Evaluation of the short-term prognosis in patients after cardiopulmonary resuscitation using the combination of blood lactate-to-albumin ratio and D-dimer
-
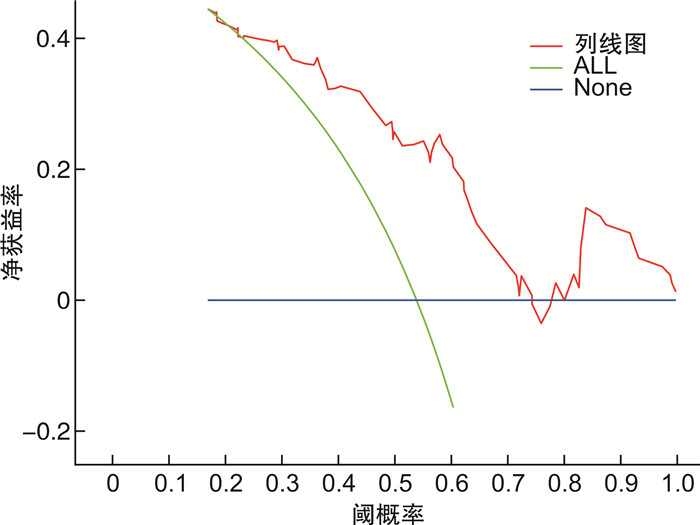
摘要: 目的 探讨血乳酸与白蛋白比值(lactate-to-albumin ratio,LAR)联合D-二聚体对院内心脏骤停(in-hospital cardiac arrest,IHCA)后患者短期预后的评估价值。方法 选取2017年7月—2024年6月哈尔滨医科大学附属第二医院收治的78例心肺复苏后自主循环恢复的患者进行回顾性研究,根据患者7 d内是否存活分为存活组和死亡组。收集患者的人口统计数据、合并症信息及实验室检查结果,包括乳酸、白蛋白、D-二聚体等,并计算LAR。采用logistic回归分析评估影响患者短期预后的独立危险因素,并建立列线图预测模型。结果 单因素和多因素logistic回归分析显示,LAR和D-二聚体是影响IHCA患者7 d预后的独立危险因素(P < 0.05)。基于LAR和D-二聚体构建的列线图预测模型显示出良好的预测性能,曲线下面积(AUC)为0.786(95%CI:0.685~0.882),灵敏度为83.3%,特异度为66.7%。结论 血乳酸与白蛋白比值联合D-二聚体能够有效评估IHCA患者复苏后的短期预后,为临床决策提供参考。Abstract: Objective To evaluate the prognostic value of the lactate-to-albumin ratio(LAR) combined with D-dimer for short-term outcomes in patients after in-hospital cardiac arrest(IHCA).Methods A retrospective study was conducted among 78 patients who achieved return of spontaneous circulation(ROSC) following cardiopulmonary resuscitation(CPR) for IHCA at the Second Affiliated Hospital of Harbin Medical University from July 2017 to June 2024. Patients were divided into survival and non-survival groups based on their survival status within 7 days. Demographic data, comorbidity information, and laboratory test results including lactate, albumin, and D-dimer were collected, and the LAR was calculated. logistic regression analysis was used to identify independent risk factors affecting short-term prognosis, and a nomogram prediction model was established.Results Univariate and multivariate logistic regression analyses revealed that LAR and D-dimer were independent risk factors for 7-day mortality in IHCA patients(P < 0.05). The nomogram prediction model based on LAR and D-dimer exhibited good predictive performance, with an area under the curve(AUC) of 0.786(95%CI: 0.685-0.882), a sensitivity of 83.3%, and a specificity of 66.7%.Conclusion The combination of the lactate-to-albumin ratio and D-dimer effectively assesses the short-term prognosis of IHCA patients after resuscitation, providing valuable information for clinical decision-making.
-
Key words:
- in-hospital cardiac arrest /
- lactate /
- albumin /
- D-dimer /
- short-term prognosis
-

-
表 1 生存组与死亡组IHCA后ROSC患者一般资料比较
项目 存活组(36例) 死亡组(42例) P 年龄/岁 55.47±16.66 59.79±15.82 0.245 性别/例(%) 0.598 男 15(41.7) 20(47.6) 女 21(58.3) 22(58.4) 高血压/例(%) 8(22.2) 13(31.0) 0.386 糖尿病/例(%) 8(22.2) 8(19.0) 0.729 冠心病/例(%) 15(41.7) 20(47.6) 0.598 肺部感染/例(%) 14(38.9) 18(42.9) 0.722 脑血管病/例(%) 13(36.1) 13(31.0) 0.630 肾功能不全/例(%) 6(16.7) 10(23.8) 0.436 WBC/(×109/L) 16.78±7.30 17.20±10.94 0.844 NEUT/(×109/L) 14.39±6.57 13.61±10.47 0.698 LYMPH/(×109/L) 1.92±1.46 3.03±2.65 0.290 MONO/(×109/L) 0.39±0.34 0.48±0.53 0.415 PLT/(×109/L) 235.94±107.07 210.19±124.95 0.336 HGB/(g/L) 115.97±31.15 118.64±36.43 0.731 PT/(SEC) 12.99±3.19 18.88±23.52 0.141 FIB/(g/L) 3.25±1.11 2.89±1.18 0.171 D-D/(ng/mL) 3 491.39±3 845.35 10 051.54±12 978.62 0.005 Scr/(μmol/L) 245.78±328.43 233.55±168.98 0.833 乳酸/(mmol/L) 6.83±4.55 11.29±3.88 < 0.001 ALB/(g/L) 33.75±5.31 31.59±7.69 0.161 LAR 0.22±0.17 0.39±0.17 < 0.001 表 2 单因素及多因素logistic回归分析IHCA后ROSC患者7 d死亡的危险因素
变量 单因素logistic回归分析 多因素logistic回归分析 OR(95%CI) P OR(95%CI) P LYMPH 1.292 5(1.014 2~1.647 3) 0.381 乳酸 1.3155(1.154 6~1.498 8) < 0.001 LAR 190.656 7(9.010 0~4034.416 0) < 0.001 2 112.699 8(29.345 7~1 521.495 8) 0.000 5 D-D 1.000 1(1.000 1~1.000 3) 0.009 7 1.000 2(1.000 1~1.000 4) 0.030 2 表 3 LAR与D-D评价IHCA后ROSC患者短期预后的评估价值
预测指标 AUC 截断值 灵敏度 特异度 LAR 0.724 0.272 0.694 0.786 D-D 0.706 2 665.5 0.661 0.738 联合指标 0.786 0.567 0.833 0.667 -
[1] Holmberg MJ, Ross CE, Fitzmaurice GM, et al. Annual Incidence of Adult and Pediatric In-Hospital Cardiac Arrest in the United States[J]. Circ Cardiovasc Qual Outcomes, 2019, 12(7): e005580. doi: 10.1161/CIRCOUTCOMES.119.005580
[2] Wang CY, Zheng W, Zheng JQ, et al. A national effort to improve outcomes for in-hospital cardiac arrest in China: the BASeline investigation of cardiac arrest(BASIC-IHCA)[J]. Resusc Plus, 2022, 11: 100259. doi: 10.1016/j.resplu.2022.100259
[3] 中国心脏骤停与心肺复苏报告编写组. 中国心脏骤停与心肺复苏报告(2022年版)概要[J]. 中国循环杂志, 2023, 38(10): 1005-1017.
[4] Yan SJ, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis[J]. Crit Care, 2020, 24(1): 61. doi: 10.1186/s13054-020-2773-2
[5] 中华医学会急诊医学分会复苏学组, 中国医药教育协会急诊专业委员会, 成人心脏骤停后综合征诊断和治疗中国急诊专家共识组. 成人心脏骤停后综合征诊断和治疗中国急诊专家共识[J]. 中华急诊医学杂志, 2021, 30(7): 799-808.
[6] Donnino MW, Andersen LW, Giberson T, et al. Initial lactate and lactate change in post-cardiac arrest: a multicenter validation study[J]. Crit Care Med, 2014, 42(8): 1804-1811. doi: 10.1097/CCM.0000000000000332
[7] Dell'Anna AM, Sandroni C, Lamanna I, et al. Prognostic implications of blood lactate concentrations after cardiac arrest: a retrospective study[J]. Ann Intensive Care, 2017, 7(1): 101. doi: 10.1186/s13613-017-0321-2
[8] Arques S. Human serum albumin in cardiovascular diseases[J]. Eur J Intern Med, 2018, 52: 8-12. doi: 10.1016/j.ejim.2018.04.014
[9] Belinskaia DA, Voronina PA, Shmurak VI, et al. Serum albumin in health and disease: esterase, antioxidant, transporting and signaling properties[J]. Int J Mol Sci, 2021, 22(19): 10318. doi: 10.3390/ijms221910318
[10] Hong SI, Kim YJ, Cho YJ, et al. Predictive value of pre-arrest albumin level with GO-FAR score in patients with in-hospital cardiac arrest[J]. Sci Rep, 2021, 11: 10631. doi: 10.1038/s41598-021-90203-9
[11] Turcato G, Zaboli A, Sibilio S, et al. The role of lactate-to-albumin ratio to predict 30-day risk of death in patients with sepsis in the emergency department: a decision tree analysis[J]. Curr Med Res Opin, 2024, 40(3): 345-352. doi: 10.1080/03007995.2024.2314740
[12] Liu Q, Zheng HL, Wu MM, et al. Association between lactate-to-albumin ratio and 28-days all-cause mortality in patients with acute pancreatitis: a retrospective analysis of the MIMIC-Ⅳ database[J]. Front Immunol, 2022, 13: 1076121. doi: 10.3389/fimmu.2022.1076121
[13] Fries M, Tang WC, Chang YT, et al. Microvascular blood flow during cardiopulmonary resuscitation is predictive of outcome[J]. Resuscitation, 2006, 71(2): 248-253. doi: 10.1016/j.resuscitation.2006.02.023
[14] Udovenko A, Makogonenko Y, Korolova D, et al. Formation and elimination of soluble fibrin and D-dimer in the bloodstream[J]. Croat Med J, 2023, 64(6): 421-429. doi: 10.3325/cmj.2023.64.421
[15] Geissenberger F, Schwarz F, Probst M, et al. D-dimer predicts disease severity but not long-term prognosis in acute pulmonary embolism[J]. Clin Appl Thromb Hemost, 2019, 25: 1076029619863495. doi: 10.1177/1076029619863495
[16] Zhou BY, Zhang Q, Hu YC, et al. Association of D-dimer with long-term prognosis in type 2 diabetes mellitus patients with acute coronary syndrome[J]. Nutr Metab Cardiovasc Dis, 2022, 32(8): 1955-1962. doi: 10.1016/j.numecd.2022.05.013
[17] Wang JM, Feng AQ, Xu J, et al. D-dimer and its combination with blood lipid on prognosis of patients with acute ischemic stroke[J]. J Stroke Cerebrovasc Dis, 2020, 29(12): 105394. doi: 10.1016/j.jstrokecerebrovasdis.2020.105394
[18] Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care[J]. Circulation, 2020, 142(16_suppl_2): S366-S468.
[19] Nolan JP, Sandroni C, Böttiger BW, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care[J]. Intensive Care Med, 2021, 47(4): 369-421. doi: 10.1007/s00134-021-06368-4
[20] Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021[J]. Intensive Care Med, 2021, 47(11): 1181-1247. doi: 10.1007/s00134-021-06506-y
[21] Issa MS, Grossestreuer AV, Patel H, et al. Lactate and hypotension as predictors of mortality after in-hospital cardiac arrest[J]. Resuscitation, 2021, 158: 208-214. doi: 10.1016/j.resuscitation.2020.10.018
[22] Zhang MQ, Zhang Q, Yu YN, et al. Effects of early hemodynamics, oxygen metabolism, and lactate dynamics on prognosis of post-cardiac arrest syndrome[J]. Chin Med J, 2021, 135(3): 344-346.
[23] Shin TG, Jo IJ, Hwang SY, et al. Comprehensive interpretation of central venous oxygen saturation and blood lactate levels during resuscitation of patients with severe sepsis and septic shock in the emergency department[J]. Shock, 2016, 45(1): 4-9. doi: 10.1097/SHK.0000000000000466
[24] Park J, Hwang SY, Jo IJ, et al. Impact of metformin use on lactate kinetics in patients with severe sepsis and septic shock[J]. Shock, 2017, 47(5): 582-587. doi: 10.1097/SHK.0000000000000782
[25] Lee TR, Kang MJ, Cha WC, et al. Better lactate clearance associated with good neurologic outcome in survivors who treated with therapeutic hypothermia after out-of-hospital cardiac arrest[J]. Crit Care, 2013, 17(5): R260. doi: 10.1186/cc13090
[26] Hayashida K, Suzuki M, Yonemoto N, et al. Early lactate clearance is associated with improved outcomes in patients with postcardiac arrest syndrome: a prospective, multicenter observational study(SOS-KANTO 2012 study)[J]. Crit Care Med, 2017, 45(6): e559-e566. doi: 10.1097/CCM.0000000000002307
[27] Kong T, Chung SP, Lee HS, et al. The prognostic usefulness of the lactate/albumin ratio for predicting clinical outcomes in out-of-hospital cardiac arrest: a prospective, multicenter observational study(koCARC)study[J]. Shock, 2020, 53(4): 442-451. doi: 10.1097/SHK.0000000000001405
[28] Zeng YQ, Qin ZA, Guo ZW, et al. Non-linear relationship between basal serum albumin concentration and cardiac arrest in critically ill patients with end-stage renal disease: a cross-sectional study[J]. BMJ Open, 2022, 12(2): e051721. doi: 10.1136/bmjopen-2021-051721
[29] Ichkawa Y, Wada H, Ezaki M, et al. Elevated D-dimer levels predict a poor outcome in critically ill patients[J]. Clin Appl Thromb Hemost, 2020, 26: 1076029620973084. doi: 10.1177/1076029620973084
[30] Esmailian M, Vakili Z, Nasr-Esfahani M, et al. D-dimer levels in predicting severity of infection and outcome in patients with COVID-19[J]. Tanaffos, 2022, 21(4): 419-433.
[31] Deng YS, He LY, Yang J, et al. Serum D-dimer as an indicator of immediate mortality in patients with in-hospital cardiac arrest[J]. Thromb Res, 2016, 143: 161-165. doi: 10.1016/j.thromres.2016.03.001
[32] Szymanski FM, Karpinski G, Filipiak KJ, et al. Usefulness of the D-dimer concentration as a predictor of mortality in patients with out-of-hospital cardiac arrest[J]. Am J Cardiol, 2013, 112(4): 467-471. doi: 10.1016/j.amjcard.2013.03.057
-





 下载:
下载: