Prognostic value of early heparin binding protein combined with procalcitonin in patients with severe pneumonia
-
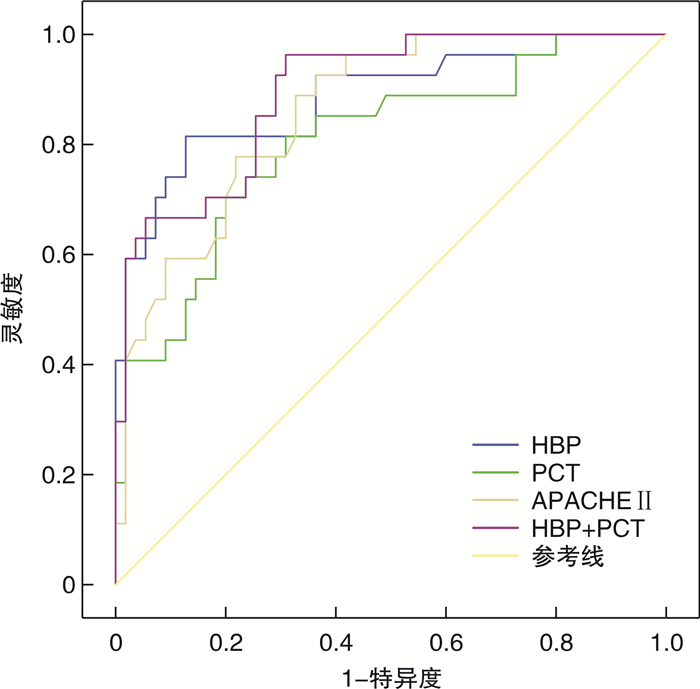
摘要: 目的 探讨早期肝素结合蛋白(HBP)水平联合降钙素原(PCT)对重症肺炎患者死亡预后的预测价值。方法 回顾性纳入我院ICU重症肺炎患者82例,根据患者28 d生存情况分为生存组和死亡组,统计两组患者基线资料情况,并比较两组患者入院24 h内血清HBP、PCT水平以及与临床预后的相关性。结果 死亡组患者的APACHEⅡ评分、PCT水平、HBP水平明显高于生存组(P< 0.05),单因素及多因素logistic回归分析示HBP、PCT、APACHEⅡ评分是重症肺炎患者发生死亡的独立风险因素(P< 0.05),相关性分析示早期HBP水平与PCT呈正相关(r=0.839,P< 0.05),HBP、PCT水平均与APACHEⅡ评分呈正相关(r=0.763,P< 0.05;r=0.797,P< 0.05)。进一步ROC曲线分析示HBP联合PCT对重症肺炎患者的预后具有较高的评估价值(AUC=0.896,P< 0.05)。结论 早期HBP水平联合PCT对重症肺炎患者具有较好的病情严重程度评估意义及死亡预后预测价值。Abstract: Objective To investigate the prognostic value of early heparin binding protein(HBP)level combined with procalcitonin(PCT)in patients with severe pneumonia.Methods A total of 82 ICU patients with severe pneumonia were retrospectively analyzed and divided into the survival group and the death group according to the 28-day survival. The baseline data of the two groups were statistically analyzed, and the serum levels of HBP and PCT within 24 hours of admission were compared between the two groups as well as their correlation with clinical prognosis.Results APACHEⅡ score, PCT level and HBP level in the death group were significantly higher than those in the survival group (P< 0.05). Logistic regression analysis showed that HBP, PCT and APACHEⅡ score were independent risk factors for death in patients with severe pneumonia (P< 0.05). Early HBP level was positively correlated with PCT (r=0.839,P< 0.05). Both HBP and PCT levels were positively correlated with APACHEⅡ score (r=0.763,P< 0.05;r=0.797,P< 0.05). ROC curve analysis further showed that HBP combined with PCT had a higher predicting value for the prognosis of death in severe pneumonia patients (AUC=0.896,P< 0.05).Conclusion The combination of HBP and PCT in early stage of severe pneumonia has a good value in evaluating the severity of the disease and predicting the prognosis of death.
-
Key words:
- severe pneumonia /
- heparin binding protein /
- procalcitonin /
- prognosis
-

-
表 1 两组患者基线资料比较
例(%), X±S 基线资料 生存组 死亡组 t/χ2 P 例数 55 27 年龄/岁 59.38±6.81 63.17±7.14 2.38 0.023 性别 3.138 0.076 男 30(54.55) 15(55.56) 女 25(45.45) 12(44.44) 吸烟史 10(18.18) 5(18.52) 2.487 0.115 BMI 24.45±5.24 23.39±4.12 1.465 0.144 APACHEⅡ评分/分 19.35±3.28 25.43±4.25 2.576 0.015 基础疾病 糖尿病 9(16.36) 5(18.52) 2.52 0.112 高血压 12(21.82) 6(22.22) 3.42 0.065 冠心病 7(12.73) 4(14.81) 3.09 0.078 脑梗死 6(10.91) 4(14.81) 2.04 0.150 肺部感染类型 细菌性肺炎 42(76.36) 20(74.07) 1.785 0.182 病毒性肺炎 4(7.27) 2(7.41) 2.950 0.086 真菌性肺炎 6(10.91) 3(11.11) 2.764 0.096 其他 3(5.45) 2(7.41) 3.096 0.078 谷丙转氨酶/(U·L-1) 53.25±12.35 58.37±17.48 1.187 0.243 谷草转氨酶/(U·L-1) 60.78±13.45 62.59±15.21 1.677 0.103 肌酐/(μmol·L-1) 95.46±23.17 99.34±25.26 1.765 0.093 尿素氮/(mmol·L-1) 19.46±4.89 20.76±5.24 1.872 0.068 PCT/(ng·mL-1) 15.61±6.50 26.56±9.76 2.184 0.036 CRP/(mg·L-1) 113.67±78.90 147.68±82.95 2.145 0.033 HBP/(ng·mL-1) 13.45±3.46 24.58±4.75 2.374 0.026 氧合指数/mmHg 218.25±60.57 175.85±57.80 3.089 0.002 表 2 单因素logistic回归分析
变量 P OR 95%CI 年龄 0.004 1.025 1.034~1.245 性别 0.087 0.789 0.987~1.348 HBP < 0.001 1.305 1.156~1.472 PCT < 0.001 1.228 1.110~1.359 CRP 0.056 1.057 0.789~1.892 APACHEⅡ < 0.001 1.269 1.135~1.420 氧合指数 < 0.001 6.675 1.115~24.678 表 3 多因素logistic回归分析
变量 P OR 95%CI 年龄 0.098 1.012 0.789~1.123 HBP 0.043 1.156 1.004~1.731 PCT 0.045 1.018 0.884~1.172 APACHEⅡ 0.016 1.171 1.030~1.331 氧合指数 < 0.001 4.567 2.356~18.679 -
[1] Huang J, Guo J, Li H, et al. Efficacy and safety of adjunctive corticosteroids therapy for patients with severe community-acquired pneumonia: A systematic review and meta-analysis[J]. Medicine(Baltimore), 2019, 98(13): e14636.
[2] 吕颖, 张一杰, 吴珺, 等. 重症肺炎病原菌耐药性及T细胞亚群变化[J]. 中华医院感染学杂志, 2020, 30(20): 3085-3089. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY202020012.htm
[3] 陈美芳, 陈春玲, 叶灵燕, 等. 降钙素原变化率在重症肺炎中的诊断价值[J]. 中华医院感染学杂志, 2019, 29(7): 993-996. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201907008.htm
[4] 中国医师协会急诊医师分会, 中国急性感染联盟. 2015年中国急诊社区获得性肺炎临床实践指南[J]. 中华急诊医学杂志, 2015, 24(12): 1324-1344. doi: 10.3760/cma.j.issn.1671-0282.2015.12.004
[5] Sun JR, Wang HH, Zong LZ, et al. Ventilator for the management of patients with severe pneumonia: A protocol of systematic review[J]. Medicine(Baltimore), 2020, 99(41): e22386.
[6] 鲁辛辛, 吴丽媛, 李雪, 等. 宿主生物标志物在社区获得性肺炎诊断、治疗和预后中的作用[J]. 临床检验杂志, 2019, 37(7): 481-485. https://www.cnki.com.cn/Article/CJFDTOTAL-LCJY201907001.htm
[7] Chalupa P, Beran O, Herwald H, et al. Evaluation of potential biomarkers for the discrimination of bacterial and viral infections[J]. Infection, 2011, 39(5): 411-417. doi: 10.1007/s15010-011-0126-4
[8] Bentzer P, Fisher J, Kong HJ, et al. Heparin-binding protein is important for vascular leak in sepsis[J]. Intensive Care Med Exp, 2016, 4(1): 33. doi: 10.1186/s40635-016-0104-3
[9] Cheng Z, Yang YJ, Jing XG, et al. Diagnostic value of HBP, PCT combined with APACHEⅡ score respectively in ventilator-associated pneumonia[J]. Zhonghua Yi Xue Za Zhi, 2019, 99(22): 1698-1702.
[10] Paulsson M, Thelaus L, Riesbeck K, et al. Heparin-binding protein in lower airway samples as a biomarker for pneumonia[J]. Respir Res, 2021, 22(1): 174. doi: 10.1186/s12931-021-01764-2
[11] Elsayed M, El-Wakel SA, Hamid MA, et al. Heparin Binding Protein as a Predictive Marker for Sepsis and Septic Shock in Critically Ill Patients: A Cross Sectional Study[J]. Egyptian J Hospital Med, 2021, 83(1): 1290-1296. doi: 10.21608/ejhm.2021.165497
[12] Havelka A, Sejersen K, Venge P, et al. Calprotectin, a new biomarker for diagnosis of acute respiratory infections[J]. Sci Rep, 2020, 10(1): 4208. doi: 10.1038/s41598-020-61094-z
[13] Cai R, Li H, Tao Z. Heparin-binding protein and procalcitonin in the diagnosis of pathogens causing community-acquired pneumonia in adult patients: a retrospective study[J]. Peer J, 2021, 9: e11056. doi: 10.7717/peerj.11056
[14] Komiya K, Yamamoto T, Yoshikawa H, et al. Factors associated with gravity-dependent distribution on chest CT in elderly patients with community-acquired pneumonia: a retrospective observational study[J]. Sci Rep, 2022, 12(1): 8023. doi: 10.1038/s41598-022-12092-w
[15] Ferrer M, Travierso C, Cilloniz C, et al. Severe community-acquired pneumonia: Characteristics and prognostic factors in ventilated and non-ventilated patients[J]. PLoS One, 2018, 13(1): e0191721. doi: 10.1371/journal.pone.0191721
[16] Zhong Y, Yu Z, Wang L, et al. Combined detection of procalcitonin, heparin-binding protein, and interleukin-6 is a promising assay to diagnose and predict acute pancreatitis[J]. J Clin Lab Anal, 2021, 35(8): e23869.
[17] Kjölvmark C, Akesson P, Linder A. Elevated urine levels of heparin-binding protein in children with urinary tract infection[J]. Pediatr Nephrol, 2012, 27(8): 1301-1308. doi: 10.1007/s00467-012-2132-x
[18] Kjölvmark C, Tschernij E, Öberg J, et al. Distinguishing asymptomatic bacteriuria from urinary tract infection in the elderly-the use of urine levels of heparin-binding protein and interleukin-6[J]. Diagn Microbiol Infect Dis, 2016, 85(2): 243-248. doi: 10.1016/j.diagmicrobio.2016.03.005
[19] Fisher J, Russell JA, Bentzer P, et al. Heparin-Binding Protein(HBP): A Causative Marker and Potential Target for Heparin Treatment of Human Sepsis-Induced Acute Kidney Injury[J]. Shock, 2017, 48(3): 313-320. doi: 10.1097/SHK.0000000000000862
-




 下载:
下载: