano D, Scott DP, et al. Antiviral efficacy of favipiravir against two prominent etiological agents of hantavirus pulmonary syndrome[J]. Antimicrob Agents Chemother, 2013, 57(10): 4673-4680.
[29] 张峰典, 张颖, 李文娟, 等. 两种工艺制备双价肾综合征出血热灭活疫苗的安全性及免疫原性评价[J]. 中国生物制品学杂志, 2022, 35(2): 129-132, 137. https://www.cnki.com.cn/Article/CJFDTOTAL-SWZP202202001.htm
[30] 王艳旭, 吴晓敏, 李明春, 等. 肾综合征出血热疫苗接种认知及影响因素分析[J]. 中国初级卫生保健, 2021, 35(1): 72-74. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCW202101025.htm
-




 下载:
下载: