Comparison of the therapeutic effect of continuous veno-venous hemofiltration versus continuous veno-venous hemodiafiltration in patients with acute kidney injury
-
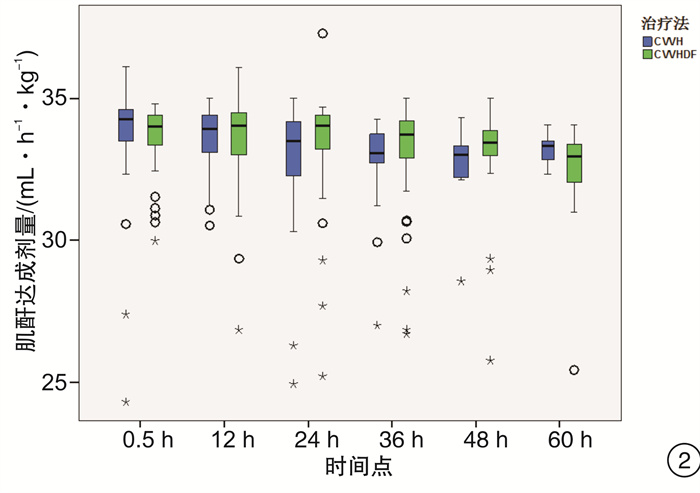
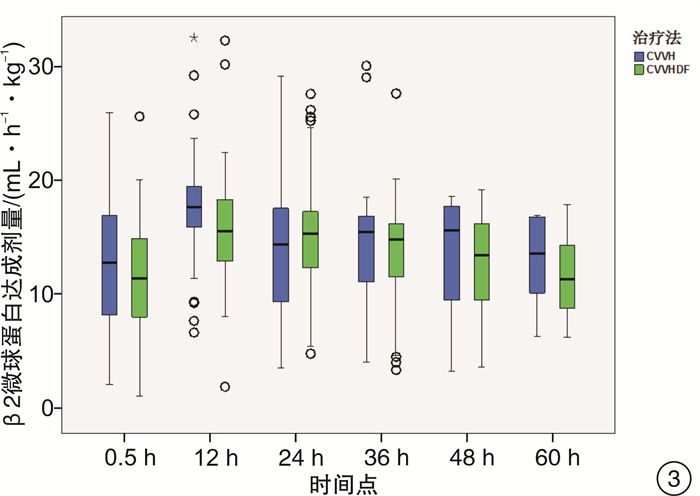
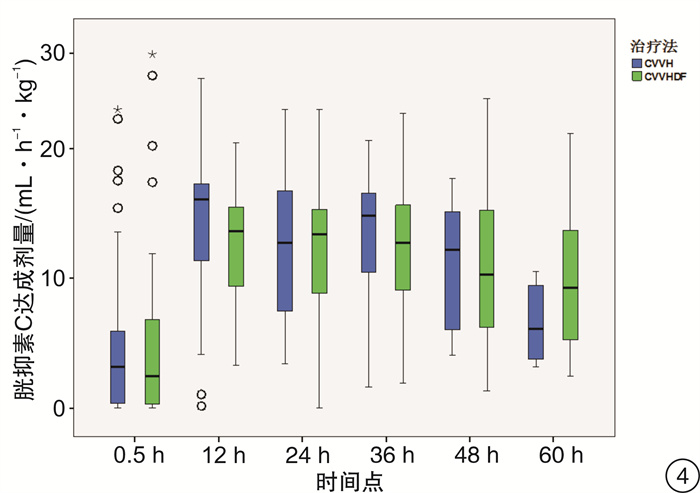
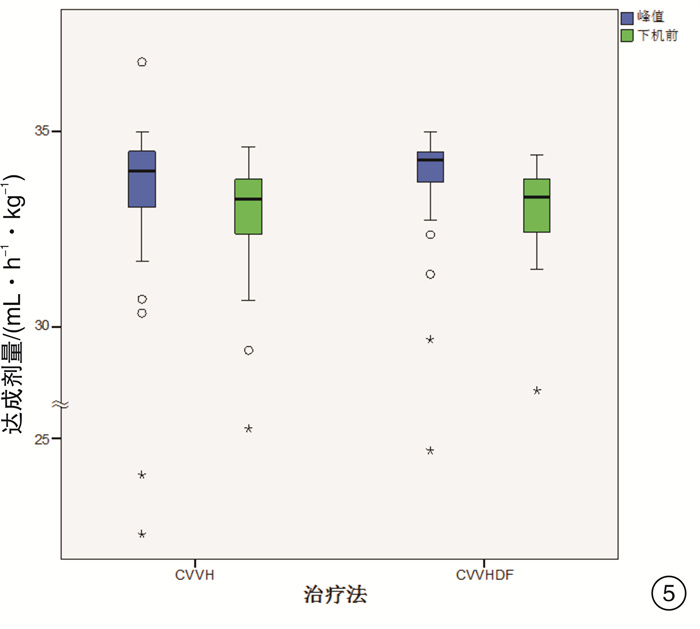
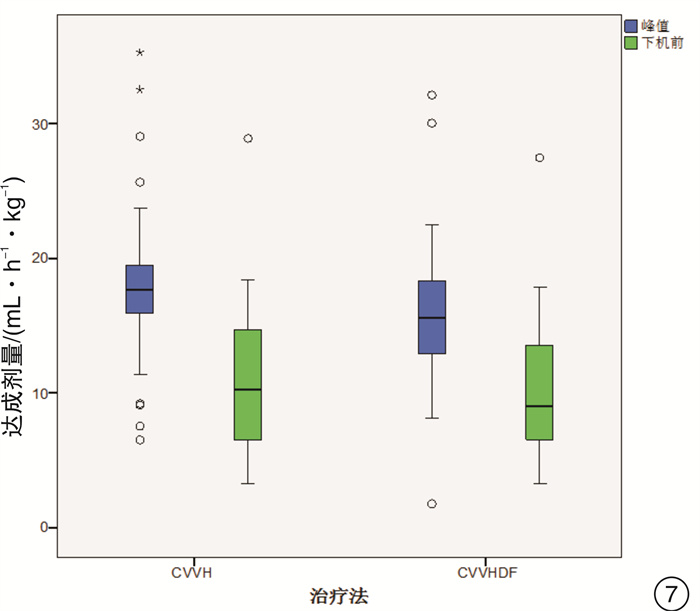
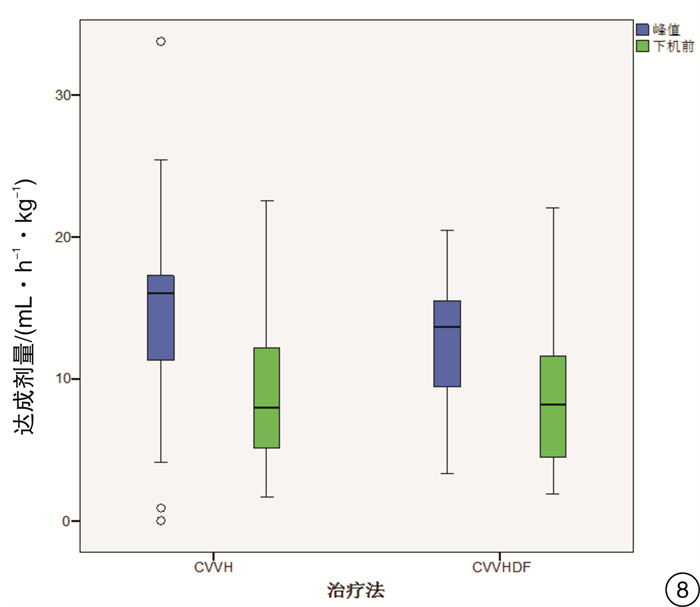
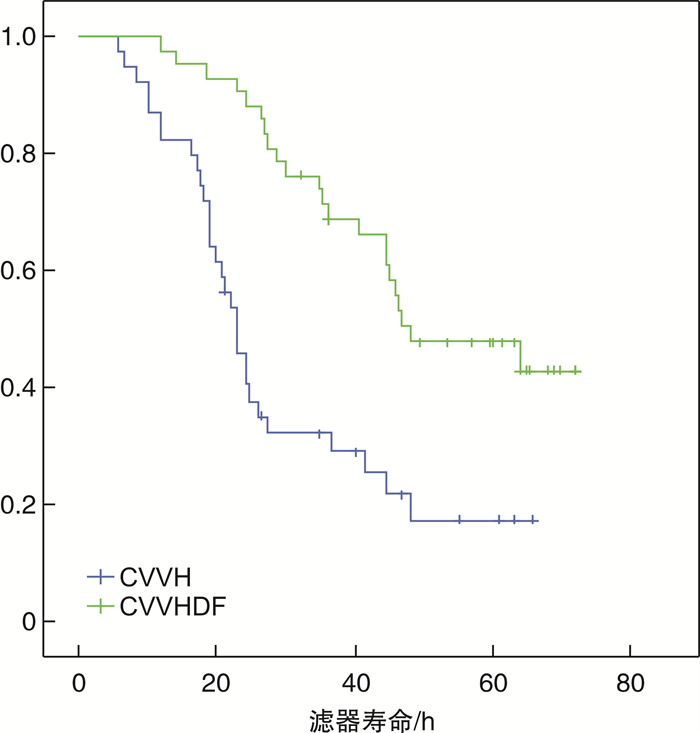
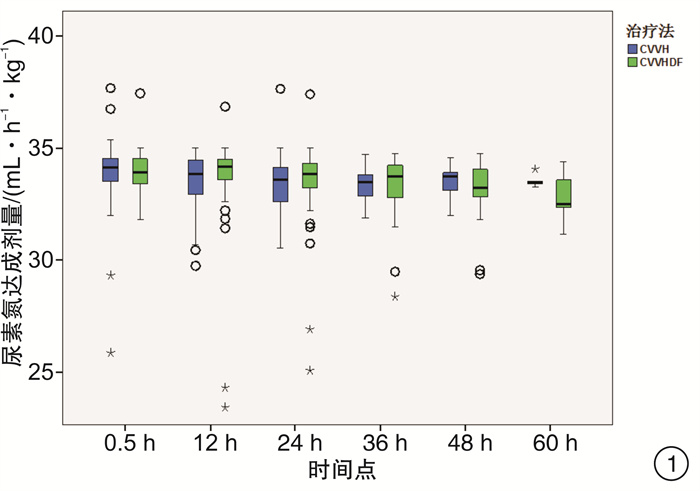
摘要: 目的 通过比较连续静-静脉血液滤过(CVVH)与连续静-静脉血液透析滤过(CVVHDF)治疗模式的溶质清除效率、滤器寿命,为临床决策中合理选择连续性肾脏替代治疗(CRRT)治疗模式提供依据。方法 选取2017年7月-2018年12月期间入住ICU需要行CRRT治疗的急性肾损伤患者,随机分组,通过交叉的研究设计,使用相同的处方剂量,分别先行CVVH或CVVHDF治疗,后行CVVHDF或CVVH治疗。比较两种治疗模式在不同时间点(治疗开始后0.5 h,每12 h及下机前),不同分子量溶质(尿素氮、肌酐、β2微球蛋白、胱抑素C)的达成剂量。最后比较两种模式的滤器寿命的差异。结果 CVVH与CVVHDF治疗模式对于小分子溶质的清除效率在各个时间点上均差异无统计学意义(P>0.05)。对于中分子溶质,CVVH模式的溶质清除效率优于CVVHDF模式,但仅出现在治疗的12 h时间点(P < 0.05)。CVVH治疗模式与CVVHDF模式对于不同分子量溶质的达成剂量在下机前均较前有明显的下降(P < 0.01)。CVVHDF模式的滤器寿命显著长于CVVH模式(P < 0.01)。结论 CVVH模式与CVVHDF模式对小分子溶质的清除率相近。CVVH对中分子溶质的清除率优势仅出现在治疗后的12 h。而CVVHDF滤器寿命更长,CVVHDF模式是更经济的选择。Abstract: Objective To provide a basis for rational selection of continuous renal replacement therapy (CRRT) treatment modality in clinical decision-making by comparing the solute removal efficiency and filter life of continuous veno-venous hemofiltration (CVVH) and continuous veno-venous hemodiafiltration (CVVHDF).Methods Patients with acute renal injury who were admitted to ICU and required CRRT were randomly assigned to receive either CVVH or CVVHDF treatment first followed by CVVHDF or CVVH treatment using the same prescribed dose in a crossover study design. The solute clearance efficiency was calculated with the delivered dose of different molecular weight solute (urea nitrogen, creatinine, β2 microglobulin and cystatin C) at various time points (0.5 h after treatment, every 12 h and before treatment ceased). The difference between delivered doses of CVVH and CVVHDF were then compared, as well as the filter life span of the two modalities.Results There was no significant difference between CVVH and CVVHDF treatment mode in the clearance efficiency of small molecule solute (urea nitrogen and creatinine) at each time point (P> 0.05). For medium molecular solutes (β2 microglobulin and cystatin C), the solute clearance efficiency of CVVH was superior than that of CVVHDF, but only exist at the 12h time point (P < 0.05). The delivered doses of CVVH and CVVHDF for different molecular weight solutes all decreased significantly before the circuit change (P < 0.01). The filter life of the CVVHDF was significantly longer than that of the CVVH (P < 0.01).Conclusion The CVVH mode and CVVHDF mode have similar clearance efficiency for small molecule solutes. The advantage of CVVH for medium molecular solutes clearance only occurs at 12h after treatment initiation. The CVVHDF filter has a longer life and CVVHDF is a more economical choice.
-

-
表 1 两组患者治疗前各项临床指标例(%),x±S
临床指标 A组(27例) B组(23例) χ2/Z/t P 性别 男 18(66.7) 16(69.6) χ2=0.118 0.732 女 9(33.3) 7(30.4) χ2=0.250 0.617 年龄/岁 62(38~79) 61(44~66) Z=-0.681 0.496 身高/cm 167±8 169±9 t=-0.870 0.388 体重/kg 70(60~75) 70(57~75) Z=-0.283 0.777 ApacheⅡ评分/分 19(13~23) 17(13~20) Z=-0.946 0.344 SOFA评分/分 13(9~16) 11(8~17) Z=-0.078 0.938 主要诊断 感染性休克 17(63.0) 9(39.1) χ2=2.462 0.117 其他脏器功能不全 1(3.7) 5(21.7) χ2=2.667 0.102 药物或毒物 6(22.2) 2(8.7) χ2=2.000 0.157 呼吸心搏骤停 2(7.4) 3(13.0) χ2=0.200 0.655 未找到明确原因的AKI 1(3.7) 4(17.4) χ2=1.800 0.180 治疗前血尿素氮/(mmol·L-1) 28.9±17.2 26.3±16.8 t=0.553 0.583 治疗前血清肌酐/(μmol·L-1) 615±650 437±223 t=1.249 0.218 治疗前血β2微球蛋白/(μg·L-1) 7746.0.±3891.4 7309.1±4696.8 t=0.360 0.721 治疗前血胱抑素C/(mg·L-1) 1.77±0.72 1.86±0.73 t=-0.414 0.681 -
[1] Chang CH, Fan PC, Chang MY, et al. Acute kidney injury enhances outcome prediction ability of sequential organ failure assessment score in critically ill patients[J]. PLoS One, 2014, 9(10): e109649. doi: 10.1371/journal.pone.0109649
[2] Yang L, Xing G, Wang L, et al. Acute kidney injury in China: a cross-sectional survey[J]. The Lancet, 2015, 386(10002): 1465-1471. doi: 10.1016/S0140-6736(15)00344-X
[3] Digvijay K, Neri M, Fan W, et al. International Survey on the Management of Acute Kidney Injury and Continuous Renal Replacement Therapies: Year 2018[J]. Blood Purif, 2019, 47(1-3): 113-119. doi: 10.1159/000493724
[4] Monti G, Herrera M, Kindgen-Milles D, et al. The DOse REsponse Multicentre International Collaborative Initiative(DO-RE-MI)[J]. Contrib Nephrol, 2007, 156(4): 34-43.
[5] Clark WR, Ding X, Qiu H, et al. Renal replacement therapy practices for patients with acute kidney injury in China[J]. PLoS One, 2017, 12(7): e0178509. doi: 10.1371/journal.pone.0178509
[6] Brunet S, Leblanc M, Geadah D, et al. Diffusive and convective solute clearances during continuous renal replacement therapy at various dialysate and ultrafiltration flow rates[J]. Am J Kidney Dis, 1999, 34(3): 486-492. doi: 10.1016/S0272-6386(99)70076-4
[7] Ricci Z, Ronco C, Bachetoni A, et al. Solute removal during continuous renal replacement therapy in critically ill patients: convection versus diffusion[J]. Crit Care, 2006, 10(2): R67. doi: 10.1186/cc4903
[8] Lyndon WD, Wille KM, Tolwani AJ. Solute clearance in CRRT: prescribed dose versus actual delivered dose[J]. Nephrol Dial Transplant, 2012, 27(3): 952-956. doi: 10.1093/ndt/gfr480
[9] Khwaja A. KDIGO clinical practice guidelines for acute kidney injury[J]. Nephron Clin Pract, 2012, 120(4): c179-184. doi: 10.1159/000339789
[10] Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016[J]. Intensive Care Med, 2017, 43(3): 304-377. doi: 10.1007/s00134-017-4683-6
[11] Mills EJ, Chan AW, Wu P, et al. Design, analysis, and presentation of crossover trials[J]. Trials, 2009, 10: 27-28. doi: 10.1186/1745-6215-10-27
[12] Smith JR, Zimmer N, Bell E, et al. A Randomized, Single-Blind, Crossover Trial of Recovery Time in High-Flux Hemodialysis and Hemodiafiltration[J]. Am J Kidney Dis, 2017, 69(6): 762-770. doi: 10.1053/j.ajkd.2016.10.025
[13] Claure-Del Granado R, Macedo E, Chertow GM, et al. Effluent volume in continuous renal replacement therapy overestimates the delivered dose of dialysis[J]. Clin J Am Soc Nephrol, 2011, 6(3): 467-475. doi: 10.2215/CJN.02500310
[14] Neri M, Villa G, Garzotto F, et al. Nomenclature for renal replacement therapy in acute kidney injury: basic principles[J]. Crit Care, 2016, 20(1): 318-329. doi: 10.1186/s13054-016-1489-9
[15] Ronco C, Bellomo R, Homel P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial[J]. Lancet, 2000, 356(9223): 26-30. doi: 10.1016/S0140-6736(00)02430-2
[16] Vesconi S, Cruz DN, Fumagalli R, et al. Delivered dose of renal replacement therapy and mortality in critically ill patients with acute kidney injury[J]. Crit Care, 2009, 13(2): R57-71. doi: 10.1186/cc7784
[17] Zhang Z, Ni H, Fan H, et al. Actually delivered dose of continuous renal replacement therapy is underestimated in hemofiltration[J]. ASAIO J, 2013, 59(6): 622-6226. doi: 10.1097/MAT.0000436713.34635.a8
[18] Calderaro V, Memoli B, Andreucci V, et al. Influence of Concentration Polarization in Post-Dilutional Hernofiltration of Human Plasma[J]. Artificial Organs, 1980, 4(4): 317-321.
[19] Marshall MR. Current status of dosing and quantification of acute renal replacement therapy. Part 1: mechanisms and consequences of therapy under-delivery[J]. Nephrology(Carlton), 2006, 11(3): 171-180.
[20] Pasko DA, Churchwell MD, Salama NN, et al. Longitudinal hemodiafilter performance in modeled continuous renal replacement therapy[J]. Blood Purif, 2011, 32(2): 82-88. doi: 10.1159/000324191
[21] Brain M, Winson E, Roodenburg O, et al. Non anti-coagulant factors associated with filter life in continuous renal replacement therapy(CRRT): a systematic review and meta-analysis[J]. BMC Nephrol, 2017, 18(1): 69. doi: 10.1186/s12882-017-0445-5
[22] Uchino S, Fealy N, Baldwin I, et al. Continuous is not continuous: the incidence and impact of circuit "down-time" on uraemic control during continuous veno-venous haemofiltration[J]. Intensive Care Med, 2003, 29(4): 575-578. doi: 10.1007/s00134-003-1672-8
[23] Kellum JA, Dishart MK. Effect of hemofiltration filter adsorption on circulating IL-6 levels in septic rats[J]. Crit Care, 2002, 6(5): 429-433. doi: 10.1186/cc1528
-




 下载:
下载: