Analysis of pathogens and drug-resistance of bacterial pneumonia in emergency intensive care unit
-
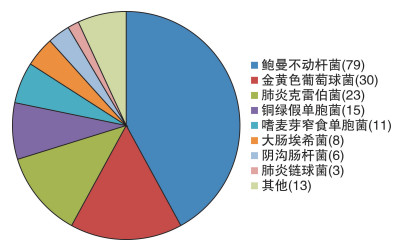
摘要: 目的 分析急诊重症监护室细菌性肺炎患者病原菌分类及耐药情况,指导细菌性肺炎的抗感染策略。方法 选取2018年1月—2019年11月期间入住海军军医大学第三附属医院急诊重症监护室的161例痰培养阳性的细菌性肺炎病例,分析检出细菌的种类及药敏情况。结果 检出致病菌中以革兰阴性菌为主(80.9%),菌群分布与同时间一些研究不尽相同。多重耐药菌常见,对于临床常用抗生素的耐药性较高。结论 急诊重症监护室细菌性肺炎患者培养菌株对于经验性抗感染治疗策略有一定的耐药性,了解所在病区的致病菌分类及耐药特点,有助于制订更有效的抗感染策略。Abstract: Objective To study and analyze pathogens and drug-resistance in patients with bacterial pneumonia in emergency intensive care unit (EICU), guiding the anti-infection strategy of bacterial pneumonia.Methods A total of 161 sputum culture-positive bacterial pneumonia patients admitted to the EICU of the Third Affiliated Hospital of Naval Medical University from January 2018 to November 2019 were selected to analyze pathogens and drug-resistance.Results Gram-negative bacteria (80.9%) were the main pathogenic bacteria. Multi-drug resistant organisms (MDRO) were common and had high resistance to commonly used antibiotics.Conclusion The pathogenic bacteria of the patients in the EICU bear certain resistance to empirical anti-infective treatment strategies. Understanding the classifications of pathogenic bacteria and the characteristics of drug-resistance is beneficial to develop a more effective anti-infection strategy.
-

-
表 1 鲍曼不动杆菌药敏试验结果
% 抗生素名称 菌株/株 耐药率 中敏率 敏感率 米诺环素 78 29.5 29.5 41.0 替加环素 32 0 0 100.0 头孢曲松 79 93.7 6.3 0 庆大霉素 78 78.2 5.1 16.7 复方新诺明 79 58.2 2.5 39.2 头孢吡肟 79 91.1 3.8 5.1 左旋氧氟沙星 76 84.2 9.2 6.6 妥布霉素 79 77.2 2.5 20.3 头孢他啶 79 94.9 0 5.1 环丙沙星 79 94.9 0 5.1 亚胺培南 79 92.4 1.3 6.3 氨苄西林/舒巴坦 78 80.8 10.3 9.0 哌拉西林/他唑巴坦 78 94.9 0 5.1 阿米卡星 79 78.5 1.3 20.3 美罗培南 78 91.0 0 9.0 多黏菌素B 9 11.1 0 88.9 表 2 甲氧西林耐药金黄色葡萄球菌药敏试验结果
% 抗生素名称 菌株/株 耐药率 中敏率 敏感率 庆大霉素 23 26.1 17.4 56.5 复方新诺明 23 0 0 100.0 左旋氧氟沙星 23 82.6 0 17.4 环丙沙星 23 82.6 0 17.4 青霉素G 23 100.0 0 0 苯唑西林 23 100.0 0 0 莫西沙星 23 73.9 4.3 21.7 克林霉素 23 87.0 0 13.0 万古霉素 23 0 0 100.0 红霉素 23 91.3 0 8.7 利奈唑胺 23 0 0 100.0 利福平 23 4.3 0 95.7 四环素 23 78.3 0 21.7 表 3 甲氧西林敏感金黄色葡萄球菌药敏试验结果
% 抗生素名称 菌株/株 耐药率 中敏率 敏感率 庆大霉素 7 0 0 100.0 复方新诺明 7 0 0 100.0 左旋氧氟沙星 7 0 0 100.0 环丙沙星 7 0 14.3 85.7 青霉素G 7 71.4 0 28.6 苯唑西林 7 0 0 100.0 莫西沙星 7 0 0 100.0 克林霉素 7 14.3 0 85.7 万古霉素 7 0 0 100.0 红霉素 6 16.7 0 83.3 利奈唑胺 7 0 0 100.0 利福平 7 0 0 100.0 四环素 7 14.3 0 85.7 -
[1] Ho J, Ip M. Antibiotic-Resistant Community-Acquired Bacterial Pneumonia[J]. Infect Dis Clin North Am, 2019, 33(4): 1087-1103. doi: 10.1016/j.idc.2019.07.002
[2] Zaragoza R, Vidal-Cortés P, Aguilar G, et al. Update of the treatment of nosocomial pneumonia in the ICU[J]. Crit Care, 2020, 24(1): 383. doi: 10.1186/s13054-020-03091-2
[3] 屈莉, 孔淑贞, 王维霞, 等. 综合医院急诊监护室收治患者疾病特点分析[J]. 中国病案, 2016, 17(1): 72-74. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGBN201601028.htm
[4] Vincent JL, Sakr Y, Singer M, et al. Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017[J]. JAMA, 2020, 323(15): 1478-1487. doi: 10.1001/jama.2020.2717
[5] 刘剑烽. 急诊病房下呼吸道感染患者各类标本细菌培养及药敏分析[J]. 临床急诊杂志, 2020, 21(2): 125-134. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202002006.htm
[6] 胡付品, 郭燕, 朱德妹, 等. 2018年CHINET中国细菌耐药性监测[J]. 中国感染与化疗杂志, 2020, 20(1): 1-10. https://www.cnki.com.cn/Article/CJFDTOTAL-KGHL202001001.htm
[7] Liang CA, Lin YC, Lu PL, et al. Antibiotic strategies and clinical outcomes in critically ill patients with pneumonia caused by carbapenem-resistant Acinetobacter baumannii[J]. Clin Microbiol Infect, 2018, 24(8): 908. e1-908. e7. doi: 10.1016/j.cmi.2017.10.033
[8] Amaya-Villar R, Garnacho-Montero J. How should we treat acinetobacter pneumonia?[J]. Curr Opin Crit Care, 2019, 25(5): 465-472. doi: 10.1097/MCC.0000000000000649
[9] Sharara SL, Maragakis LL, Cosgrove SE. Decolonization of Staphylococcus aureus[J]. Infect Dis Clin North Am, 2021, 35(1): 107-133. doi: 10.1016/j.idc.2020.10.010
[10] McGuinness WA, Malachowa N, DeLeo FR. Vancomycin Resistance in Staphylococcus aureus[J]. Yale J Biol Med, 2017, 90(2): 269-281.
[11] Vestergaard M, Frees D, Ingmer H. Antibiotic Resistance and the MRSA Problem[J]. Microbiol Spectr, 2019, 7(2).
[12] Inglis GD, Taboada EN, Boras VF. Rates of fluoroquinolone resistance in domestically acquired Campylobacter jejuni are increasing in people living within a model study location in Canada[J]. Can J Microbiol, 2021, 67(1): 37-52. doi: 10.1139/cjm-2020-0146
[13] Klemm EJ, Shakoor S, Page AJ, et al. Emergence of an Extensively Drug-Resistant Salmonella enterica Serovar Typhi Clone Harboring a Promiscuous Plasmid Encoding Resistance to Fluoroquinolones and Third-Generation Cephalosporins[J]. mBio, 2018, 9(1): e00105-18.
[14] 霍凤芝. 下呼吸道细菌感染及耐药菌性分析[J]. 临床急诊杂志, 2011, 12(4): 278-280. doi: 10.3969/j.issn.1009-5918.2011.04.027
[15] 彭映辉, 朱达. 重症监护病房呼吸机相关性肺炎多重耐药非发酵菌的感染情况及相关高危因素分析[J]. 临床急诊杂志, 2019, 20(5): 348-351. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC201905003.htm
[16] Medina E, Pieper DH. Tackling Threats and Future Problems of Multidrug-Resistant Bacteria[J]. Curr Top Microbiol Immunol, 2016, 398: 3-33.
[17] Martin-Loeches I, Torres A. New guidelines for severe community-acquired pneumonia[J]. Curr Opin Pulm Med, 2021, 27(3): 210-215. doi: 10.1097/MCP.0000000000000760
[18] Martin-Loeches I, Rodriguez AH, Torres A. New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe[J]. Curr Opin Crit Care, 2018, 24(5): 347-352. doi: 10.1097/MCC.0000000000000535
[19] 王乾, 张海峰, 张智舒, 等. 急诊科抢救室细菌性肺炎患者死亡的危险因素[J]. 临床急诊杂志, 2021, 22(6): 406-409. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202106009.htm
[20] Lanks CW, Musani AI, Hsia DW. Community-acquired Pneumonia and Hospital-acquired Pneumonia[J]. Med Clin North Am, 2019, 103(3): 487-501. doi: 10.1016/j.mcna.2018.12.008
-




 下载:
下载: