Analysis of clinical efficacy of reverse fluid resuscitation in patients with septic shock fluid overload
-
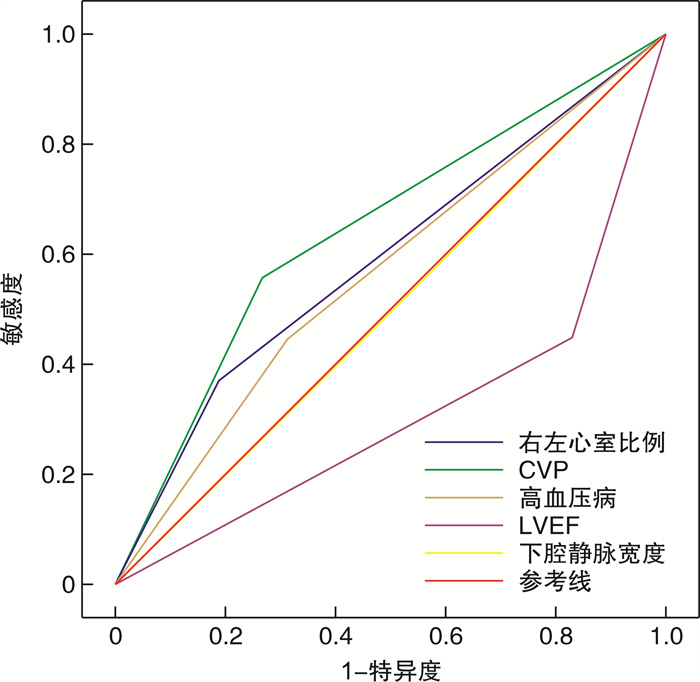
摘要: 目的 分析可能影响脓毒性休克液体过负荷患者反向液体复苏临床疗效的相关因素,指导临床医师判断合适的反向液体复苏的时机。方法 按时间顺序选取2019年1月—2022年1月在开封市中心医院住院并诊断为脓毒性休克的85例患者为研究对象,按照2018年中国脓毒性休克指南进行规范化治疗,早期积极液体复苏治疗,若出现心衰、组织水肿等容量过负荷时,综合判断后进行反向液体复苏(利尿剂应用或血液净化超滤治疗)。统计可能影响患者反向液体复苏临床疗效的11项相关因素:性别、年龄、高血压病史、糖尿病史、冠心病史;记录反向液体复苏前患者的中心静脉压(CVP)、下腔静脉宽度、呼气末正压(PEEP)(机械通气患者)、平均肺动脉压、左室射血分数(LVEF)、右心/左心比例。根据反向液体复苏前后患者心排血量(CO)的变化来判断是否复苏成功并分成2个组:复苏成功组(CO增加组)、复苏失败组(CO未增加组),比较2组以上观察指标的差异,对有差异的指标与反向液体复苏成功的结局进行二分类logistic回归分析判断其相关性。结果 2组患者的性别、年龄、糖尿病史、冠心病史、平肺动脉压比较差异无统计学意义(P>0.05);高血压病史、CVP、下腔静脉宽度、PEEP、LVEF、右心/左心比例比较差异有统计学意义(P< 0.05)。将以上差异有统计学意义的5项指标按照临床共识或者中位数等标准进行二分类[高血压病(有/无)、CVP(< 20 cmH2O/≥20 cmH2O)、下腔静脉宽度(< 2.0 cm/≥2.0 cm)、右心/左心比例(< 0.6=0/≥0.6)、LVEF(< 45%/≥45%)],与反向液体复苏成功结局之间进行logistic条件向后逐步回归分析显示:X1(有高血压病)(R=3.638)、X2(CVP≥20 cmH2O)(R=3.204)、X4(右心/左心比例≥0.6)(R=0.125)(P< 0.05)与反向液体复苏成功的结局独立相关。建立反向液体复苏成功预测模型方程:logitP=In(P/1-P)=-1.530 +1.291X1+1.164X2+1.996X4。对模型的拟合优度检验,得出χ2=16.183,P=0.023,具有较好的拟合优度。预测反向液体复苏成功概率与实际液体反向复苏成功概率差异无统计学意义。结论 患者既往有高血压病史、反向液体复苏前CVP≥20 cmH2O、右心/左心比例≥0.6是判断脓毒性休克容量过负荷患者反向液体复苏是否能成功的独立影响因素;当脓毒性休克患者出现容量过负荷表现,并符合以上3项条件时进行反向液体复苏会有效提高复苏成功率。Abstract: Objective To analyze the related factors that may affect the clinical efficacy of reverse fluid resuscitation in patients with septic shock fluid overload, and to guide clinicians to judge the appropriate time of reverse fluid resuscitation.Methods Eighty-five patients with septic shock hospitalized in EICU of Kaifeng Central Hospital from January 2019 to January 2022 were selected in chronological order. Standardized treatment and early active fluid resuscitation were carried out according to the 2108 Chinese guidelines for septic shock. In case of volume overload such as heart failure and tissue edema, reverse fluid resuscitation(diuretic application or blood purification ultrafiltration treatment) was comprehensively judged. Eleven factors that may affect the clinical efficacy of the reverse fluid resuscitation were statistically analyzed: gender, age, history of hypertension, diabetes mellitus, and coronary heart disease. Central venous pressure(CVP), inferior vena cava width, positive end expiratory pressure(PEEP)(patients with mechanical ventilation), mean pulmonary artery pressure, left ventricular ejection fraction(LVEF), and right/left heart ratio were recorded before reverse fluid resuscitation. According to the changes of cardiac output(CO) before and after reverse fluid resuscitation, judge whether it is successful resuscitation, and divide it into two groups: successful resuscitation group(co increased group) and failed resuscitation group(co not increased group). Compare the differences of more than two observation indexes between the two groups, and conduct binary logistic regression analysis to judge the correlation between the different indexes and the outcome of successful reverse fluid resuscitation.Results There were no significant differences in gender, age, diabetes history, coronary heart disease and pulmonary artery pressure between the two groups(P>0.05). There were significant differences in hypertension history, CVP, inferior vena cava width, peep, LVEF and right/left heart ratio(P< 0.05); the above five indicators with statistical differences were classified into two categories according to clinical consensus or median[hypertension](yes/no), CVP(< 20 cmH2O/≥ 20 cmH2O), inferior vena cava width(< 2.0 cm/≥ 2.0 cm), right heart/left heart ratio(< 0.6/≥0.6), LVEF(< 45%/≥45%) ], logistic conditional backward stepwise regression analysis showed that there was hypertension(R=3.638), CVP ≥ 20 cmH2O(R=3.204) right/left heart ratio≥ 0.6(R=0.125)(P< 0.05) was independently associated with the outcome of successful reverse fluid resuscitation. Establish the prediction model equation of reverse fluid resuscitation success: logitP=in(P/1-P)=-1.530+1.291X1+1.164X2+1.996X4. Where p is the success probability of NIV. The goodness of fit test of the model shows thatχ2=16.183,P=0.023, which has a good goodness of fit. There was no significant difference between the predicted success probability of reverse fluid resuscitation and the actual success probability of reverse fluid resuscitation.Conclusion The patient has a history of hypertension in the past; CVP ≥ 20 cmH2O and right/left heart ratio ≥ 0.6, before reverse fluid resuscitation are independent factors to judge the success of reverse fluid resuscitation in patients with septic shock volume overload. When the above three conditions are met, reverse fluid resuscitation will effectively improve the success rate of reverse fluid resuscitation.
-
Key words:
- septic shock /
- reverse fluid resuscitation
-

-
表 1 2组一般资料及疗效的比较
例,X±S 复苏成功组(n=47) 复苏失败组(n=38) t/χ2 P 性别 男 29 28 1.360 0.24 女 18 10 年龄/岁 68.14+13.25 68.86+11.14 0.063 0.803 高血压病史 有 27 10 8.284 0.003 无 20 28 糖尿病史 有 21 19 0.233 0.620 无 26 19 冠心病 有 22 18 0.070 0.780 无 25 20 CVP 17.89±3.80 12.07±2.58 4.246 0.042 下腔静脉宽度 1.94±0.51 1.82±0.39 3.790 0.049 PEEP 7.97±2.84 7.52±3.35 2.261 0.136 肺动脉压 27.21±5.84 27.81±5.12 0.952 0.332 LVEF 45.21±11.95 44.31±7.82 5.912 0.017 右心/左心比例 0.66±0.07 0.32±0.06 4.316 0.041 表 2 反向液体复苏成功相关因素赋值
自变量 赋值说明 高血压病(X1) 有=0,无=1, CVP(X2) < 20 cmH2O=0,≥20 cmH2O=1 下腔静脉宽度(X3) < 2.0 cm=0,≥2.0 cm=1 右心/左心比例(X4) < 0.6=0,≥0.6=1 LVEF(X5) < 45%=0,≥45%=1 表 3 反向液体复苏成功相关因素logistic条件向后回归分析结果
B S.E Wals df Sig. Exp(B) 高血压病 1.291 0.499 6.712 1 0.010 3.638 CVP 1.164 0.467 6.226 1 0.013 3.204 下腔静脉宽度 0.668 0.473 1.997 1 0.158 1.951 右心/左心比例 1.966 0.483 7.602 1 0.012 0.140 LVEF -0.651 0.493 1.744 1 0.187 0.522 常量 -1.530 0.494 9.614 1 0.002 0.216 -
[1] 何怀武, 隆云. 容量状态与容量反应性[J]. 中国医刊, 2016, 51(7): 13-16. doi: 10.3969/j.issn.1008-1070.2016.07.004
[2] 陈齐红, 郑瑞强, 林华, 等. 脓毒性休克液体管理对预后的影响[J]. 中华临床感染病杂志, 2010, 3(6): 369-371. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS201717023.htm
[3] 重症血流动力学治疗协作组(CHTC Group). 重症右心功能管理专家共识[J]. 中华内科杂志, 2017, 56(12): 962-973. doi: 10.3760/cma.j.issn.0578-1426.2017.12.019
[4] 中国医师协会急诊医师分会, 中国研究型医院学会休克与脓毒症专业委员会. 中国脓毒症/脓毒性休克急诊治疗指南(2018)[J]. 感染、炎症、修复, 2019, 20(1): 3-22. doi: 10.3969/j.issn.1672-8521.2019.01.001
[5] 龚仕金, 宋佳. 重症超声: 评估容量反应性的有力武器[J]. 现代实用医学, 2018, 30(4): 421-424. doi: 10.3969/j.issn.1671-0800.2018.04.001
[6] 黄薇, 张宏民, 王小亭, 等. 容量管理认识面面观[J]. 协和医学杂志, 2019, 10(5): 450-455. doi: 10.3969/j.issn.1674-9081.2019.05.005
[7] Kuttab HI, Lykins JD, Hughes MD, et al. Evaluation and Predictors of Fluid Resuscitation in Patients With Severe Sepsis and Septic Shock[J]. Crit Care Med, 2019, 47(11): 1582-1590. doi: 10.1097/CCM.0000000000003960
[8] Papayannopoulos V. Neutrophil extracellular traps in immunity and disease[J]. Nat Rev Immunol, 2018, 18(2): 134-147. doi: 10.1038/nri.2017.105
[9] Wessels I, Pupke JT, von Trotha KT, et al. Zinc supplementation ameliorates lung injury by reducing neutrophil recruitment and activity[J]. Thorax, 2020, 75(3): 253-261. doi: 10.1136/thoraxjnl-2019-213357
[10] 关红, 杜俊凯. NICaS监测脓毒症休克患者体液复苏的应用及对微循环、血流动力学的影响[J]. 中国急救复苏与灾害医学杂志, 2021, 16(11): 1262-1265. doi: 10.3969/j.issn.1673-6966.2021.11.015
[11] Denning NL, Aziz M, Gurien SD, et al. DAMPs and NETs in Sepsis[J]. Front Immunol, 2019, 10: 2536. doi: 10.3389/fimmu.2019.02536
[12] 朱然, 王小亭, 马晓春. 从右心认知到右心管理: 《重症右心功能管理专家共识》要点解读[J]. 协和医学杂志, 2018, 9(5): 407-410. doi: 10.3969/j.issn.1674-9081.2018.05.006
[13] Cheng L, Yan J, Han S, et al. Comparative efficacy of vasoactive medications in patients with septic shock: a network meta-analysis of randomized controlled trials[J]. Crit Care, 2019, 23(1): 168. doi: 10.1186/s13054-019-2427-4
[14] Lindberg O, De Geer L, Chew MS. Nonadherence to antibiotic guidelines in patients admitted to ICU with sepsis is associated with increased mortality: A registry-based, retrospective cohort study[J]. Eur J Anaesthesiol, 2020, 37(2): 113-120. doi: 10.1097/EJA.0000000000001140
[15] Ben-Nun-Shaul O, Srivastava R, Elgavish S, et al. Empty SV40 capsids increase survival of septic rats by eliciting numerous host signaling networks that participate in a number of systemic functions[J]. Oncotarget, 2020, 11(6): 574-588. doi: 10.18632/oncotarget.27448
[16] 朱晓雯, 侯金珍, 张奇, 等. 不同目标平均动脉压治疗对合并高血压的脓毒性休克患者胃肠功能的影响[J]. 中华危重病急救医学, 2021, 33(5): 517-522. doi: 10.3760/cma.j.cn121430-20200713-00515
[17] 原娇娇, 杨晓玲, 袁琪茜, 等. 基于脓毒性休克患者超声引导下液体复苏与早期目标导向治疗复苏效果的系统评价[J]. 中华危重病急救医学, 2020, 32(1): 56-61. doi: 10.3760/cma.j.cn121430-20191114-00010
[18] 郝翠平, 胡庆河, 朱丽娜, 等. 血乳酸和降钙素原与病情严重程度评分对脓毒性休克患者短期预后的联合预测价值[J]. 中华危重病急救医学, 2021, 33(3): 281-285. doi: 10.3760/cma.j.cn121430-20201113-00715
[19] Bouchery T, Moyat M, Sotillo J, et al. Hookworms Evade Host Immunity by Secreting a Deoxyribonuclease to Degrade Neutrophil Extracellular Traps[J]. Cell Host Microbe 2020, 27(2): 277-289. doi: 10.1016/j.chom.2020.01.011
[20] Powell D, Tauzin S, Hind LE, et al. Chemokine Signaling and the Regulation of Bidirectional Leukocyte Migration in Interstitial Tissues[J]. Cell Rep, 2017, 19(8): 1572-1585. doi: 10.1016/j.celrep.2017.04.078
[21] 任娜, 刘名胜, 周森. 液体复苏前后外周灌注指数水平对脓毒性休克患者28 d死亡风险预测价值的研究[J]. 临床急诊杂志, 2021, 22(6): 377-382. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=4f02dc04-8a22-400a-853c-0dadff2131c7
[22] 中华医学会急诊医学分会, 中国医师协会急诊医师分会, 中国人民解放军急救医学专业委员会, 中国医疗保健国际交流促进会急诊急救专业委员会. 脓毒症液体治疗急诊专家共识[J]. 中华急诊医学杂志, 2018, 27(1): 30-38. doi: 10.3760/cma.j.issn.1671-0282.2018.01.007
[23] Wang J, Hossain M, Thanabalasuriar A, et al. Visualizing the function and fate of neutrophils in sterile injury and repair[J]. Science, 2017, 358(6359): 111-116. doi: 10.1126/science.aam9690
[24] Wang J. Neutrophils in tissue injury and repair[J]. Cell Tissue Res, 2018, 371(3): 531-539. doi: 10.1007/s00441-017-2785-7
-




 下载:
下载: