Prognostic value of peripheral blood inflammatory index in sepsis associated with acute kidney injury
-
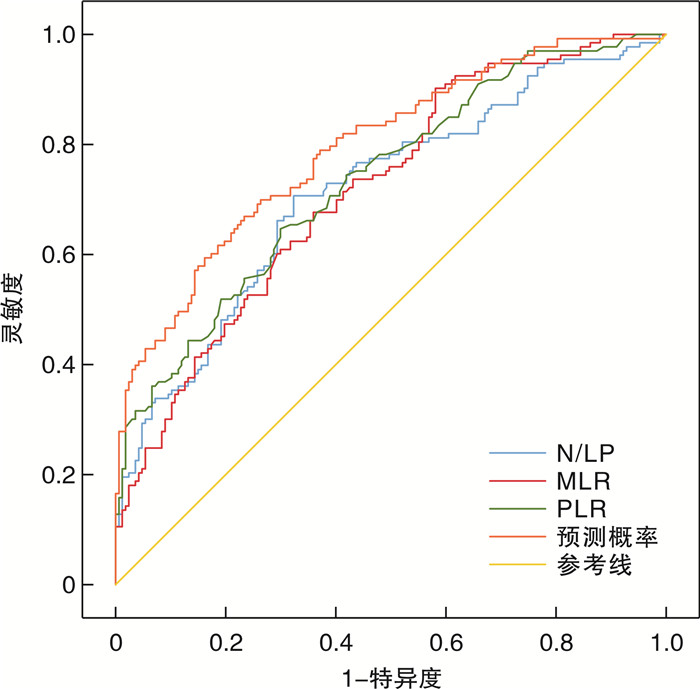
摘要: 目的 探讨外周血炎症指标中性粒细胞与淋巴细胞和血小板之间的比率(neutrophil/lymphocyte and platelet ratio,N/LP)、血小板和淋巴细胞的比率(platelet to lymphocyte ratio,PLR)、单核细胞和淋巴细胞的比率(monocytes and lymphocytes ratio,MLR)对脓毒症急性肾损伤的临床诊断及预测的价值。方法 回顾性分析收治的300例脓毒症患者的临床资料,按照改善全球肾脏病预后指南(KDIGO)定义急性肾损伤(acute kidney injury,AKI),将患者分为脓毒症急性肾损伤组(S-AKI组)和脓毒症非AKI组,比较两组间各指标差异,采用logistic回归模型分析筛选出发生AKI的独立危险因素,绘制受试者工作特征(receiver operator characteristic,ROC)曲线,并计算曲线下面积(area under the curve,AUC),评估外周血炎症指标对脓毒症肾损伤的临床预测价值。结果 ① 纳入脓毒症患者中S-AKI组133例,脓毒症非AKI组167例,S-AKI组发病率为44.33%,N/LP、PLR、MLR显著高于脓毒症非AKI组,差异有统计学意义(N/LP:Z=6.397,P<0.001;PLR:Z=6.476,P<0.001;MLR:Z=6.999,P<0.001),并且S-AKI患者28 d内病死率(46.6% vs. 26.3%)更高,合并更多的器官受损、需要更多的血管活性药物及血液透析维持,SOFA评分和APACHEⅡ评分更高(均P<0.05)。②多因素logistic回归分析发现N/LP、PLR、MLR是S-AKI发生的独立危险因素(N/LP:OR=1.03,95%CI:1.005~1.055,P=0.019;PLR:OR=1.004,95%CI:1.002~1.007,P<0.001;MLR:OR=2.344,95%CI:1.156~4.755,P=0.018);AUC分别为0.715(95%CI:0.676~0.774)、0.718(95%CI:0.661~0.775)、0.735(95%CI:0.679~0.791),均P<0.001;截断值分别为8.7、99.81和0.615,三者联合预测时ROC的AUC为0.794(95%CI:0.743~0.844,P<0.001)。结论 N/LP、MLR和PLR联合检测可评估S-AKI的发生。Abstract: Objective To study the value of the neutrophil/lymphocyte and platelet ratio(N/LP), platelet/lymphocyte ratio(PLR), monocyte and lymphocyte ratio(MLR) in clinical diagnosis and prediction of patients with acute renal impairment in sepsis.Methods The clinical data of 300 patients with sepsis were retrospectively analyzed, according to the definition of acute kidney injury(AKI) in the Guidelines for Improving Global Renal Outcomes(KDIGO), the patients were classified into two groups: S-AKI and non-AKI. Differences in all the parameters were compared between two groups.The logistic regression model was used to select independent risk factors of AKI, and a ROC curve was drawn and the AUC was calculated to assess the clinical value of peripheral inflammation in patients with septic renal injury.Results ① Among the patients with sepsis, 133 cases were included in S-AKI group and 167 cases were included in non-AKI group. The incidence in S-AKI group was 44.33%, and difference between N/LP, PLR, MLR and non-AKI was statistically significant(N/LP: Z=6.397, P<0.001; PLR: Z=6.476, P<0.001; MLR: Z=6.999, P<0.001), and S-AKI patients had higher 28-day mortality(46.6% vs. 26.3%), more organ damage, more vasoactive drugs required, and hemodialysis maintenance, resulting in higher SOFA and APACHEⅡ scores(all P<0.05). ②Multivariate logistic regression analysis indicated that the risk factors of S-AKI were N/LP, PLR and MLR. OR of N/LP=1.03, 95%CI: 1.005-1.055, P=0.019; PLR: OR=1.004, 95%CI: 1.002-1.007, P<0.001; MLR: OR=2.344, 95%CI: 1.156-4.755, P=0.018, The AUC values were 0.715(95%CI: 0.676-0.774), 0.718(95%CI: 0.661-0.775), 0.735(95%CI: 0.679-0.791)(P<0.001), and the cutoff values were 8.7, 99.81 and 0.615, respectively. The area under ROC curve for the three joint prediction was 0.794(95%CI: 0.743-0.844, P<0.001).Conclusion The combined detection of N/LP, MLR and PLR can evaluate the occurrence of S-AKI.
-
Key words:
- sepsis /
- acute kidney injury /
- inflammatory makers /
- risk factor
-

-
表 1 脓毒症非AKI组与S-AKI组临床资料比较
X±S, M(P25,P75) 指标 脓毒症非AKI组(167例) S-AKI组(133例) Z/t P 性别/例(%) 0.205 0.651 男 123(73.7) 101(75.9) 女 44(26.3) 32(24.1) 年龄/岁 76(67,84) 78(68,86.5) -1.301 0.193 呼吸频率/(次/min) 20(18,25) 20(18,26) -0.091 0.927 体温/℃ 37.57±1.06 37.56±1.08 0.116 0.908 脉搏/(次/min) 97.00±19.75 101.00±24.52 -1.683 0.094 基础疾病/例(%) 高血压 87(52.1) 72(54.1) 0.124 0.725 糖尿病 49(29.3) 48(36.1) 1.541 0.217 冠心病 37(22.2) 48(36.1) 7.080 0.008 脑梗死 40(24) 29(21.8) 0.193 0.661 主要感染来源/例(%) 肺部感染 101(60.5) 89(66.9) 1.535 0.215 腹腔感染 51(30.5) 36(27.1) 0.381 0.537 泌尿系感染 25(15) 24(18) 0.555 0.456 其他部位感染 15(9) 14(10.5) 0.202 0.653 平均动脉压/(次/min) 86.78±15.54 83.34±19.03 1.723 0.093 血生化指标 红细胞计数/(×1012/L) 3.87(3.34,4.32) 3.74(3.09,4.16) 3.474 0.001 白细胞计数/(×109/L) 15.37±8.01 16.95±8.30 -1.665 0.097 淋巴细胞计数/(×109/L) 1.40(0.84,1.95) 0.85(0.55,1.27) 8.569 <0.001 单核细胞计数/(×109/L) 0.53(0.29,0.84) 0.56(0.30,0.82) -1.478 0.139 血小板计数/(×109/L) 167(100.0,234.0) 144(90.0,212.5) 0.995 0.320 中性粒细胞计数/(×109/L) 13.38±7.52 15.14±8.00 -2.055 0.042 红细胞比积/% 35.05±7.20 32.32±8.35 3.052 0.002 N/LP 5.89(2.99,12.45) 11.97(5.45,22.98) -6.397 <0.001 PLR 135.71(72.50,213.16) 162.81(96.29,274.47) -6.476 <0.001 MLR 0.18(0.41,0.69) 0.64(0.35,1.06) -6.999 <0.001 凝血D二聚体/(mg/L) 2.21(1.22,5.02) 3.28(1.56,7.78) -3.367 0.001 白蛋白/(g/L) 32.02±5.54 32.02±6.72 -0.822 0.412 尿酸/(μmol/L) 242.89±128.75 438.80±200.72 -10.244 <0.001 血糖/(mmol/L) 8.60±4.34 9.62±5.06 -1.875 0.067 乳酸脱氢酶/(mmol/L) 228(185,322) 289(211,454.5) -3.964 <0.001 血红蛋白/(g/L) 115.84±22.93 107±27.74 2.821 0.004 总胆红素/(μmol/L) 16.3(10.9,35.9) 16.2(10.35,30.85) 0.859 0.390 胱抑素C/(mg/L) 1.28(1.00,1.61) 2.23(1.67,3.52) -10.963 <0.001 血清肌酐/(μmol/L) 73(58,90) 165(137.5,238) -14.282 <0.001 血清尿素氮/(mmol/L) 7.54(5.34,10.2) 14.93(11.33,21.52) -10.418 <0.001 降钙素原/(ng/mL) 2.09(0.50,8.55) 6.16(1.93,43.96) -5.029 <0.001 钠离子/(mmol/L) 137(134,140) 140(137,147) -4.479 <0.001 钾离子/(mmol/L) 3.84(3.5,4.25) 4.09(3.66,4.67) -3.609 <0.001 pH 7.41±0.10 7.33±0.12 4.942 <0.001 PO2/mmHga) 70(58.00,85.00) 70(57.50,86.00) 0.110 0.912 PCO2/mmHg 34.6(29.08,37.55) 33.2(27.40,38.00) 0.959 0.337 注:a)1 mmHg=0.133 kPa。 表 2 脓毒症非AKI组与S-AKI组不良事件及临床预后对比
M(P25,P75) 指标 脓毒症非AKI组(167例) S-AKI组(133例) Z/t P 住院总天数/d 11(7,20) 12(7,23) -0.700 0.484 机械通气天数/d 10(5.00,19.25) 10.5(4.00,20.00) -0.422 0.673 合并器官受累数/个 3(2.0,4.0) 6(5.0,8.5) -11.514 <0.001 血管活性药物/例(%) 75(44.9) 95(71.4) 23.248 <0.001 机械通气/例(%) 128(76.6) 113(85) 5.042 0.080 血液透析/例(%) 14(8.4) 33(24.8) 16.867 <0.001 DIC/例(%) 11(6.6) 14(10.5) 1.504 0.220 血液透析天数/d 7(2.5,15.5) 3(1.0,16.0) 0.899 0.396 SOFA评分/分 6(3,9) 16(13,22) -16.888 <0.001 APACHEⅡ评分/分 17.01±7.03 24.03±6.22 -9.031 <0.001 28 d内死亡/例(%) 44(26.3) 62(46.6) -13.312 <0.001 表 3 S-AKI相关指标的单因素、多因素logistic回归分析
指标 单因素logistic回归 多因素logistic回归 OR 95%CI P OR 95%CI P 冠心病/例(%) 0.504 0.303~0.838 0.008 0.456 0.234~0.891 0.022 红细胞计数/(×1012/L) 0.610 0.456~0.816 0.001 0.821 0.336~2.004 0.665 淋巴细胞计数/(×109/L) 0.177 0.108~0.29 <0.001 中性粒细胞计数/(×109/L) 1.032 1.001~1.063 0.045 N/LP 1.047 1.026~1.068 <0.001 1.030 1.005~1.055 0.019 PLR 1.005 1.003~1.007 <0.001 1.004 1.002~1.007 <0.001 MLR 4.093 2.414~6.941 <0.001 2.344 1.156~4.755 0.018 红细胞比积/% 0.954 0.925~0.985 0.003 0.945 0.87~1.027 0.185 血红蛋白/(g/L) 0.987 0.977~0.996 0.005 1.007 0.982~1.032 0.594 凝血D二聚体/(mg/L) 1.001 1.000~1.002 0.112 血清肌酐/(μmol/L) 1.086 1.063~1.109 <0.001 血清尿素氮/(mmol/L) 1.197 1.138~1.259 <0.001 尿酸/(μmol/L) 1.008 1.006~1.010 <0.001 胱抑素C/(mg/L) 4.562 3.041~6.845 <0.001 降钙素原/(ng/mL) 1.014 1.007~1.022 <0.001 1.016 1.007~1.024 <0.001 乳酸脱氢酶/(mmol/L) 1.001 1.000~1.001 0.024 1.000 1.000~1.001 0.614 钠离子/(mmol/L) 1.078 1.043~1.115 <0.001 1.091 1.039~1.146 <0.001 钾离子/(mmol/L) 1.776 1.281~2.463 0.001 1.659 1.090~2.525 0.018 pH 0.005 0.001~0.048 <0.001 0.028 0.001~0.639 0.025 表 4 N/LP、PLR、MLR及联合检测对S-AKI的预测价值
指标 截断值 灵敏度/% 特异度/% AUC 95%CI P 标准误 N/LP 8.700 70.70 67.70 0.715 0.676~0.774 <0.001 0.030 MLR 0.615 64.70 70.10 0.735 0.679~0.791 <0.001 0.029 PLR 99.810 90.20 41.90 0.718 0.661~0.775 <0.001 0.029 联合预测 0.370 70.00 73.70 0.794 0.743~0.844 <0.001 0.026 -
[1] Gaborit BJ, Chaumette T, Chauveau M, et al. Circulating Regulatory T Cells Expressing Tumor Necrosis Factor Receptor Type 2 Contribute to Sepsis-Induced Immunosuppression in Patients During Septic Shock[J]. J Infect Dis, 2021, 224(12): 2160-2169. doi: 10.1093/infdis/jiab276
[2] Hoste EA, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study[J]. Intensive Care Med, 2015, 41(8): 1411-1423. . doi: 10.1007/s00134-015-3934-7
[3] Nandagopal N, Reddy PK, Ranganathan L, et al. Comparison of Epidemiology and Outcomes of Acute Kidney Injury in Critically Ill Patients with and without Sepsis[J]. Indian J Crit Care Med, 2020, 24(4): 258-262. doi: 10.5005/jp-journals-10071-23386
[4] Wiersema R, Jukarainen S, Vaara ST, et al. Two subphenotypes of septic acute kidney injury are associated with different 90-day mortality and renal recovery[J]. Crit Care, 2020, 24(1): 150. doi: 10.1186/s13054-020-02866-x
[5] Xie J, Wang H, Kang Y, et al. The Epidemiology of Sepsis in Chinese ICUs: A National Cross-Sectional Survey[J]. Crit Care Med, 2020, 48(3): e209-e218. doi: 10.1097/CCM.0000000000004155
[6] Shi Y, Yang C, Chen L, et al. Predictive value of neutrophil-to-lymphocyte and platelet ratio in in-hospital mortality in septic patients[J]. Heliyon, 2022, 8(11): e11498. doi: 10.1016/j.heliyon.2022.e11498
[7] 苏丽娜, 车晓宇, 王金环, 等. 外周血血小板与淋巴细胞比值胱抑素C及降钙素原对脓毒症继发急性肾损伤的预测价值研究[J]. 山西医药杂志, 2022, 51(21): 2438-2440.
[8] Zarbock A, Nadim M K, Pickkers P, et al. Sepsis-associated acute kidney injury: consensus report of the 28th Acute Disease Quality Initiative workgroup[J]. Nat Rev Nephrol, 2023, 19(6): 401-417. doi: 10.1038/s41581-023-00683-3
[9] Chang YM, Chou YT, Kan WC, et al. Sepsis and Acute Kidney Injury: A Review Focusing on the Bidirectional Interplay[J]. Int J Mol Sci, 2022, 23(16): 9159. doi: 10.3390/ijms23169159
[10] Kwak SH, Ahn S, Shin MH, et al. Identification of Biomarkers for the Diagnosis of Sepsis-Associated Acute Kidney Injury and Prediction of Renal Recovery in the Intensive Care Unit[J]. Yonsei Med J, 2023, 64(3): 181-190. doi: 10.3349/ymj.2022.0324
[11] Font MD, Thyagarajan B, Khanna AK. Sepsis and Septic Shock-Basics of diagnosis, pathophysiology and clinical decision making[J]. Med Clin North Am, 2020, 104(4): 573-585. doi: 10.1016/j.mcna.2020.02.011
[12] Jacobi J. The pathophysiology of sepsis-2021 update: Part 1, immunology and coagulopathy leading to endothelial injury[J]. Am J Health Syst Pharm, 2022, 79(5): 329-337. doi: 10.1093/ajhp/zxab380
[13] Zanza C, Caputo G, Tornatore G, et al. Cellular Immuno-Profile in Septic Human Host: A Scoping Review[J]. Biology(Basel), 2022, 11(11): 1626.
[14] Liu S, Li Y, She F, et al. Predictive value of immune cell counts and neutrophil-to-lymphocyte ratio for 28-day mortality in patients with sepsis caused by intra-abdominal infection[J]. Burns Trauma, 2021, 9: tkaa040. doi: 10.1093/burnst/tkaa040
[15] Shimoyama Y, Umegaki O, Kadono N, et al. Presepsin Values Predict Septic Acute Kidney Injury, Acute Respiratory Distress Syndrome, Disseminated Intravascular Coagulation, and Shock[J]. Shock, 2021, 55(4): 501-506. doi: 10.1097/SHK.0000000000001664
[16] Gameiro J, Fonseca JA, Jorge S, et al. Neutrophil, lymphocyte and platelet ratio as a predictor of mortality in septic-acute kidney injury patients[J]. Nefrologia(Engl Ed), 2020, 40(4): 461-468.
[17] Xiao W, Lu Z, Liu Y, et al. Influence of the Initial Neutrophils to Lymphocytes and Platelets Ratio on the Incidence and Serverity of Sepsis Associated Acute Kidney A Double Robust Estimation Based on a Large Public Database[J]. Front Immunol, 2022, 13: 925494. doi: 10.3389/fimmu.2022.925494
[18] Kazem N, Hofer F, Koller L, et al. The age-specific prognostic impact of the platelet-to-lymphocyte ratio on long-term outcome after acute coronary syndrome[J]. Eur Heart J Open, 2022, 2(1): b31.
[19] Platini H, Ferdinand E, Kohar K, et al. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Prognostic Markers for Advanced Non-Small-Cell Lung Cancer Treated with Immunotherapy: A Systematic Review and Meta-Analysis[J]. Medicina(Kaunas), 2022, 58(8): 1069.
[20] Schobert IT, Savic LJ, Chapiro J, et al. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios as predictors of tumor response in hepatocellular carcinoma after DEB-TACE[J]. Eur Radiol, 2020, 30(10): 5663-5673. doi: 10.1007/s00330-020-06931-5
[21] Thorup CV, Christensen S, Hvas AM. Immature Platelets As a Predictor of Disease Severity and Mortality in Sepsis and Septic Shock: A Systematic Review[J]. Semin Thromb Hemost, 2020, 46(3): 320-327. doi: 10.1055/s-0039-3400256
[22] Shimoyama Y, Umegaki O, Kadono N, et al. Presepsin and platelet to lymphocyte ratio predict the progression of septic subclinical acute kidney injury to septic acute kidney injury: a pilot study[J]. BMC Res Notes, 2022, 15(1): 212. doi: 10.1186/s13104-022-06103-2
[23] Napolitano L, Barone B, Reccia P, et al. Preoperative monocyte-to-lymphocyte ratio as a potential predictor of bladder cancer[J]. J Basic Clin Physiol Pharmacol, 2022, 33(6): 751-757. doi: 10.1515/jbcpp-2022-0179
[24] Jakubowska K, Koda M, Grudzinska M, et al. Monocyte-to-lymphocyte ratio as a prognostic factor in peripheral whole blood samples of colorectal cancer patients[J]. World J Gastroenterol, 2020, 26(31): 4639-4655. doi: 10.3748/wjg.v26.i31.4639
[25] 马丽, 黄从新. 单核细胞/淋巴细胞比率与冠状动脉病变程度相关性的临床研究[J]. 心血管病学进展, 2020, 41(5): 542-546.
[26] 李艳秀, 刘云, 周春雷, 等. 单核细胞/淋巴细胞比值作为重症患者30 d死亡及不良事件预测指标的相关研究[J]. 中华危重病急救医学, 2021, 33(5): 582-586.
[27] Jiang F, Lei J, Xiang J, et al. Monocyte-to-lymphocyte ratio: a potential novel predictor for acute kidney injury in the intensive care unit[J]. Ren Fail, 2022, 44(1): 1004-1011. doi: 10.1080/0886022X.2022.2079521
-




 下载:
下载: