Predictive value of acquired antithrombin-Ⅲ reduction on risk of mortality in patients with sepsis
-
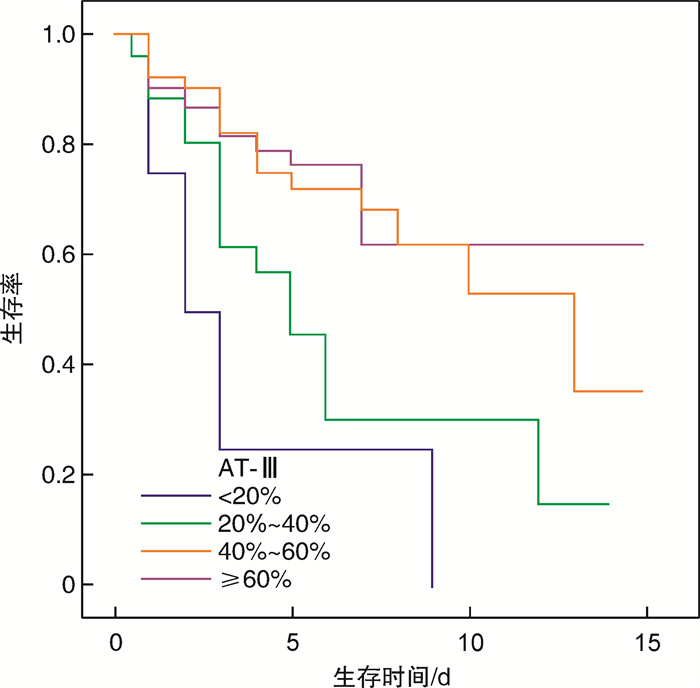
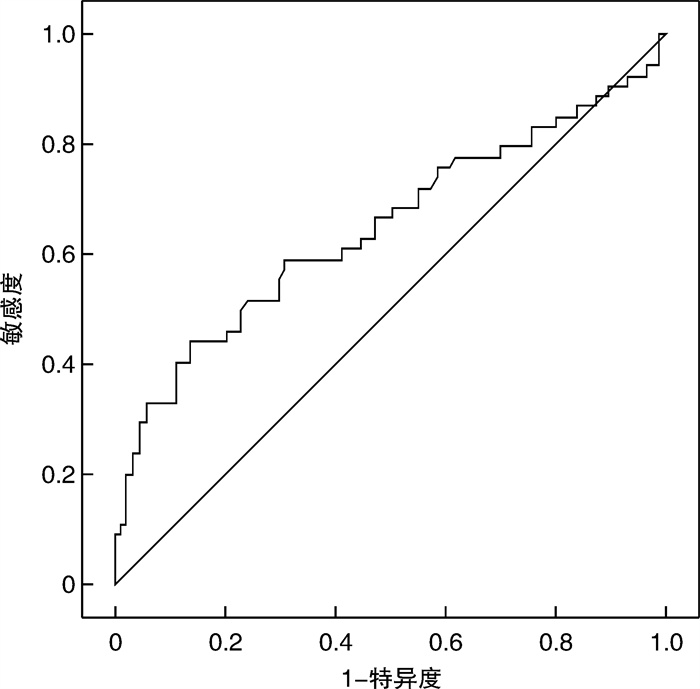
摘要: 目的 分析获得性抗凝血酶-Ⅲ(AT-Ⅲ)降低对脓毒症患者死亡风险预测的敏感度和特异度,为临床救治脓毒症患者、降低脓毒症患者死亡风险提供依据。方法 回顾性分析2020年6月-2021年9月期间武汉大学人民医院重症医学科收治的141例脓毒症患者病历资料。根据患者预后情况分为脓毒症存活组和死亡组,比较两组患者的急性生理与慢性健康Ⅱ(APACHE Ⅱ)评分、全身感染相关性器官功能衰竭评价系统(SOFA)评分、入住ICU时的AT-Ⅲ值、住ICU期间是否行机械通气、是否输血、是否使用血管活性药、感染部位、病原菌及住ICU时长等。结果 141例患者中,死亡54例,存活87例,死亡组的脓毒症患者的AT-Ⅲ值及住ICU时间明显低于生存组患者,APACHEⅡ评分、SOFA评分、凝血酶原时间(PT)、部分活化凝血酶原时间(APTT)、总胆红素(TBIL)、直接胆红素(DBIL)等均显著高于生存组,对上述有统计学意义的单因素纳入logistic回归模型中进行多因素分析发现只有AT-Ⅲ值及住ICU时间差异有统计学意义,作ROC曲线发现AT-Ⅲ诊断脓毒症患者死亡风险高的阈值为≤42.5%。结论 获得性AT-Ⅲ降低可作为脓毒症患者预后判断的有效指标,当脓毒症患者的AT-Ⅲ下降至42.5%及以下时,提示患者病死率明显升高。Abstract: Objective To explore the predictive value of acquired AT-Ⅲ reduction on risk of mortality in patients with sepsis and provide a basis for clinical treatment of sepsis patients and reduction of risk of death in patients with sepsis.Methods One hundred and forty one patients with sepsis treated in the Department of Critical Medicine of Wuhan University People's Hospital from June 2020 to September 2021 were enrolled for the retrospective analysis. According to the patient's prognosis, patients were divided into sepsis survival group and death group. The APACHE Ⅱ score, SOFA score, AT-Ⅲ value at ICU, access to mechanical ventilation during residence in ICU, whether to accept blood transfusion, application of vascular active drugs, infection site, pathogens and ICU duration were compared.Results Of the 141 enrolled patients with sepsis, 54 died and 87 survived, the AT-Ⅲ value and residence time in ICU of sepsis patients in the death group were significantly lower than those in the survival group, and the APACHEII score, SOFA score, PT, APTT, total bilirubin (TBIL), direct bilirubin (DBIL) and so on were significantly higher than those in the survival group. Multivariate logistic regression was used to analyze the statistically significant single factors and found that there were statistical differences of the AT-Ⅲ value and ICU length of stay between the two groups. ROC curve analysis showed that the HIGH threshold for the death risk of patients diagnosed with sepsis was found to be ≤ 42.5%.Conclusion The reduction of acquired AT-Ⅲ can be used as an effective indicator of prognosis in patients with sepsis, and AT-Ⅲ under 42.5% in patients with sepsis may indicate increased mortality rate.
-
Key words:
- sepsis /
- antithrombin-Ⅲ /
- risk of death /
- prognosis
-

-
表 1 存活组及死亡组患者入科时的基线资料
X±S 基线资料 存活组(87例) 死亡组(54例) t/Z P 年龄/岁 59.29±12.65 63.63±11.46 2.053 0.042 性别/例 2.67 0.102 男 51 39 女 36 15 入科体温/℃ 36.92±0.74 36.74±0.6 -1.474 0.143 APACHEⅡ评分 13.51±5.56 17.8±6.21 4.257 < 0.001 SOFA评分 5.59±2.71 8.81±3.64 6.017 < 0.001 PCT/(ng·mL-1) 15.12±20.2 16.41±27.09 0.321 0.748 CRP/(mg·L-1) 126.47±47.67 120.23±53.11 -0.724 0.471 PT/s 14.3±4.32 18.46±11.93 2.956 0.004 APTT/s 32.69±7.57 39.05±14.75 3.375 0.001 二聚体/(mg·L-1) 9.82±15.7 15.24±20.19 1.781 0.077 Cr/(μmol·mL-1) 171.69±170.34 185.33±214.02 0.418 0.676 ALT/(IU·L-1) 71.06±216.37 97.93±217.12 0.716 0.475 AST/(IU·L-1) 100.09±335.91 220.8±665.43 1.426 0.156 TBIL/(μmol·L-1) 24.22±27.2 50.7±82.36 2.769 0.006 DBIL/(μmol·L-1) 13.35±18.55 34.13±58.89 3.06 0.003 PO2/mmHga) 117.15±42.09 105.57±58.79 -1.36 0.176 AT-Ⅲ/% 60.84±18.09 51.00±24.59 -2.73 0.007 Lac/(mmol·L-1) 2.18±4.64 3.46±3.52 1.741 0.084 注:a)1 mmHg=0.133 kPa。 表 2 存活组及死亡组患者住院期间其他数据的对比
例,X±S 项目 存活组(87例) 死亡组(54例) t/ Z P 是否栓塞 0.006 0.936 否 84 52 是 3 2 是否出血 0.044 0.834 否 78 49 是 9 5 是否用血管活性药 12.89 < 0.001 否 62 22 是 25 32 MV时间/d 0.49±1.71 2.26±2.69 4.77 < 0.001 住ICU时间/d 6.49±3.84 4.31±3.99 -3.24 0.001 表 3 多因素logistic回归分析变量中的差异性
变量 B 标准误差 瓦尔德 自由度 显著性 OR(95%CI) 年龄 -0.004 0.014 0.1 1 0.751 1(0.97~1.02) ApⅡ评分 0.019 0.047 0.163 1 0.686 1.02(0.93~1.12) SOFA评分 0.108 0.099 1.196 1 0.274 1.12(0.92~1.35) PT 0.009 0.039 0.059 1 0.808 1.01(0.94~1.09) APTT -0.015 0.025 0.341 1 0.56 0.99(0.94~1.04) TBIL -0.03 0.024 1.607 1 0.205 0.97(0.93~1.02) DBIL 0.045 0.035 1.637 1 0.201 1.05(0.98~1.12) MV时间 0.385 0.123 9.728 1 0.002 1.47(1.15~1.87) 是否用血管活性药 0.365 0.465 0.618 1 0.432 1.44(0.58~3.58) AT-Ⅲ -0.024 0.009 6.859 1 0.009 0.98(0.96~0.99) 是否输血 0.023 0.448 0.003 1 0.959 1.02(0.43~2.46) 注:分类变量以第一分类为参比类别。 表 4 AT-Ⅲ≤42.5%与脓毒症患者的病死率明显相关
变量 诊断阈值/% P AUC SE 95%CI 敏感度/% 特异度/% 约登指数 AT-Ⅲ ≤42.5 0.0036 0.648 0.051 0.564~0.727 44.44 86.21 0.3065 -
[1] Manjappachar NK, Cuenca JA, Ramírez CM, et al. Outcomes and Predictors of 28-Day Mortality in Patients With Hematologic Malignancies and Septic Shock Defined by Sepsis-3 Criteria[J]. J Natl Compr Canc Netw, 2022, 20(1): 45-53. doi: 10.6004/jnccn.2021.7046
[2] Chee SS, Jawaid M, Alothman OY, et al. Effects of Nanoclay on Mechanical and Dynamic Mechanical Properties of Bamboo/Kenaf Reinforced Epoxy Hybrid Composites[J]. Polymers(Basel), 2021, 13(3): 395.
[3] 郭伟, 李平, 陈翠, 等. 脓毒症诱导T细胞功能紊乱及免疫治疗进展[J]. 临床急诊杂志, 2020, 21(9): 758-762. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=5bed3f4b-7e39-4b82-803d-9e8589c4191f
[4] Mayeux PR, MacMillan-Crow LA. Pharmacological targets in the renal peritubular microenvironment: implications for therapy for sepsis-induced acute kidney injury[J]. Pharmacol Ther, 2012, 134(2): 139-155. doi: 10.1016/j.pharmthera.2012.01.004
[5] Paoli CJ, Reynolds MA, Sinha M, et al. Epidemiology and Costs of Sepsis in the United States-An Analysis Based on Timing of Diagnosis and Severity Level[J]. Crit Care Med, 2018, 46(12): 1889-1897. doi: 10.1097/CCM.0000000000003342
[6] Lu Z, Wang F, Liang M. SerpinC1/Antithrombin Ⅲ in kidney-related diseases[J]. Clin Sci(Lond), 2017, 131(9): 823-831. doi: 10.1042/CS20160669
[7] Lu Z, Cheng D, Yin J, et al. Antithrombin Ⅲ Protects Against Contrast-Induced Nephropathy[J]. EBioMedicine, 2017, 17(2): 101-107.
[8] Iba T, Levy JH, Aihara K, et al. Newly Developed Recombinant Antithrombin Protects the Endothelial Glycocalyx in an Endotoxin-Induced Rat Model of Sepsis[J]. Int J Mol Sci, 2020, 22(1): 176. doi: 10.3390/ijms22010176
[9] Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287
[10] Xie J, Wang H, Kang Y, et al. The Epidemiology of Sepsis in Chinese ICUs: A National Cross-Sectional Survey[J]. Crit Care Med, 2020, 48(3): e209-e218. doi: 10.1097/CCM.0000000000004155
[11] Weng L, Zeng XY, Yin P, et al. Sepsis-related mortality in China: a descriptive analysis[J]. Intensive Care Med, 2018, 44(7): 1071-1080. doi: 10.1007/s00134-018-5203-z
[12] Allingstrup M, Wetterslev J, Ravn FB, et al. Antithrombin Ⅲ for critically ill patients: a systematic review with meta-analysis and trial sequential analysis[J]. Intensive Care Med, 2016, 42(4): 505-520. doi: 10.1007/s00134-016-4225-7
[13] Hayakawa M, Saito S, Uchino S, et al. Characteristics, treatments, and outcomes of severe sepsis of 3195 ICU-treated adult patients throughout Japan during 2011-2013[J]. J Intensive Care, 2016, 12(4): 44.
[14] 王曼, 谭奕东, 温福铭, 等. 不同监测方法指导下的脓毒症凝血功能障碍患者的肝素抗凝治疗研究[J]. 临床急诊杂志, 2021, 22(2): 87-91. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=c931b734-67ef-4836-9294-a946637ff1db
[15] 张鑫, 李小石, 周国平, 等. 血浆钙网蛋白水平与脓毒症患者预后的关系[J]. 临床急诊杂志, 2020, 21(6): 456-460. http://zzlc.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=b8323555-6239-4f78-ada6-25cf683e4f8a
-




 下载:
下载: