Lipoproteins abnormalities and prognostic value of blood urea nitrogen/lipoprotein(a) ratio in patients with severe community-acquired pneumonia
-
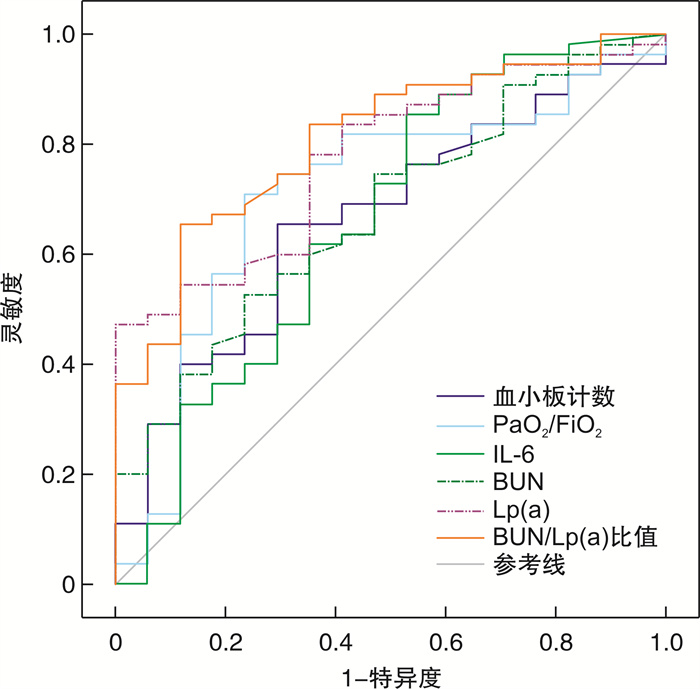
摘要: 目的 观察重症社区获得性肺炎(severe community-acquired pneumonia,SCAP)患者的血脂水平变化,探讨血尿素氮与脂蛋白a比值[BUN/Lp(a)]对SCAP患者重症监护病房(ICU)死亡的预测价值。方法 选取2021年3月至2023年3月在急诊重症监护病房(EICU)住院的72例SCAP患者。收集患者EICU入院后12 h内的血液检查结果,以及入院后第1天早晨的血脂和脂蛋白水平。根据患者ICU内是否死亡分为生存组(55例)和死亡组(17例)。采用受试者工作特征曲线和曲线下面积(AUC)评价BUN/Lp(a)比值的预测价值。结果 与生存组比较,死亡组患者白细胞介素-6(IL-6)、BUN、BUN/Lp(a)比值均显著升高(P<0.05)。死亡组患者氧合指数(PaO2/FiO2)、血小板计数、Lp(a)均显著低于生存组(P<0.05)。死亡组患者脓毒性休克的比例高于生存组(P=0.05)。IL-6、BUN、BUN/Lp(a)比值与SCAP患者ICU死亡呈弱的正相关性(P<0.05)。PaO2/FiO2和Lp(a)与SCAP患者ICU死亡呈弱的负相关性(P<0.05)。Lp(a)与SCAP患者血小板计数、低密度脂蛋白胆固醇、载脂蛋白B呈正相关性(P<0.05),Lp(a)与IL-6呈负相关性(P<0.05)。血小板计数、PaO2/FiO2、IL-6、BUN、Lp(a)水平和BUN/Lp(a)比值预测SCAP患者ICU死亡的AUC分别为0.665(95%CI 0.544~0.772)、0.709(95%CI 0.590~0.810)、0.660(95%CI 0.539~0.768)、0.678(95%CI 0.558~0.783)、0.776(95%CI 0.662~0.866)和0.809(95%CI 0.699~0.892)(均P<0.05)。AUC两两比较显示,BUN/Lp(a)比值的预测价值优于BUN(P=0.007 9)。BUN/Lp(a)比值预测ICU死亡的灵敏度为65.45%,特异度为88.24%(截断值=0.60)。结论 与生存组比较,SCAP患者死亡组的Lp(a)水平在入院时较低。BUN/Lp(a)比值是SCAP患者ICU死亡的良好预测指标,可能成为评估患者预后的一个很好的方法。Abstract: Objective To observe the changes in blood lipid levels in patients with severe community-acquired pneumonia(SCAP), and to explore the predictive value of blood urea nitrogen /lipoprotein(a) ratio(BUN/Lp[a]) for mortality in intensive care unit(ICU) of SCAP patients.Methods A total of seventy-two patients with SCAP hospitalized in the emergency intensive care unit(EICU) from March 2021 to March 2023 were included. Blood test results were collected within the first 12 h of EICU admission. The plasma lipid and lipoprotein levels in the morning of the first day after EICU admission were collected. The patients were divided into a survival group(55 cases) and a death group(17 cases). The predictive value was evaluated by using receiver operating characteristic curve and the area under the curve(AUC).Results Compared to patients in the survival group, the interleukin-6(IL-6), BUN, and BUN/Lp(a) ratio were significantly increased in patients with the death group(P < 0.05). Patients in the death group had significantly lower PaO2/FiO2, platelet count, Lp(a) than those in patients with the survival group(P < 0.05). The proportion of septic shock in patients in the death group was higher than that in the survival group(P=0.05). IL-6, BUN, and BUN/Lp(a) ratio showed a weak positive correlation with ICU death in patients with SCAP(P < 0.05). PaO2/FiO2 and Lp(a) showed a weak negative correlation with ICU death in patients with SCAP(P < 0.05). Lp(a) was positively correlated with platelet count, low-density lipoprotein cholesterol, and apolipoprotein B(P < 0.05), and Lp(a) was negatively correlated with IL-6 in SCAP patients(P < 0.05). The AUCs of platelet count, PaO2/FiO2, IL-6, BUN, Lp(a) levels, and BUN/Lp(a) ratio for predicting ICU death in patients with SCAP were 0.665(95%CI 0.544-0.772), 0.709(95%CI 0.590-0.810), 0.660(95%CI 0.539-0.768), 0.678(95%CI 0.558-0.783), 0.776(95%CI 0.662-0.866) and 0.809(95%CI 0.699-0.892), respectively(P < 0.05). A pairwise comparison of AUCs showed that the predictive value of BUN/Lp(a) ratio was significantly better than that of BUN(P=0.007 9). The sensitivity and specificity of the BUN/Lp(a) ratio in predicting ICU mortality were 65.45% and 88.24%, respectively, with a cut-off value of 0.60.Conclusion Compared with the survival group, the Lp(a) level in the death group of SCAP patients decreased upon admission. The BUN/Lp(a) ratio is a good predictor of ICU mortality in SCAP patients and may become a good alternate option for evaluating the prognosis of patients.
-

-
表 1 2组患者基线特征及实验室检查结果比较
临床资料 生存组(55例) 死亡组(17例) P 基线特征 年龄/岁 73(62,83) 78(64,84) 0.546 男/例(%) 41(74.5) 13(76.5) 1.000 APACHEⅡ评分 19.4±5.8 21.8±8.1 0.182 SBP/mmHg△ 119.6±25.3 111.7±17.8 0.240 DBP/mmHg 70(63,80) 63(55,68) 0.065 HR/(次/min) 99.8±17.9 108.2±26.6 0.236 PaO2/FiO2/mmHg 185.6±79.1 136.0±73.8 0.025 脓毒性休克/例(%) 15(27.3) 9(52.9) 0.050 合并症/例(%) 高血压 29(52.7) 11(64.7) 0.385 糖尿病 17(30.9) 4(23.5) 0.762 肾脏疾病 1(1.8) 1(5.9) 0.419 冠心病 13(23.6) 6(35.3) 0.359 慢性阻塞性肺疾病 2(3.6) 0 1.000 脑血管病 35(63.6) 11(64.7) 0.936 肝功能异常 3(5.5) 0 1.000 常规实验室检查 PCT/(ng/mL) 1.81(0.51,15.44) 6.91(0.45,19.44) 0.600 CRP/(mg/L) 159.36±120.47 191.55±94.30 0.317 IL-6/(pg/mL) 124.00(57.52,434.00) 390.10(86.81,3 194.50) 0.047 中性粒细胞计数/(×109/L) 9.85(6.12,12.76) 11.68(6.71,18.92) 0.225 淋巴细胞计数/(×109/L) 0.90(0.42,1.37) 0.47(0.26,1.09) 0.054 血小板计数/(×109/L) 188(143,274) 151(109,209) 0.041 D-dimer/(mg/L) 3.24(1.47,5.89) 2.28(1.22,8.72) 0.858 Lac/(mmol/L) 2.50(1.60,3.73) 2.70(1.85,4.55) 0.310 Alb/(g/L) 30.10(26.40,33.00) 31.10(27.10,32.40) 0.974 TBiL/(μmol/L) 16.40(11.70,22.80) 19.90(11.80,31.20) 0.389 Scr/(μmol/L) 72.00(55.10,113.30) 119.60(59.70,186.75) 0.132 BUN/(mmol/L) 8.30(4.90,13.60) 13.20(8.35,22.30) 0.027 血脂检查 TC/(mmol/L) 2.89±1.05 2.59±1.13 0.312 TG/(mmol/L) 1.13(0.77,1.64) 1.25(0.79,1.80) 0.507 HDL-C/(mmol/L) 0.79±0.26 0.74±0.38 0.553 LDL-C/(mmol/L) 1.80±0.70 1.59±0.75 0.304 VLDL-C/(mmol/L) 0.26(0.16,0.41) 0.24(0.13,0.38) 0.591 ApoA-1/(g/L) 0.73±0.28 0.62±0.28 0.154 ApoB/(g/L) 0.59±0.22 0.51±0.19 0.182 Lp(a)/(mg/dL) 15.81(11.16,29.48) 7.52(5.77,14.46) 0.001 BUN/Lp(a)比值 0.46(0.21,0.98) 1.77(0.80,2.69) <0.001 △1 mmHg=0.133 kPa。 表 2 SCAP患者ICU死亡相关因素的Spearman分析
相关因素 r P 年龄 0.071 0.552 PaO2/FiO2 -0.264 0.025 脓毒性休克 0.231 0.051 APACHEⅡ评分 0.159 0.182 PCT 0.046 0.701 CRP 0.120 0.317 IL-6 0.343 0.003 中性粒细胞计数 0.154 0.196 淋巴细胞计数 -0.192 0.106 血小板计数 -0.226 0.057 D-dimer 0.065 0.589 Lac 0.066 0.580 Alb -0.005 0.964 TBiL 0.214 0.071 Scr 0.117 0.329 BUN 0.273 0.020 TC -0.121 0.312 TG 0.027 0.821 HDL-C -0.071 0.553 LDL-C -0.123 0.304 VLDL-C -0.101 0.400 ApoA-1 -0.170 0.154 ApoB -0.159 0.182 Lp(a) -0.308 0.008 BUN/Lp(a)比值 0.395 0.001 表 3 SCAP患者Lp(a)水平相关因素的Spearman分析
相关因素 r P PaO2/FiO2 0.070 0.559 脓毒性休克 -0.177 0.136 APACHEⅡ评分 0.046 0.704 PCT -0.089 0.457 CRP -0.096 0.423 IL-6 -0.260 0.027 中性粒细胞计数 -0.080 0.503 淋巴细胞计数 0.091 0.446 血小板计数 0.314 0.007 D-dimer -0.121 0.311 Lac -0.155 0.193 Alb -0.096 0.423 TBiL -0.224 0.059 Scr 0.027 0.825 BUN -0.061 0.610 TC 0.210 0.077 TG -0.050 0.676 HDL-C 0.073 0.541 LDL-C 0.259 0.028 VLDL-C 0.063 0.598 ApoA-1 0.148 0.214 ApoB 0.241 0.041 表 4 ROC分析结果
相关因素 AUC 95%CI P 血小板计数 0.665 0.544~0.772 0.024 PaO2/FiO2 0.709 0.590~0.810 0.006 IL-6 0.660 0.539~0.768 0.047 BUN 0.678 0.558~0.783 0.013 Lp(a) 0.776 0.662~0.866 <0.001 BUN/Lp(a)比值 0.809 0.699~0.892 <0.001 表 5 血小板计数、PaO2/FiO2、IL-6、BUN、Lp(a)和BUN/Lp(a)比值预测SCAP患者ICU死亡的最佳临界值、灵敏度和特异度
相关因素 截断值 灵敏度/% 特异度/% 阳性似然比 阴性似然比 血小板计数/(×109/L) 169.00 65.45(95%CI 51.4~77.8) 70.59(95%CI 44.0~89.7) 2.23 0.49 PaO2/FiO2/mmHg 152.67 70.91(95%CI 57.1~82.4) 76.47(95%CI 50.1~93.2) 3.01 0.38 IL-6/(pg/mL) 1 111.00 85.45(95%CI 73.3~93.5) 47.06(95%CI 23.0~72.2) 1.61 0.31 BUN/(mmol/L) 8.60 52.73(95%CI 38.8~66.3) 76.47(95%CI 50.1~93.2) 2.24 0.62 Lp(a)/(mg/dL) 20.22 47.27(95%CI 33.7~61.2) 100.00(95%CI 80.5~100.0) - 0.53 BUN/Lp(a)比值 0.60 65.45(95%CI 51.4~77.8) 88.24(95%CI 63.6~98.5) 5.56 0.39 -
[1] GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2018, 392(10159): 1736-1788. doi: 10.1016/S0140-6736(18)32203-7
[2] Jain S, Self WH, Wunderink RG, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults[J]. N Engl J Med, 2015, 373(5): 415-427. doi: 10.1056/NEJMoa1500245
[3] 王重阳, 王璐, 郭仁楠, 等. ROX指数预测老年重症社区获得性肺炎患者气管插管的有效性分析[J]. 临床急诊杂志, 2022, 23(12): 854-858. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.12.010?viewType=HTML
[4] Cillóniz C, Dominedò C, Garcia-Vidal C, et al. Community-acquired pneumonia as an emergency condition[J]. Curr Opin Crit Care, 2018, 24(6): 531-539. doi: 10.1097/MCC.0000000000000550
[5] Montull B, Menéndez R, Torres A, et al. Predictors of Severe Sepsis among Patients Hospitalized for Community-Acquired Pneumonia[J]. PLoS One, 2016, 11(1): e0145929. doi: 10.1371/journal.pone.0145929
[6] Laudanski K. Persistence of Lipoproteins and Cholesterol Alterations after Sepsis: Implication for Atherosclerosis Progression[J]. Int J Mol Sci, 2021, 22(19): 10517. doi: 10.3390/ijms221910517
[7] Cirstea M, Walley KR, Russell JA, et al. Decreased high-density lipoprotein cholesterol level is an early prognostic marker for organ dysfunction and death in patients with suspected sepsis[J]. J Crit Care, 2017, 38: 289-294. doi: 10.1016/j.jcrc.2016.11.041
[8] Pizzini A, Kurz K, Orth-Hoeller D, et al. The impact of bacteremia on lipoprotein concentrations and patient's outcome: a retrospective analysis[J]. Eur J Clin Microbiol Infect Dis, 2019, 38(7): 1279-1286. doi: 10.1007/s10096-019-03543-w
[9] Reisinger AC, Schuller M, Holzer M, et al. Arylesterase Activity of HDL Associated Paraoxonase as a Potential Prognostic Marker in Patients With Sepsis and Septic Shock-A Prospective Pilot Study[J]. Front Med(Lausanne), 2020, 7: 579677.
[10] Reyes-Soffer G, Westerterp M. Beyond Lipoprotein(a)plasma measurements: Lipoprotein(a)and inflammation[J]. Pharmacol Res, 2021, 169: 105689. doi: 10.1016/j.phrs.2021.105689
[11] Apostolou F, Gazi IF, Lagos K, et al. Acute infection with Epstein-Barr virus is associated with atherogenic lipid changes[J]. Atherosclerosis, 2010, 212(2): 607-613. doi: 10.1016/j.atherosclerosis.2010.06.006
[12] Liu J, Sun LL, Wang J, et al. Blood urea nitrogen in the prediction of in-hospital mortality of patients with acute aortic dissection[J]. Cardiol J, 2018, 25(3): 371-376. doi: 10.5603/CJ.a2017.0075
[13] Gary T, Pichler M, Schilcher G, et al. Elevated Blood Urea Nitrogen is Associated With Critical Limb Ischemia in Peripheral Arterial Disease Patients[J]. Medicine(Baltimore), 2015, 94(24): e948.
[14] Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America[J]. Am J Respir Crit Care Med, 2019, 200(7): e45-e67. doi: 10.1164/rccm.201908-1581ST
[15] Golucci APBS, Marson FAL, Ribeiro AF, et al. Lipid profile associated with the systemic inflammatory response syndrome and sepsis in critically ill patients[J]. Nutrition, 2018, 55-56: 7-14. doi: 10.1016/j.nut.2018.04.007
[16] Ali Abdelhamid Y, Cousins CE, Sim JA, et al. Effect of Critical Illness on Triglyceride Absorption[J]. JPEN J Parenter Enteral Nutr, 2015, 39(8): 966-972. doi: 10.1177/0148607114540214
[17] Hofmaenner DA, Kleyman A, Press A, et al. The Many Roles of Cholesterol in Sepsis: A Review[J]. Am J Respir Crit Care Med, 2022, 205(4): 388-396. doi: 10.1164/rccm.202105-1197TR
[18] Apostolou F, Gazi IF, Kostoula A, et al. Persistence of an atherogenic lipid profile after treatment of acute infection with Brucella[J]. J Lipid Res, 2009, 50(12): 2532-2539. doi: 10.1194/jlr.P900063-JLR200
[19] Mooser V, Berger MM, Tappy L, et al. Major reduction in plasma Lp(a)levels during sepsis and burns[J]. Arterioscler Thromb Vasc Biol, 2000, 20(4): 1137-1142. doi: 10.1161/01.ATV.20.4.1137
[20] Klaude M, Mori M, Tjäder I, et al. Protein metabolism and gene expression in skeletal muscle of critically ill patients with sepsis[J]. Clin Sci(Lond), 2012, 122(3): 133-142. doi: 10.1042/CS20110233
[21] Peerapornratana S, Manrique-Caballero CL, Gómez H, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment[J]. Kidney Int, 2019, 96(5): 1083-1099. doi: 10.1016/j.kint.2019.05.026
[22] Li X, Zheng R, Zhang T, et al. Association between blood urea nitrogen and 30-day mortality in patients with sepsis: a retrospective analysis[J]. Ann Palliat Med, 2021, 10(11): 11653-11663. doi: 10.21037/apm-21-2937
[23] Feng DY, Zhou YQ, Zou XL, et al. Elevated Blood Urea Nitrogen-to-Serum Albumin Ratio as a Factor That Negatively Affects the Mortality of Patients with Hospital-Acquired Pneumonia[J]. Can J Infect Dis Med Microbiol, 2019, 2019: 1547405.
[24] Zou XL, Feng DY, Wu WB, et al. Blood urea nitrogen to serum albumin ratio independently predicts 30-day mortality and severity in patients with Escherichia coli bacteraemia[J]. Med Clin(Barc), 2021, 157(5): 219-225.
[25] Gentile LF, Cuenca AG, Vanzant EL, et al. Is there value in plasma cytokine measurements in patients with severe trauma and sepsis?[J]. Methods, 2013, 61(1): 3-9. doi: 10.1016/j.ymeth.2013.04.024
[26] Georgescu AM, Grigorescu BL, Chirteș IR, et al. The Relevance of Coding Gene Polymorphysms of Cytokines and Cellular Receptors in Sepsis[J]. J Crit Care Med(Targu Mures), 2017, 3(1): 5-11. doi: 10.1515/jccm-2017-0001
[27] Zhang LT, Xu X, Han H, et al. The value of NSE to predict ICU mortality in patients with septic shock: A prospective observational study[J]. Medicine(Baltimore), 2022, 101(40): e30941.
[28] Sharma B, Sharma M, Majumder M, et al. Thrombocytopenia in septic shock patients--a prospective observational study of incidence, risk factors and correlation with clinical outcome[J]. Anaesth Intensive Care, 2007, 35(6): 874-880. doi: 10.1177/0310057X0703500604
[29] Thiery-Antier N, Binquet C, Vinault S, et al. Is Thrombocytopenia an Early Prognostic Marker in Septic Shock?[J]. Crit Care Med, 2016, 44(4): 764-772. doi: 10.1097/CCM.0000000000001520
[30] Venkata C, Kashyap R, Farmer JC, et al. Thrombocytopenia in adult patients with sepsis: incidence, risk factors, and its association with clinical outcome[J]. J Intensive Care, 2013, 1(1): 9. doi: 10.1186/2052-0492-1-9
-




 下载:
下载: