Diagnostic value and prognostic effect of thromboelastometry on disseminated intravascular coagulation in patients with sepsis
-
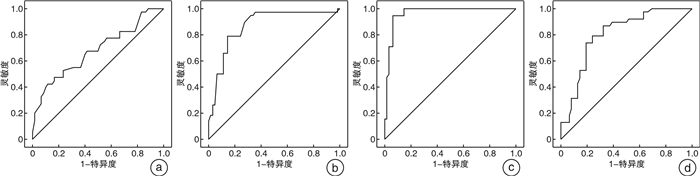
摘要: 目的 探讨血栓弹力图各参数对脓毒症患者弥散性血管内凝血(DIC)的诊断和排除价值及对其预后的影响。方法 收集2020年1月1日-2021年6月31日上海市浦东新区人民医院急诊与危重症医学科符合脓毒症3.0诊断标准且入院当天测过血栓弹力图的100例患者为研究对象,同时对入组患者进行中国DIC诊断积分系统(CDSS)积分,筛查出合并DIC的患者, 分为DIC组和非DIC组;记录患者90 d的生存状态,分为存活组与死亡组。运用受试者工作特征曲线(ROC)来评估血栓弹力图对脓毒症患者DIC的预测价值及对其预后的影响。结果 存活组(n=60例)和死亡组(n=40例)比较发现:死亡组血小板计数、白蛋白降低,而C反应蛋白、初始乳酸、序贯器官衰竭评分(SOFA)和急性生理学及慢性健康状况评分Ⅱ(APACHEⅡ)明显升高(P<0.05);凝血指标中凝血酶原时间、部分凝血活酶时间、国际标准化比率、D-二聚体、凝血反应时间(R)升高,但最大振幅(MA)降低(P<0.05);利用ROC曲线分析MA预测脓毒症患者90 d的生存率,发现曲线下面积为0.678(95%CI 0.569~0.788),诊断阈值为68.9,灵敏度为47.5%,特异度为83.3%。DIC组(n=38)与非DIC组(n=62)相比发现:DIC组R、血凝块形成时间(K)升高,血凝块形成速率(α角)及MA降低(P<0.05);ROC曲线分析发现R诊断DIC的曲线下面积为0.869(95%CI 0.794~0.943),诊断阈值为6.9,灵敏度为78.9%,特异度为88.5%;K诊断DIC的曲线下面积为0.965(95%CI 0.930~0.999),诊断阈值为3.5,灵敏度为94.7%,特异度为93.5%;排除DIC的MA曲线下面积为0.805(95%CI 0.719~0.890),诊断阈值为64.2,灵敏度为78.9%,特异度为75.8%;α角不能排除DIC诊断。结论 血栓弹力图参数可作为诊断及排除DIC的一种有效方法。MA值对预测脓毒症患者的病死率有参考价值。Abstract: Objective To analyze the effect of thromboelastography(TEG) parameters on the diagnosis and exclusion value and prognosis of disseminated intravascular coagulation(DIC) in patients with sepsis.Methods A total of 100 patients were collected from January 1, 2020 to June 31, 2021 in the Department of Critical Care Medicine of Shanghai Pudong New Area People's Hospital who met the criteria of sepsis 3.0 and had thromboelastography measured on the day of admission. At the same time, the enrolled patients were scored by the Chinese disseminated intravascular coagulation diagnostic scoring system(CDSS) to screen out patients with DIC who were recorded the 90-day survival status, in the meanwhile. Receiver operating curve(ROC) was used to evaluate the predictive value and prognostic impact of thromboelastometry on patients occurred DIC with sepsis.Results Compared with the survival group(n=60 cases) and the death group(n=40 cases), it was found that the platelet count and albumin in the death group were decreased, while the C-reactive protein, initial lactate, sequential organ failure assessment(SOFA) score and APACHE Ⅱ score were significantly increased(P < 0.05); in coagulation indexes, prothrombin time, partial thromboplastin time, international normalized ratio, D-dimer, coagulation reaction time(R) increased, but the maximum amplitude(MA) decreased(P < 0.05);using ROC curve analysis to predict the 90-day survival rate of patients with sepsis, the area under the curve was 0.678(95%CI 0.569-0.788), the diagnostic threshold was 68.9, the sensitivity was 47.5%, and the specificity was 83.3%. Compared with the non-DIC group(n=62) in the DIC group(n=38), it was found in that the DIC group the coagulation reaction time(R), the blood clot formation time(K), and the blood clot formation rate(α angle) were increased and the maximum amplitude(MA) was decreased(P < 0.05); ROC curve analysis found that the area under the curve of R to diagnose DIC was 0.869(95%CI 0.794-0.943), the diagnostic threshold was 6.9, the sensitivity was 78.9%, and the specificity was 88.5%;the area under the curve of K to diagnose DIC was 0.965(95%CI 0.930-0.999), the diagnostic threshold was 3.5, and the sensitivity was 94.7%, specificity 93.5%;area under the MA curve to exclude DIC was 0.805(95%CI 0.719-0.890), diagnostic threshold was 64.2, sensitivity was 78.9%, specificity was 75.8%; alpha angle could not exclude DIC diagnosis.Conclusion TEG parameters can be used as an effective method to diagnose and exclude DIC. The MA value has a reference value for predicting the mortality of sepsis patients.
-
Key words:
- sepsis /
- thromboelastography /
- disseminated intravascular coagulation /
- diagnosis /
- prognosis
-

-
表 1 CDSS积分标准
积分项 分数/分 存在导致DIC的原发病 2 临床表现 不能用原发病解释的严重或多发出血倾向 1 不能用原发病解释的微循环障碍或休克 1 广泛性皮肤、黏膜栓塞,灶性缺血性坏死、脱落及溃疡形成;不明原因的肺、肾、脑等脏器功能衰竭 1 实验室指标 血小板计数/(×109/L) 非恶性血液病 ≥100 0 80~<100 1 <80 2 24 h内下降≥50% 1 恶性血液病 <50 1 24 h内下降≥50% 1 D-二聚体/(mg·L-1) <5 0 5~<9 2 ≥9 3 PT及APTT延长 PT延长<3 s且APTT延长<10 s 0 PT延长3~<6 s或APTT延长≥10 s 1 PT延长≥6 s 2 纤维蛋白原/(g·L-1) ≥1.0 0 <1.0 1 注:非恶性血液病:每日积分1次,≥7分时可诊断为DIC;恶性血液病:临床表现第1项不参与评分,每日积分1次,≥6分时可诊断为DIC。 表 2 存活组与死亡组患者临床资料的比较
X±S,例,M(Q1,Q3) 临床资料 存活组(n=60) 死亡组(n=40) t/z P 年龄/岁 70.93±13.90 71.60±11.93 -0.248 0.804 性别 男 29 24 1.141 0.257 女 31 16 白细胞/(×109·L-1) 13.45±4.93 15.42±5.93 -1.801 0.075 血小板/(×109·L-1) 188.23±94.44 142.90±53.88 2.749 0.007 C反应蛋白/(mg·L-1) 69.22(22.94,122.97) 97.94(58.31,168.00) -2.213 0.027 血红蛋白/(g·L-1) 111.28±17.23 105.85±13.75 1.670 0.098 白蛋白/(g·L-1) 30.95±3.57 29.31±2.92 2.424 0.017 乳酸/(mmol·L-1) 5.28±2.93 7.77±2.63 -4.331 <0.001 SOFA评分/分 5.60±1.90 9.95±2.15 -8.441 <0.001 APACHEⅡ评分/分 17.15±7.02 28.80±6.97 -8.150 <0.001 表 3 DIC组与非DIC组患者临床资料的比较
X±S,例,M(Q1,Q3) 临床资料 DIC组(n=38) 非DIC组(n=62) t/z P 年龄/岁 72.50±12.08 70.40±13.71 0.776 0.440 性别 男 19 34 0.466 0.642 女 19 28 白细胞/(×109·L-1) 13.57±4.86 14.65±5.73 -0.963 0.338 血小板/(×109·L-1) 128.63±60.89 195.52±85.53 -4.208 <0.001 C反应蛋白/(mg·L-1) 79.30(29.71,168.00) 83.95(43.13,127.77) -0.245 0.806 血红蛋白/(g·L-1) 104.34±13.97 112.03±16.69 -2.375 0.020 白蛋白/(g·L-1) 29.32±2.86 30.89±3.59 -2.292 0.024 乳酸/(mmol·L-1) 8.28±3.11 5.04±2.29 5.982 <0.001 SOFA评分/分 8.97±2.69 7.21±2.35 3.445 0.001 APACHEⅡ评分/分 28.11±8.08 17.95±7.26 6.546 <0.001 表 4 各组的原发感染部位分布
例 感染部位 例数 存活组(n=60) 死亡组(n=40) DIC组(n=38) 非DIC组(n=62) 呼吸道感染 53 31 22 20 33 胃肠道感染 20 11 9 8 12 胆系感染 11 8 3 4 7 泌尿系感染 10 6 4 3 7 其他感染 6 4 2 3 3 表 5 存活组和死亡组凝血指标的比较
X±S,M(Q1,Q3) 凝血指标 存活组(n=60) 死亡组(n=40) t/z P PT/s 13.91±2.55 16.14±2.47 -4.348 <0.001 APTT/s 36.71±6.66 41.77±10.39 -2.972 0.004 INR 1.15±0.21 1.33±0.22 -4.071 <0.001 纤维蛋白原/(g·L-1) 4.25±1.47 4.65±1.84 -1.198 0.234 D-二聚体/(mg·L-1) 3.70(2.24,12.92) 13.06(6.30,25.38) -2.660 0.008 R/min 6.11±1.81 7.58±2.66 -3.278 0.001 K/min 3.11±1.86 3.49±1.84 -0.985 0.326 α/deg 59.60±7.13 57.30±11.08 1.263 0.210 MA/mm 65.74±6.28 59.47±10.12 3.829 <0.001 表 6 DIC组与非DIC组凝血指标的比较
X±S,M(Q1,Q3) 凝血指标 DIC组(n=38) 非DIC组(n=62) t/z P PT/s 16.43±1.42 13.80±2.87 5.262 <0.001 APTT/s 43.12±9.63 36.04±6.82 4.298 <0.001 INR 1.40±0.14 1.12±0.20 7.631 <0.001 纤维蛋白原/(g·L-1) 4.08±1.55 4.62±1.66 -1.600 0.113 D-二聚体/(mg·L-1) 12.92(3.71,22.58) 4.95(2.55,13.45) 2.738 0.006 R/min 8.45±2.11 5.63±1.67 7.416 <0.001 K/min 5.20±1.08 2.08±1.04 14.384 <0.001 α/deg 55.94±8.48 60.35±8.86 -2.457 0.016 MA/mm 57.99±9.70 66.45±5.87 -5.440 <0.001 -
[1] Font MD, Thyagarajan B, Khanna AK. Sepsis and Septic Shock-Basics of diagnosis, pathophysiology and clinical decision making[J]. Med Clin North Am, 2020, 104(4): 573-585. doi: 10.1016/j.mcna.2020.02.011
[2] Iba T, Levy JH. Sepsis-induced Coagulopathy and Disseminated Intravascular Coagulation[J]. Anesthesiology, 2020, 132(5): 1238-1245. doi: 10.1097/ALN.0000000000003122
[3] Delabranche X, Helms J, Meziani B. Immunohaemostasis: a new view on haemostasis during sepsis[J]. Ann Intensive Care, 2017, 7(1): 117. doi: 10.1186/s13613-017-0339-5
[4] Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(20): 2237.
[5] Abe T, Kubo K, Izumoto S, et al. Complement Activation in Human Sepsis is Related to Sepsis-Induced Disseminated Intravascular Coagulation[J]. Shock, 2020, 54(2): 198-204. doi: 10.1097/SHK.0000000000001504
[6] 张涛, 万亚楠, 王逸平, 等. 脓毒症患者DIC预警系统构建与临床研究[J]. 临床急诊杂志, 2021, 22(8): 513-520. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=3df26ce4-7d3f-4dc0-847e-a7e555ecfb1c
[7] Yamakawa K, Umemura Y, Murao S, et al. Optimal Timing and Early Intervention With Anticoagulant Therapy for Sepsis-Induced Disseminated Intravascular Coagulation[J]. Clin Applied Thrombosis/Hemostasis, 2019, 25: 1076029619835055.
[8] Iba T, Levi M, Levy JH. Sepsis-Induced Coagulopathy and Disseminated Intravascular Coagulation[J]. Semin Thromb Hemost, 2020, 46(1): 89-95. doi: 10.1055/s-0039-1694995
[9] Reikvam H, Steien E, Hauge B, et al. Thrombelastography[J]. Transfus Apher Sci, 2009, 40(2): 119-123. doi: 10.1016/j.transci.2009.01.019
[10] Ostrowski SR, Windelov NA, Ibsen M, et al. Consecutive thrombelastography clot strength profiles in patients with severe sepsis and their association with 28-day mortality: a prospective study[J]. J Crit Care, 2013, 28(3): 3-11.
[11] Haase N, Ostrowski SR, Wetterslev J, et al. Thromboelastography in patients with severe sepsis: A prospective cohort study[J]. Intens Care Med, 2015, 41: 77-85. doi: 10.1007/s00134-014-3552-9
[12] Koami H, Sakamoto Y, Ohta M, et al. Can rotational thromboelastometry predict septic disseminated intravascular coagulation? Blood Coagul[J]. Fibrinol, 2015, 26: 778-783.
[13] Luo C, Hu H, Gong J, et al. The Value of Thromboelastography in the Diagnosis of Sepsis-Induced Coagulopathy[J]. Clin Appl Thromb Hemost, 2020, 26: 1076029620951847.
[14] Kim MK, Kim SI, Yu G, et al. Role of Thromboelastography as an Early Predictor of Disseminated Intravascular Coagulation in Patients with Septic Shock[J]. J Clin Med, 2020, 9(12): 3883. doi: 10.3390/jcm9123883
[15] 中华医学会血液学分会血栓与止血学组. 弥散性血管内凝血诊断中国专家共(2017年版)[J]. 中国血液病杂志, 2017, 38(5): 361-363.
[16] Zhi DY, Lin J, Zhuang HZ, et al. Acute Kidney Injury in Critically Ill Patients with Sepsis: Clinical Characteristics and Outcomes[J]. J Investig Surg, 2020, 32(8): 689-696.
[17] Ramos-Rossy J, Otero-Domínguez Y, Axtmayer J, et al. An Unexpected Cause of Sepsis: Keep Pursuing the Source of Infection[J]. P R Health Sci J, 2019, 38(2): 118-119.
[18] Iba T, Arakawa M, Di Nisio M, et al. Newly Proposed Sepsis-Induced Coagulopathy Precedes International Society on Thrombosis and Haemostasis Overt-Disseminated Intravascular Coagulation and Predicts High Mortality[J]. J Intensive Care Med, 2020, 35(7): 643-649. doi: 10.1177/0885066618773679
[19] Haase N, Ostrowski SR, Wetterslev J, et al. Thromboelastography in patients with severe sepsis: a prospective cohort study[J]. Intensive Care Med, 2015, 41(1): 77-85. doi: 10.1007/s00134-014-3552-9
[20] Zheng R, Pan H, Wang JF, et al. The association of coagulation indicators with in-hospital mortality and 1-year mortality of patients with sepsis at ICU admissions: a retrospective cohort study[J]. Int J Clin Chem, 2020, 504: 109-118.
[21] Van der Meijden PEJ, Heemskerk JWM. Platelet biology and functions: new concepts and clinical perspectives[J]. Nat Rev Cardiol, 2019, 16(3): 166-179. doi: 10.1038/s41569-018-0110-0
[22] Pigozzi L, Aron JP, Ball J, et al. Understanding platelet dysfunction in sepsis[J]. Int Care Med, 2016, 42(4): 583-586. doi: 10.1007/s00134-015-4012-x
[23] Sivula M, Pettila V, Niemi TT, et al. Thromboelastometry in patients with severe sepsis and disseminated intravascular coagulation[J]. Blood Coagul Fibrinolysis, 2009, 20(6): 419-426. doi: 10.1097/MBC.0b013e32832a76e1
[24] Xue L, Sun QM, Yu H, et al. Relationship between Cellular Immunity Changes and Prognosis in Elderly Patients with Sepsis[J]. J Coll Physicians Surg Pak, 2019, 29(12): 1144-1148. doi: 10.29271/jcpsp.2019.12.1144
-




 下载:
下载: