Risk factors of acute respiratory distress syndrome caused by pyogenic liver abscess
-
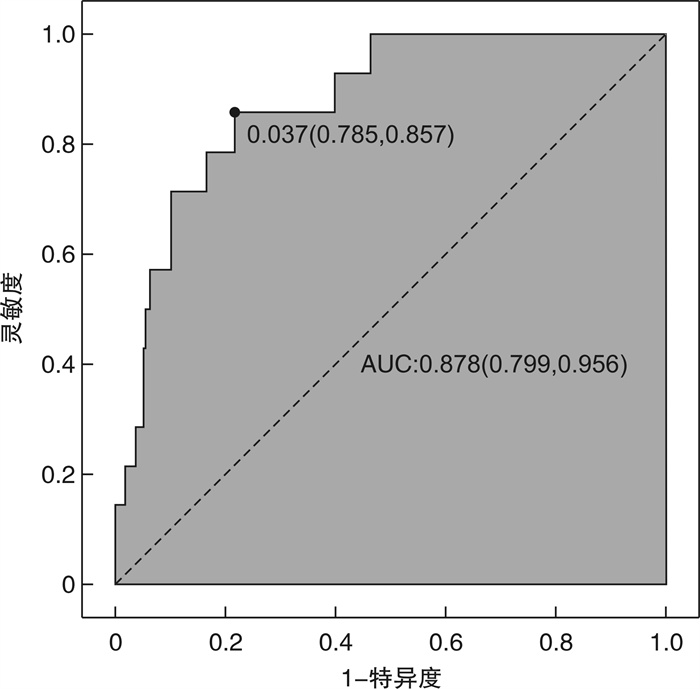
摘要: 目的 探讨细菌性肝脓肿(PLA)导致急性呼吸窘迫综合征(ARDS)的危险因素。方法 对湖南省人民医院2019年1月—2022年6月收住院治疗的922例PLA患者的临床资料进行回顾性分析。根据是否发生ARDS,分为ARDS组和非ARDS组,比较2组患者间临床特征,分析2组患者的一般临床资料、实验室及影像学结果,通过单因素和多因素logistic分析PLA导致ARDS的危险因素,采用受试者工作特征(ROC)曲线评价相关危险因素对发生ARDS的预测价值,探讨PLA致ARDS的危险因素及早期诊断生物标志物。结果 922例PLA患者中48例(5.21%)发生ARDS。多因素logistic回归模型发现性别、脓毒性休克、CRP、ALB为PLA发生ARDS的独立预测因素。女性患者发生ARDS的风险是男性患者的0.18倍(OR=0.18,95%CI:0.04~0.94,P=0.042);发生脓毒性休克患者是未发生脓毒性休克患者发生ARDS风险的3.58倍(OR=3.58,95%CI:1.49~8.61,P=0.004);CRP每增加1 mg/L发生ARDS的风险增加1%(OR=1.01,95%CI:1.00~1.02,P=0.002);ALB每增加1 g/L,发生ARDS的风险下降22%(OR=0.78,95%CI:0.67~0.78,P=0.002)。联合4项独立因素预测PLA患者发生ARDS的AUC为0.878(95%CI:0.799~0.956),灵敏度为85.7%,特异度为78.5%。结论 性别、脓毒性休克、CRP、ALB为PLA发生急性呼吸窘迫综合征的独立预测因素,结合上述4个因素对PLA患者导致ARDS的预测价值高。Abstract: Objective To explore the related factors of acute respiratory distress syndrome(ARDS) induced by pyogenic liver abscess(PLA).Methods The clinical data of 922 patients with liver abscess admitted to Hunan People's Hospital from January 2019 to June 2022 were analyzed retrospectively. According to the occurrence of ARDS, the patients were divided into ARDS Group and non-ARDS group, the clinical characteristics, general clinical data, laboratory and imaging results were compared between the two groups. The risk factors of ARDS in patients with PLA were analyzed by univariate and multivariate logistic regression analysis, receiver operating characteristic(ROC) curve was used to evaluate the predictive value of risk factors for ARDS, and to explore the risk factors and biomarkers for early diagnosis of ARDS caused by PLA.Results The incidence of ARDS was 5.21%(48/922) in patients with PLA. Multiple Logistic regression model found that gender, Septic Shock, CRP and ALB were independent predictors of the occurrence of ARDS in PLA. The risk of ARDS in female patients is 0.18 times higher than that in male patients (OR=0.18, 95%CI: 0.04-0.94, P=0.042); The risk of ARDS in patients with septic shock was 3.58 times higher than that in patients without septic shock(OR=3.58, 95%CI: 1.49-8.61, P=0.004); The risk of ARDS increases by 1% for every 1 mg/L increase in CRP(OR=1.01, 95%CI: 1.00-1.02, P=0.002), and for every 1 g/L increase in ALB, the risk of ARDS decreases by 22%(OR=0.78, 95%CI: 0.67-0.78, P=0.002). The AUC for predicting ARDS in PLA patients by combining four independent factors was 0.878(95%CI: 0.799-0.956), the sensitivity was 85.7% and the specificity was 78.5%.Conclusion Gender, Septic Shock, CRP and ALB were the independent predictive factors of ARDS in PLA patients. Combined with the above four factors, it has high predictive value for PLA patients to cause ARDS.
-
Key words:
- pyogenic liver abscess /
- acute respiratory distress syndrome /
- sepsis
-

-
表 1 ARDS组和非ARDS组一般资料比较
例(%),X±S 变量 总例数(n=922) ARDS组(n=48) 非ARDS组(n=874) χ2 P 性别 6.211 0.013 男 492(53.4) 34(70.8) 458(52.4) 女 430(46.6) 14(29.2) 416(47.6) 年龄/岁 59.4±12.2 62.3±12.7 59.2±12.2 2.883 0.09 病因 Fisher 0.108 隐源性 275(29.8) 7(14.6) 268(30.7) 糖尿病 223(24.2) 18(37.5) 205(23.5) 胆道结石 280(30.4) 14(29.2) 266(30.4) 腹腔感染 3(0.3) 0(0) 3(0.3) 侵入操作 10(1.1) 0(0) 10(1.1) 肝CA 31(3.4) 1(2.1) 30(3.4) 合并2种以上 100(10.8) 8(16.7) 92(10.5) 表 2 ARDS组和非ARDS组实验室指标及临床资料比较
例(%),X±S 变量 总计(n=922) ARDS组(n=48) 非ARDS组(n=874) χ2 P WBC/(×109·L-1) 11.0±22.5 12.3±6.2 10.9±23.0 0.177 0.674 PLT/(×109·L-1) 231.7±141.8 199.9±137.6 233.5±141.8 2.56 0.110 CRP/(mg·L-1) 104.7±77.9 180.4±85.4 101.3±76.0 19.507 < 0.001 PCT/(μg·L-1) 9.2±21.0 23.7±31.3 8.5±20.2 10.193 0.002 ALB/(g·L-1) 32.1±5.7 27.9±3.5 32.2±5.7 11.013 < 0.001 Cr/(μmmol·L-1) 79.1±178.3 81.1±70.9 78.9±182.4 0.007 0.934 TBil/(μmmol·L-1) 34.7±73.7 36.6±51.8 34.6±74.7 0.035 0.853 DBil/(μmmol·L-1) 27.4±98.8 25.1±41.0 27.6±101.0 0.027 0.869 ALT/(U·L-1) 67.2±190.7 105.0±140.8 65.2±192.9 1.983 0.159 AST/(U·L-1) 73.1±228.2 114.6±205.5 70.8±229.3 1.677 0.196 脓毒症 4.203 0.040 无 815(88.4) 38(79.2) 777(88.9) 有 107(11.6) 10(20.8) 97(11.1) 脓毒性休克 Fisher 0.006 无 878(95.2) 41(85.4) 837(95.8) 有 44(4.8) 7(14.6) 37(4.2) 表 3 ARDS组与非ARDS组影像学资料比较
例(%) 变量 总计(n=922) ARDS组(n=48) 非ARDS组(n=874) χ2 P 多发肝脓肿 0.042 0.837 否 570(61.8) 29(60.4) 541(61.9) 是 352(38.2) 19(39.6) 333(38.1) 肝脓肿部位 Fisher 0.886 左叶 246(26.7) 12(25.0) 234(26.8) 右叶 572(62.0) 30(62.5) 542(62.0) 尾叶 14(1.5) 0(0) 14(1.6) 两叶以上 90(9.8) 6(12.5) 84(9.6) 肝脓肿大小/cm 2.360 0.307 < 5 340(36.9) 13(27.1) 327(37.4) 5~10 420(45.6) 24(50) 396(45.3) >10 162(17.6) 11(22.9) 151(17.3) 胸腔积液 8.530 0.003 无 496(53.8) 16(33.3) 480(54.9) 有 426(46.2) 32(66.7) 394(45.1) 表 4 PLA致ARDS的单因素及多因素logistic回归分析
变量 总计 例(%) 单因素OR(95%CI) P 多因素OR(95%CI) P 性别 男 492 34(6.9) 1(Ref) 1(Ref) 女 430 14(3.3) 0.45(0.24~0.86) 0.015 0.18(0.04~0.94) 0.042 胸腔积液 无 496 16(3.2) 1(Ref) 1(Ref) 有 426 32(7.5) 2.44(1.32~4.51) 0.005 1.18(0.30~4.56) 0.813 脓毒症 无 815 38(4.7) 1(Ref) 1(Ref) 有 107 10(9.3) 2.11(1.02~4.36) 0.045 0.27(0.03~2.84) 0.275 脓毒性休克 无 878 41(4.7) 1(Ref) 1(Ref) 有 44 7(15.9) 3.86(1.62~9.19) 0.002 3.58(1.49~8.61) 0.004 CRP 922 48(5.2) 1.01(1.01~1.02) < 0.001 1.01(1.00~1.02) 0.002 PCT 922 48(5.2) 1.02(1.01~1.03) 0.004 0.99(0.96~1.02) 0.509 ALB 922 48(5.2) 0.86(0.79~0.94) 0.001 0.78(0.67~0.91) 0.002 表 5 CRP、ALB、性别、脓毒性休克及联合4项指标对PLA患者发生ARDS的预测价值
指标 截断值 AUC 95%CI 灵敏度/% 特异度/% 阳性预测值/% 阴性预测值/% CRP/(mg·L-1) 117.5 0.760 0.655~0.864 84.2 59.3 83.8 98.8 ALB/(g·L-1) 32.02 0.730 0.649~0.811 95.0 51.0 63.5 99.7 性别 0.592 0.525~0.659 70.8 47.6 69.1 96.7 脓毒性休克 0.552 0.501~0.603 14.6 95.8 15.9 95.3 4项指标联合 0.878 0.799~0.956 85.7 78.5 13.5 99.3 -
[1] Lo JZW, Leow JJJ, Ng PLF, et al. Predictors of therapy failure in a series of 741 adult pyogenic liver abscesses[J]. J Hepatobiliary Pancreat Sci, 2015, 22(2): 156-165. doi: 10.1002/jhbp.174
[2] 齐文旗, 黄椿媚, 边帆, 等. 肝脓肿致脓毒血症的危险因素及早期诊断[J]. 中华急诊医学杂志, 2019, 28(11): 1383-1389. doi: 10.3760/cma.j.issn.1671-0282.2019.11.010
[3] Zhou JF, Qian CY, Zhao MY, et al. Epidemiology and outcome of severe sepsis and septic shock in intensive care units in mainland China[J]. PLoS One, 2014, 9(9): e107181. doi: 10.1371/journal.pone.0107181
[4] 张勤, 胡相悦. 血清KL-6, sTM, CC-16对脓毒症并发急性呼吸窘迫综合征患者预后的价值研究[J]. 临床急诊杂志, 2020, 21(9): 711-716. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202009007.htm
[5] Chen Y, Qiu CH, Cai WR. Identification of key immune genes for sepsis-induced ARDS based on bioinformatics analysis[J]. Bioengineered, 2022, 13(1): 697-708. doi: 10.1080/21655979.2021.2012621
[6] Force ARDSDT, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition[J]. JAMA, 2012, 307(23): 2526-2533.
[7] Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315(8): 762-774. doi: 10.1001/jama.2016.0288
[8] Longworth S, Han J. Pyogenic liver abscess[J]. Clin Liver Dis, 2015, 6(2): 51-54. doi: 10.1002/cld.487
[9] 中华医学会急诊医学分会. 细菌性肝脓肿诊治急诊专家共识[J]. 中华急诊医学杂志, 2022, 31(3): 273-280.
[10] 陈曦, 付春毅, 张新超. 肺炎克雷伯菌肝脓肿侵袭性综合征10例临床分析[J]. 临床急诊杂志, 2020, 21(6): 451-455. doi: 10.13201/j.issn.1009-5918.2020.06.006
[11] Meyer NJ, Gattinoni L, Calfee CS. Acute respiratory distress syndrome[J]. Lancet, 2021, 398(10300): 622-637. doi: 10.1016/S0140-6736(21)00439-6
[12] 何超, 黄增相, 陶骅, 等. 严重脓毒症性急性呼吸窘迫综合征患者血管外肺水的变化以及乌司他丁的作用[J]. 中国呼吸与危重监护杂志, 2015, 14(3): 291-294. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGHW201503021.htm
[13] Gupta A, Bhatti S, Leytin A, et al. Novel complication of an emerging disease: Invasive Klebsiella pneumoniae liver abscess syndrome as a cause of acute respiratory distress syndrome[J]. Clin Pract, 2018, 8(1): 1021. doi: 10.4081/cp.2018.1021
[14] 唐瑜, 吕健, 张丽茹, 等. 脓毒症早期识别的研究进展[J]. 临床急诊杂志, 2022, 23(7): 513-518. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.07.011
[15] Chen H, Cheng ZB, Yu RG. Procalcitonin as a predictor of moderate to severe acute respiratory distress syndrome after cardiac surgery with cardiopulmonary bypass: a study protocol for a prospective cohort study[J]. BMJ Open, 2014, 4(10): e006344. doi: 10.1136/bmjopen-2014-006344
[16] Komiya K, Ishii H, Murakami J, et al. Comparison of chest computed tomography features in the acute phase of cardiogenic pulmonary edema and acute respiratory distress syndrome on arrival at the emergency department[J]. J Thorac Imaging, 2013, 28(5): 322-328. doi: 10.1097/RTI.0b013e31828d40b2
[17] Fanali G, di Masi A, Trezza V, et al. Human serum albumin: from bench to bedside[J]. Mol Aspects Med, 2012, 33(3): 209-290. doi: 10.1016/j.mam.2011.12.002
[18] McNeil JB, Jackson KE, Wang CX, et al. Linear association between hypoalbuminemia and increased risk of acute respiratory distress syndrome in critically ill adults[J]. Crit Care Explor, 2021, 3(9): e0527. doi: 10.1097/CCE.0000000000000527
[19] Hoeboer SH, Oudemans-van Straaten HM, Groeneveld ABJ. Albumin rather than C-reactive protein may be valuable in predicting and monitoring the severity and course of acute respiratory distress syndrome in critically ill patients with or at risk for the syndrome after new onset fever[J]. BMC Pulm Med, 2015, 15: 22. doi: 10.1186/s12890-015-0015-1
[20] Regitz-Zagrosek V, Kararigas G. Mechanistic Pathways of Sex Differences in Cardiovascular Disease[J]. Physiol Rev, 2017, 97(1): 1-37. doi: 10.1152/physrev.00021.2015
[21] He SJ, Yu J, Wang HR, et al. Percutaneous fine-needle aspiration for pyogenic liver abscess(3-6 cm): a two-center retrospective study[J]. BMC Infect Dis, 2020, 20(1): 516. doi: 10.1186/s12879-020-05239-5
[22] Erfinanda L, Ravindran K, Kohse F, et al. Oestrogen-mediated upregulation of the Mas receptor contributes to sex differences in acute lung injury and lung vascular barrier regulation[J]. Eur Respir J, 2021, 57(1): 2000921. doi: 10.1183/13993003.00921-2020
[23] 葛庆岗, 姚智渊, 王铁华, 等, 急性呼吸窘迫综合征发生及预后危险因素的多中心前瞻性队列研究[J]. 中华危重病急救医学, 2014, 26(11): 773-779.
[24] Heffernan DS, Dossett LA, Lightfoot MA, et al. Gender and acute respiratory distress syndrome in critically injured adults: a prospective study[J]. J Trauma, 2011, 71(4): 878-883, 885.
[25] Grieco DL, Maggiore SM, Roca O, et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS[J]. Intensive Care Med, 2021, 47(8): 851-866.
-




 下载:
下载: