Risk factors analysis and prediction model construction of hospital death in patients with hollow viscera perforation
-
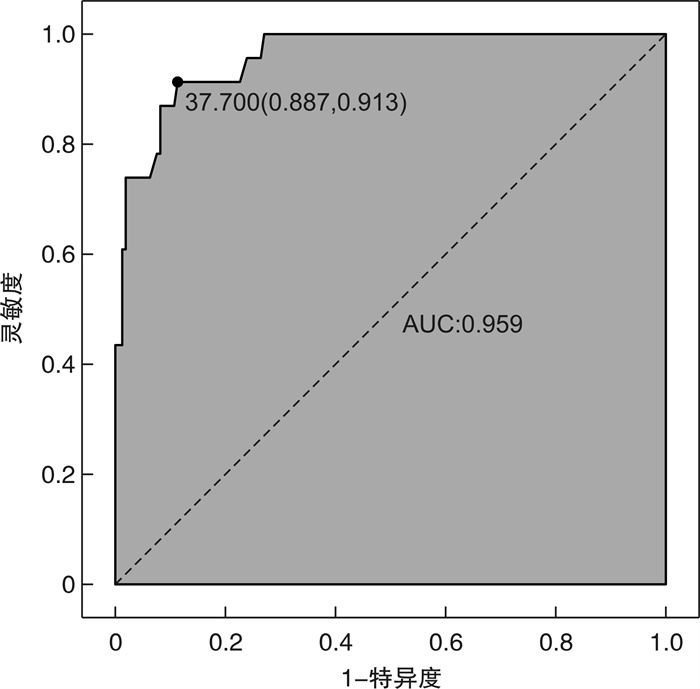
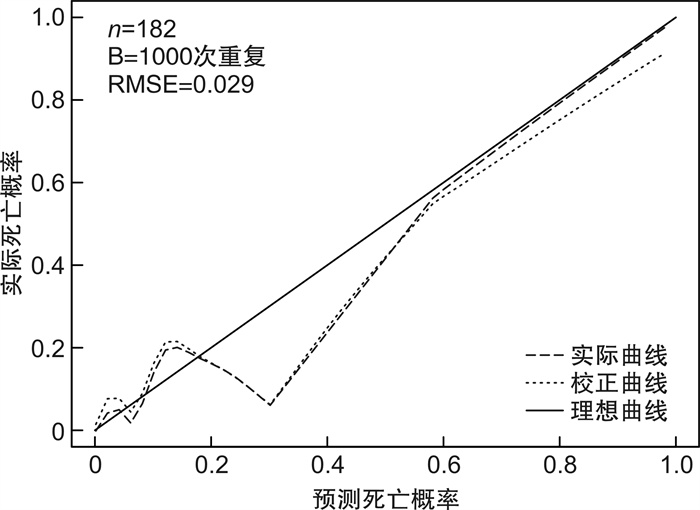
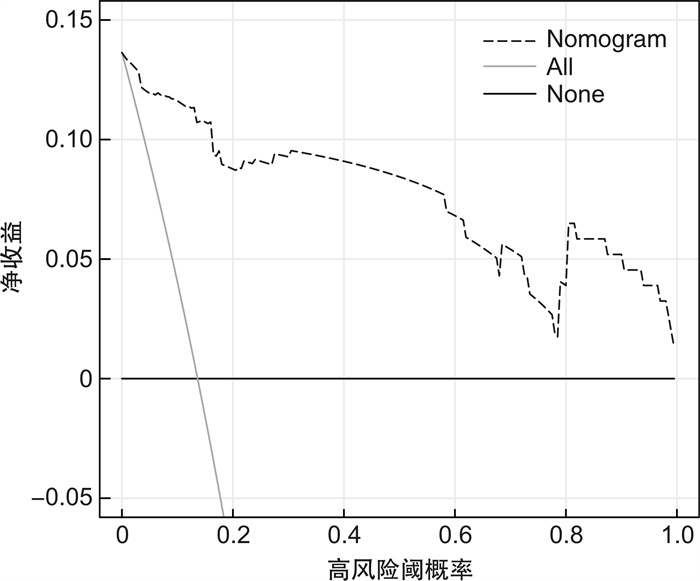
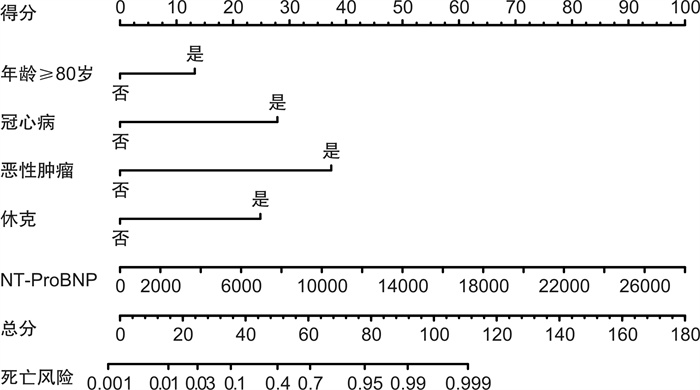
摘要: 目的 分析导致空腔脏器穿孔患者死亡的危险因素并建立预测模型,为临床医生提供便捷有效的预测方法。方法 回顾性收集2019年1月—2022年6月我院急诊科收治的空腔脏器穿孔患者为研究对象。包括患者的一般临床资料,入院第1天的生命体征、既往病史及实验室检查结果、是否进行外科手术、住院天数(总住院天数与ICU住院天数)、病情转归等,对上述指标进行统计学分析并构建列线图。结果 本研究最终纳入182例患者,根据最终是否死亡分为死亡组及存活组。将2组患者基线资料进行单因素以及logistic多因素回归分析后,得出年龄≥80岁、冠心病、休克、恶性肿瘤、NT-ProBNP是空腔脏器穿孔患者短期不良预后的5个独立危险因素。基于上述独立影响因素构建列线图,通过绘制ROC曲线并计算曲线下面积(AUC值)来评估其区分度,通过R语言程序包绘制校准曲线并计算均方根误差(RMSE)来评估模型准确度,结果显示,该模型具有较好的区分度(AUC=0.959)和均方根误差(RMSE=0.029),利用约登指数计算其灵敏度及特异度,该模型的灵敏度为91.3%,特异度为88.7%;决策曲线分析也显示出该列线图具有较高的临床获益性。结论 本文通过单因素及多因素分析后得出的空腔脏器穿孔患者的短期不良预后的独立危险因素包括年龄≥80岁、冠心病、休克、恶性肿瘤、NT-ProBNP。将这5个指标联合,建立预测性能较好的评估患者死亡风险的列线图,为临床医生提供简单有效的预测方法。Abstract: Objective To analyze the risk factors leading to the death of patients with hollow viscera perforation and to establish a prediction model to provide clinicians with a convenient and effective prediction method and accurate treatment timing to reduce the mortality of patients.Methods Patients with hollow viscera perforation admitted to our hospital from from January 2019 to June 2022 were retrospectively collected as research subjects. The general clinical data of the patients were collected, including vital signs on the first day of admission, previous medical history and laboratory test results, whether to perform surgery, days of hospitalization(total hospitalization days and ICU days), and prognosis. Statistical analysis of the above indicators is conducted and a nomogram is constructed.Results This study finally included 182 patients, who were divided into death group and survival group according to whether they died or not. Univariate and logistic multivariate regression analysis was performed on the baseline data of the two groups, and it was concluded that age ≥80, coronary heart disease, shock, malignant tumor, and NT-ProBNP were five independent risk factors for poor short-term prognosis of patients with hollow viscera perforation. A nomogram was constructed based on the above independent influencing factors, and the discrimination was evaluated by drawing the ROC curve and calculating the AUC value. The R language package was used to draw the calibration curve and calculate the root mean square error(RMSE) to evaluate the model accuracy. The results showed that the model had good discrimination(AUC=0.959) and root mean square error(RMSE=0.029). The Youden index was used to calculate its sensitivity and specificity. The sensitivity of the model was 91.3% and the specificity was 88.7%. Decision curve analysis also showed that the nomogram had a high clinical benefit.Conclusion The independent risk factors for poor short-term prognosis of patients with hollow viscera perforation obtained by univariate and multivariate analysis included age ≥80, coronary heart disease, shock, malignant tumor, and NT-ProBNP. Combining these five indicators, a nomogram with better predictive performance was established to assess patient risk, providing clinicians with a simple and effective prediction method and reducing patient mortality.
-
Key words:
- hollow viscera perforation /
- death /
- risk factors /
- nomogram /
- prediction model
-

-
表 1 空腔脏器穿孔患者的基线特征
M(P25,P75) 指标 死亡组(n=23,12.6%) 存活组(n=159,87.4%) χ2/Z P 男性/例(%) 13(56.5) 122(76.7) 4.284 0.038 年龄/岁 78.0(66.0,84.0) 62.0(45.0,73.0) -4.130 < 0.001 体温/℃ 36.5(36.3,36.7) 36.5(36.4,36.7) -0.043 0.966 呼吸/(次·min-1) 20.0(19.0,23.0) 20.0(18.0,20.0) -1.539 0.124 休克/例(%) 19(82.6) 24(15.1) 50.758 < 0.001 吸烟/例(%) 8(34.8) 32(20.1) 2.517 0.113 饮酒/例(%) 4(17.4) 24(15.1) 0.081 0.775 高血压/例(%) 11(47.8) 37(23.2) 6.240 0.012 糖尿病/例(%) 3(13.0) 11(6.9) 1.062 0.303 冠心病/例(%) 5(21.7) 4(2.5) 15.797 < 0.001 肾功能不全/例(%) 1(4.3) 3(1.9) 0.566 0.452 消化性溃疡/例(%) 1(4.3) 13(8.2) 0.415 0.520 恶性肿瘤/例(%) 6(20.0) 14(8.5) 6.135 0.013 WBC/(×109/L) 5.3(3.2,9.1) 10.1(7.0,14.1) -3.940 < 0.001 N%/% 87.2(75.5,90.7) 87.3(78.7,91.5) -0.169 0.865 Hb/(g·L-1) 122.0(97.0,137.0) 133.0(116.0,149.0) -1.787 0.074 PLT/(×109/L) 163.0(119.0,211.0) 219.0(169.0,263.0) -3.132 0.002 NT-ProBNP/(pg·mL-1) 5376.0(700.0,13654.0) 497.0(222.74,923.0) -4.800 < 0.001 ALT/(U·L-1) 14.0(12.0,25.0) 15.0(11.0,22.0) -0.131 0.895 ALB/(g·L-1) 32.7(25.5,37.9) 38.2(32.4,42.5) -3.807 < 0.001 下消化道穿孔/例(%) 14(60.9) 54(34.0) 6.216 0.013 急诊手术/例(%) 18(78.3) 135(84.9) 0.662 0.416 心肌损伤/例(%) 16(69.6) 19(11.9) 42.943 < 0.001 脓毒血症/例(%) 20(100.0) 46(26.4) 29.271 < 0.001 机械通气天数/d 1.0(0.0,3.0) 0.0(0.0,0.0) -6.348 < 0.001 ICU住院天数/d 2.0(0.0,5.0) 0.0(0.0,1.0) -4.084 < 0.001 总住院天数/d 4.0(2.0,13.0) 12.0(9.0,17.0) -3.818 < 0.001 表 2 空腔脏器穿孔患者院内死亡的多因素logistic回归分析
指标 回归系数(β) 标准误(S.E.) OR(95%CI) P 年龄≥80岁 3.530 1.770 34.118(1.063,1095.425) 0.046 性别 -0.872 1.146 0.418(0.044,3.950) 0.446 冠心病(CHD)史 5.174 2.058 176.652(3.128,9974.775) 0.012 恶性肿瘤史 6.038 2.154 418.868(6.150,28528.819) 0.005 休克 3.725 1.605 41.465(1.786,962.692) 0.020 NT-ProBNP 0.001 0.000 1.001(1.000,1.001) 0.006 WBC -0.236 0.124 0.790(0.619,1.008) 0.058 ALB 0.030 0.058 1.031(0.920,1.154) 0.602 高血压史 0.612 1.098 1.843(0.214,15.871) 0.578 下消化道穿孔 3.104 1.647 22.290(0.884,562.135) 0.059 -
[1] 党云超. 螺旋CT在腹部空腔脏器破裂穿孔中的应用价值分析[J]. 内蒙古医学杂志, 2018, 50(9): 1045-1046, 1154. doi: 10.16096/J.cnki.nmgyxzz.2018.50.09.010
[2] Lee NK, Kim S, Hong SB, et al. CT diagnosis of non-traumatic gastrointestinal perforation: an emphasis on the causes[J]. Jpn J Radiol, 2020, 38(2): 101-111. doi: 10.1007/s11604-019-00910-7
[3] Shin D, Rahimi H, Haroon S, et al. Imaging of Gastrointestinal Tract Perforation[J]. Radiol Clin North Am, 2020, 58(1): 19-44. doi: 10.1016/j.rcl.2019.08.004
[4] Søreide K, Thorsen K, Søreide JA. Strategies to improve the outcome of emergency surgery for perforated peptic ulcer[J]. Br J Surg, 2013, 101(1): e51-e64. doi: 10.1002/bjs.9368
[5] Lo Re G, Mantia FL, Picone D, et al. Small bowel perforations: what the radiologist needs to know[J]. Semin Ultrasound CT MR, 2016, 37(1): 23-30. doi: 10.1053/j.sult.2015.11.001
[6] Tan KK, Bang SL, Sim R. Surgery for small bowel perforation in an Asian population: predictors of morbidity and mortality[J]. J Gastrointest Surg, 2010, 14(3): 493-499. doi: 10.1007/s11605-009-1097-y
[7] 潘传鹏, 余应喜, 徐昉. 消化道穿孔所致复杂腹腔感染的ICU诊治研究进展[J]. 中国急救医学, 2021, 41(2): 176-181. doi: 10.3969/j.issn.1002-1949.2021.02.017
[8] Lee DB, Shin S, Yang CS. Patient outcomes and prognostic factors associated with colonic perforation surgery: a retrospective study[J]. J Yeungnam Med Sci, 2022, 39(2): 133-140. doi: 10.12701/yujm.2021.01445
[9] Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D. Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality[J]. World J Surg, 2009, 33(1): 80-85. doi: 10.1007/s00268-008-9796-1
[10] Boey J, Choi SK, Poon A, et al. Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors[J]. Ann Surg, 1987, 205(1): 22-26. doi: 10.1097/00000658-198701000-00005
[11] Møller MH, Engebjerg MC, Adamsen S, et al. The Peptic Ulcer Perforation(PULP)score: a predictor of mortality following peptic ulcer perforation. A cohort study[J]. Acta Anaesthesiol Scand, 2012, 56(5): 655-662. doi: 10.1111/j.1399-6576.2011.02609.x
[12] Linder MM, Wacha H, Feldmann U, et al. The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis[J]. Chirurg, 1987, 58(2): 84-92.
[13] Thomas M, George NA, Gowri BP, et al. Comparative evaluation of ASA classification and ACE-27 index as morbidity scoring systems in oncosurgeries[J]. Indian J Anaesth, 2010, 54(3): 219-225. doi: 10.4103/0019-5049.65366
[14] Konishi T, Goto T, Fujiogi M, et al. New machine learning scoring system for predicting postoperative mortality in gastroduodenal ulcer perforation: a study using a Japanese nationwide inpatient database[J]. Surgery, 2022, 171(4): 1036-1042. doi: 10.1016/j.surg.2021.08.031
[15] Wu JZ, Shu P, He HY, et al. Predictors of mortality in patients with acute small-bowel perforation transferred to ICU after emergency surgery: a single-centre retrospective cohort study[J]. Gastroenterol Rep(Oxf), 2022, 10: goab054.
[16] Shin R, Lee SM, Sohn B, et al. Predictors of morbidity and mortality after surgery for intestinal perforation[J]. Ann Coloproctol, 2016, 32(6): 221-227. doi: 10.3393/ac.2016.32.6.221
[17] 王春艳. 以监测NT-proBNP为指导的临床用药对慢性心力衰竭病人住院率及心血管死亡率的影响[J]. 中西医结合心脑血管病杂志, 2021, 19(10): 1700-1702. doi: 10.12102/j.issn.1672-1349.2021.10.025
[18] 郭志强. 消化道恶性肿瘤200例临床分析[J]. 基层医学论坛, 2017, 21(23): 3158-3159. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLT201723096.htm
-




 下载:
下载: