Study on the relationship between dynamic change of end-tidal carbon dioxide concentration in the expired air and neurological prognosis in cardiopulmonary resuscitation patients treated with therapeutic hypothermia
-
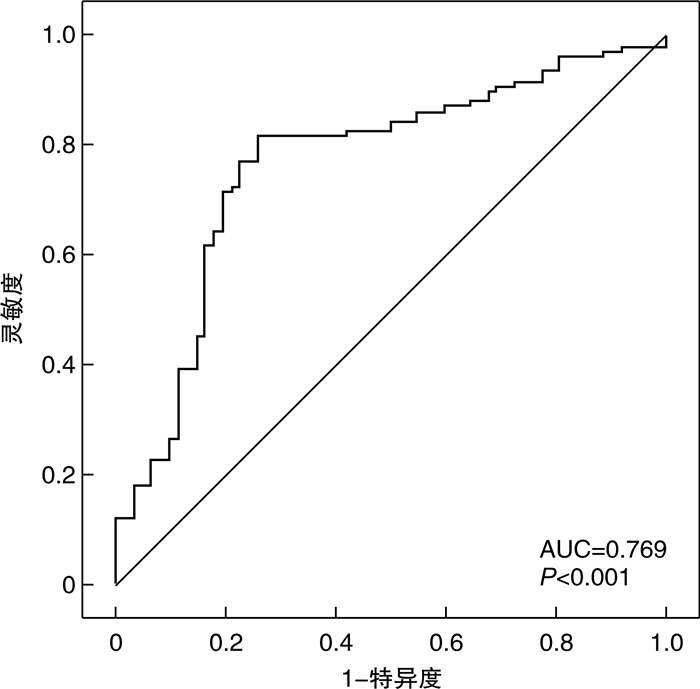
摘要: 目的 探讨呼气末二氧化碳(ETCO2)动态变化与接受亚低温治疗(TH)的心肺复苏患者神经预后的关系。方法 回顾性选择2020年1月—2022年1月我院收治的172例接受TH的心肺复苏患者,根据格拉斯哥昏迷量表(GCS)评分分为轻型昏迷组(6~7分,47例)、中型昏迷组(4~5分,79例)和重型昏迷组(≤3分,46例),根据格拉斯哥-匹兹堡脑功能表现分级(CPC)评分分为神经预后良好组(1~2级,62例),神经预后不良组(3~5级,110例)。分别于TH治疗前(T0)、治疗12 h(T1)、治疗24 h(T2)监测ETCO2,通过多因素logistic回归分析影响TH心肺复苏患者神经预后的因素,受试者工作特征曲线(ROC)分析ETCO2预测TH心肺复苏患者神经预后的价值。结果 TH治疗后ETCO2逐渐增加(P< 0.01),重型昏迷组T1、T2时ETCO2低于中型昏迷组和轻型昏迷组(P< 0.05),神经预后不良组T1、T2时ETCO2低于神经预后良好组(P< 0.01)。恢复自主循环时间、重型昏迷是TH心肺复苏患者神经预后不良的危险因素(P< 0.01),T2 ETCO2是保护因素(P< 0.01)。T2 ETCO2预测TH心肺复苏患者神经预后不良的曲线下面积为0.769(95%CI:0.698~0.829),灵敏度为77.27%,特异度为77.42%。结论 低ETCO2与TH心肺复苏患者昏迷程度加重以及神经预后不良有关,可作为预测神经预后的指标。Abstract: Objective To investigate the relationship between dynamic change of end-tidal carbon dioxide concentration in the expired air(ETCO2) and neurological prognosis in patients undergoing therapeutic hypothermia(TH) during cardiopulmonary resuscitation(CPR).Methods One hundred and seventy-two patients with cardiopulmonary resuscitation patients who received TH and admitted to our hospital from January 2020 to January 2022 were retrospectively selected. According to the Glasgow coma scale(GCS) score these patients were divided into light coma group(6 to 7 points, 47 cases), medium coma group(4 to 5 points, 79 cases), heavy coma group(≤3 points, 46 cases), according to the Glasgow-Pittsburgh brain function performance classification(CPC) score they were divided into neural good prognosis groups(grade 1 to 2, 62 cases), poor neurological prognosis group(grade 3 to 5, 110 cases). ETCO2 was monitored before treatment(T0), 12 h(T1) and 24 h(T2) after TH in patients with TH CPR. Multivariate logistic regression was used to analyze the factors affecting the neurological prognosis of patients with TH CPR, and receiver operating characteristic curve(ROC) was used to analyze the value of ETCO2 in predicting the neurological prognosis of patients with TH CPR.Results After TH treatment, ETCO2 increased gradually(P< 0.01). The ETCO2 of severe coma group at T1 and T2 was lower than that of moderate coma group and mild coma group(P< 0.05). The ETCO2 of poor neurological prognosis group at T1 and T2 was lower than that of good neurological prognosis group(P< 0.01). Recovery time of spontaneous circulation and severe coma were risk factors for poor neurological prognosis in patients with TH CPR(P< 0.01), while T2 ETCO2 was protective factor(P< 0.01). The area under the curve for T2 ETCO2 to predict poor neurological prognosis in patients with cardiopulmonary resuscitation who received TH was 0.769(95%CI: 0.698-0.829), with a sensitivity of 77.27% and specificity of 77.42%.Conclusion Low ETCO2 is associated with worsening coma degree and poor neurological prognosis in patients with cardiopulmonary resuscitation who received TH, which can be used as a predictor of neurological prognosis.
-

-
表 1 不同昏迷程度患者ETCO2变化和差异
mmHg,X±S 组别 例数 T0 T1 T2 轻型昏迷组 47 10.35±3.26 23.15±6.35 30.12±7.95 中型昏迷组 79 10.02±3.191) 19.35±5.111) 23.65±6.471) 重型昏迷组 46 9.92±3.021)2) 13.02±4.181)2) 18.35±5.301)2) 注:1 mmHg=0.133 kPa。与轻型昏迷组比较,1)P < 0.05;与中型昏迷组比较,2)P < 0.05。 表 2 不同神经预后患者ETCO2变化和差异
mmHg,X±S 组别 例数 T0 T1 T2 神经预后良好组 62 10.16±3.09 20.15±5.39 27.34±7.19 神经预后不良组 110 10.04±3.16 17.88±4.03 22.18±4.06 t 0.241 3.131 6.021 P 0.810 < 0.01 < 0.01 表 3 影响TH心肺复苏患者神经预后的单因素分析结果
例(%),X±S,M(P25,P75) 组别 神经预后不良组(110例) 神经预后良好组(62例) t/z/χ2 P 年龄/岁 51.84±9.32 49.65±10.24 1.428 0.155 性别 0.556 0.456 男 65(59.09) 33(53.23) 女 45(40.91) 29(46.77) BMI 23.05±1.67 22.96±1.53 0.350 0.727 基础疾病 高血压 42(38.18) 25(40.32) 0.076 0.782 糖尿病 31(28.18) 14(22.58) 0.644 0.422 自主循环恢复时间/min 8.02±1.02 5.32±0.30 20.330 < 0.01 昏迷程度 13.518 < 0.01 轻型昏迷 20(18.18) 27(43.55) 中型昏迷 59(53.64) 20(32.26) 重型昏迷 31(28.18) 15(24.19) APACHE Ⅱ评分/分 22.02(15,29) 16.35(10,18) 11.378 < 0.01 机械通气时间/d 9.35(12,23) 15.21(9,20) 8.209 < 0.01 潮气量/mL 695.23±59.04 694.11±58.74 0.120 0.905 呼吸频率/(次·min-1) 13.02±0.68 12.98±0.71 0.365 0.716 PEEP/cmH2 O 4.13±0.63 4.17±0.59 0.409 0.683 氧浓度/% 37.65±8.13 37.09±8.04 0.435 0.664 EICU入住时间/d 22.11(15,28) 17.42(12,23) 15.284 < 0.01 LVEF/% 56.11±2.07 57.02±3.18 2.269 0.025 E/A比值 2.01±0.32 1.96±0.31 0.995 0.321 表 4 影响TH心肺复苏患者神经预后的logistic回归方程
因素 β SE Wald χ2 OR P 常数项 5.021 1.009 24.763 < 0.01 恢复自主循环时间 0.651 0.182 12.794 1.917 < 0.01 重型昏迷 0.759 0.201 14.259 2.136 < 0.01 T2 ETCO2 -0.517 0.153 11.418 0.596 < 0.01 -
[1] Sandroni C, D'Arrigo S, Cacciola S, et al. Prediction of poor neurological outcome in comatose survivors of cardiac arrest: a systematic review[J]. Intensive Care Med, 2020, 46(10): 1803-1851. doi: 10.1007/s00134-020-06198-w
[2] 许丽君, 崔英杰, 秦历杰. 心肺复苏后神经功能预后与早期平均动脉压的关系[J]. 中华急诊医学杂志, 2020, 29(5): 711-715. https://www.cnki.com.cn/Article/CJFDTOTAL-XNYB202103012.htm
[3] Taccone FS, Picetti E, Vincent JL. High Quality Targeted Temperature Management(TTM)After Cardiac Arrest[J]. Crit Care, 2020, 24(1): 6. doi: 10.1186/s13054-019-2721-1
[4] 王嘉宇, 杜贤进. 呼气末二氧化碳监测在血流动力学监测中的应用[J]. 临床急诊杂志, 2020, 21(12): 1009-1013. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202012019.htm
[5] Aminiahidashti H, Shafiee S, Zamani Kiasari A, et al. Applications of End-Tidal Carbon Dioxide(ETCO2) Monitoring in Emergency Department; a Narrative Review[J]. Emerg(Tehran), 2018, 6(1): e5.
[6] 张明, 钱俊英, 李涛, 等. 脑电双频指数在评估心肺复苏成功患者的昏迷程度和判定预后中的价值[J]. 中国急救医学, 2012, 32(1): 7-10.
[7] Sandroni C, Cariou A, Cavallaro F, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine[J]. Resuscitation, 2014, 85(12): 1779-1789. doi: 10.1016/j.resuscitation.2014.08.011
[8] Sandroni C, Cronberg T, Sekhon M. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis[J]. Intensive Care Med, 2021, 47(12): 1393-1414. doi: 10.1007/s00134-021-06548-2
[9] 罗成准, 王世伟, 贾天元, 等. 心肺复苏后患者中性粒细胞与淋巴细胞比值与死亡的相关性研究[J]. 临床急诊杂志, 2020, 21(2): 143-146. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202002010.htm
[10] Rossetti AO, Rabinstein AA, Oddo M. Neurological prognostication of outcome in patients in coma after cardiac arrest[J]. Lancet Neurol, 2016, 15(6): 597-609. doi: 10.1016/S1474-4422(16)00015-6
[11] 周建坡, 徐珑, 赵继宗. 神经电生理监测技术在昏迷患者预后评估中的应用进展[J]. 中华神经外科杂志, 2020, 36(4): 418-421.
[12] Uzunay H, Selvi F, Bedel C, et al. Comparison of ETCO2 Value and Blood Gas PCO2 Value of Patients Receiving Non-invasive Mechanical Ventilation Treatment in Emergency Department[J]. SN Compr Clin Med, 2021, 3(8): 1717-1721. doi: 10.1007/s42399-021-00935-y
[13] Nassar BS, Schmidt GA. Estimating Arterial Partial Pressure of Carbon Dioxide in Ventilated Patients: How Valid Are Surrogate Measures?[J]. Ann Am Thorac Soc, 2017, 14(6): 1005-1014. doi: 10.1513/AnnalsATS.201701-034FR
[14] Sazgar M, Golikhatir I, Pashaee SM, et al. Norepinephrine with dopamine infusion on the end-tidal carbon dioxide(EtCO2) pressure in patients with septic shock[J]. Caspian J Intern Med, 2021, 12(4): 580-585.
[15] Bulger N, Harrington B, Krieger J, et al. Prehospital end-tidal carbon dioxide predicts hemorrhagic shock upon emergency department arrival[J]. J Trauma Acute Care Surg, 2021, 91(3): 457-464. doi: 10.1097/TA.0000000000003312
[16] Baudel JL, Dubee V, Boelle PY, et al. The Weaning Index combining EtCO2 and respiratory rate early identifies Spontaneous Breathing Trial failure[J]. Minerva Anestesiol, 2019, 85(4): 384-392.
[17] Nicholson TC, Paiva EF. Uses and pitfalls of measurement of end-tidal carbon dioxide during cardiac arrest[J]. Curr Opin Crit Care, 2020, 26(6): 612-616. doi: 10.1097/MCC.0000000000000767
[18] Touma O, Davies M. The prognostic value of end tidal carbon dioxide during cardiac arrest: a systematic review[J]. Resuscitation, 2013, 84(11): 1470-1479. doi: 10.1016/j.resuscitation.2013.07.011
[19] Ölander CH, Vikholm P, Schiller P, et al. End-Tidal Carbon Dioxide Impacts Brain and Kidney Injury in Experimental Extracorporeal Cardiopulmonary Resuscitation(ECPR)[J]. Shock, 2021, 55(4): 563-569.
[20] Chandrasekharan PK, Rawat M, Nair J, et al. Continuous End-Tidal Carbon Dioxide Monitoring during Resuscitation of Asphyxiated Term Lambs[J]. Neonatology, 2016, 109(4): 265-273.
[21] Balakrishnan S, Naik S, Chakrabarti D, et al. Effect of Respiratory Physiological Changes on Optic Nerve Sheath Diameter and Cerebral Oxygen Saturation in Patients With Acute Traumatic Brain Injury[J]. J Neurosurg Anesthesiol, 2022, 34(1): e52-e56.
-




 下载:
下载: