Predictive value of changes of blood TRAF6 and NF-κB levels in patients with acute pancreatitis for extrapancreatic complication acute lung injury
-
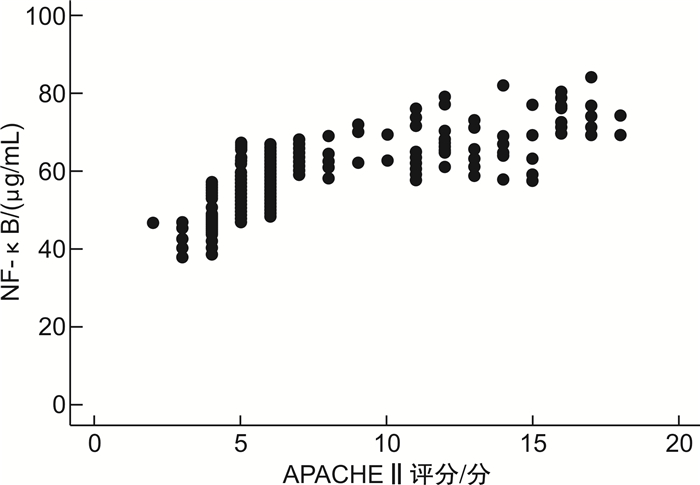
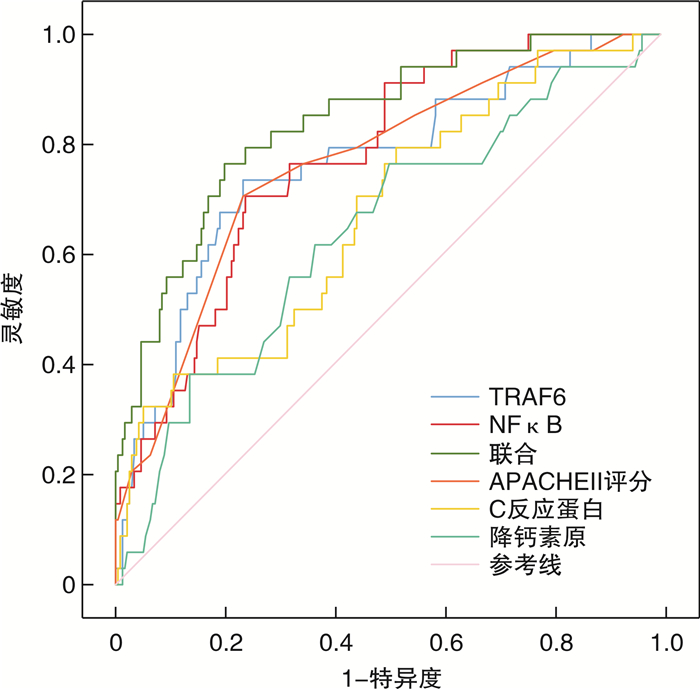
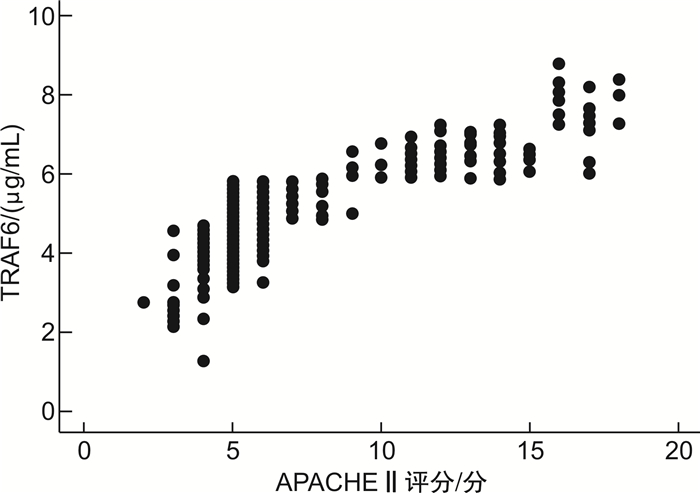
摘要: 目的 探讨急性胰腺炎(acute pancreatitis,AP)患者血肿瘤坏死因子受体相关因子6(tumor necrosis factor receptor related factor 6,TRAF6)、核转录因子-κB(nuclear factor kappa B,NF-κB)水平变化对胰外并发症急性肺损伤(acute lung injury,ALI)的预测价值。方法 选取2021年8月—2023年3月在我院诊治的AP患者269例为研究组,选取同期健康体检者269例为对照组。两组均检测血清TRAF6、NF-κB水平。研究组根据《中国急性胰腺炎诊治指南(2021)》相关标准分为轻症AP(mild AP,MAP)和重症AP(severe SAP,SAP),并采用急性生理学与慢性健康状况评分系统Ⅱ(acute physiology and chronic health status scoring system Ⅱ,APACHEⅡ)评估患者病情程度,分析TRAF6、NF-κB与APACHEⅡ评分的相关性。统计研究组ALI发生率,对比不同发生时间的ALI患者TRAF6、NF-κB水平。分析继发ALI的影响因素。绘制受试者工作曲线(receiver operating curve,ROC)评估TRAF6、NF-κB预测ALI的价值。结果 研究组治疗前、治疗24 h血清TRAF6、NF-κB水平高于对照组(P<0.05)。研究组治疗24 h血清TRAF6、NF-κB水平低于治疗前(P<0.05)。MAP患者、SAP患者治疗24 h血清TRAF6、NF-κB水平及APACHEⅡ评分低于治疗前(P<0.05)。治疗前、治疗24 h SAP患者血清TRAF6、NF-κB水平及APACHEⅡ评分高于MAP患者(P<0.05)。治疗前TRAF6、NF-κB与APACHEⅡ评分呈正相关(P<0.05)。研究组269例患者中34例发生ALI,发生率为12.65%。≤24 h出现ALI患者的治疗前、治疗24 h TRAF6、NF-κB均高于>24 h出现ALI患者的水平(P<0.05)。调整混杂因素后治疗前TRAF6、NF-κB水平升高仍会增加AP患者ALI发生风险(P<0.05)。TRAF6、NF-κB联合评估AP患者发生ALI的AUC值大于单独评估值(P<0.05)。结论 AP患者血清TRAF6、NF-κB水平与病情程度呈正相关,且对预测ALI具有较高价值,且二者水平越高,继发ALI的时间越早。
-
关键词:
- 急性胰腺炎 /
- 肿瘤坏死因子受体相关因子6 /
- 核转录因子-κB /
- 病情程度 /
- 急性肺损伤
Abstract: Objective To investigate the predictive value of changes of blood tumor necrosis factor receptor related factor 6(TRAF6) and nuclear factor kappa B(NF-κB) levels in patients with acute pancreatitis(AP) for acute lung injury(ALI) caused by extrapancreatic complications.Methods A total of 269 AP patients diagnosed and treated in our hospital from August 2021 to March 2023 were selected as the study group, and 269 healthy subjects during the same period were selected as the control group. Serum TRAF6 and NF-κB levels were detected in both groups. The study group was divided into mild AP(MAP) and severe SAP(SAP) according to the Chinese Guidelines for Diagnosis and Treatment of Acute Pancreatitis(2021). The acute physiology and chronic health status scoring system Ⅱ(APACHEⅡ) was used to evaluate the severity of the disease, and the correlation of TRAF6, NF-κB and APACHEⅡ score was analyzed. The incidence of ALI in the study group was analyzed. The levels of TRAF6 and NF-κB in ALI patients with different onset time were compared. The influencing factors of secondary ALI were analyzed. Receiver operating curve(ROC) was plotted to evaluate the value of TRAF6 and NF-κB in predicting ALI.Results Serum TRAF6 and NF-κB levels in the study group were higher than those in the control group before treatment and within 24 h after treatment(P < 0.05). The levels of serum TRAF6 and NF-κB in the study group at 24 h after treatment were lower than before treatment(P < 0.05). Serum TRAF6, NF-κB levels and APACHEⅡ scores in MAP and SAP patients were lower than before treatment at 24 h(P < 0.05). Serum TRAF6, NF-κB levels and APACHEⅡ scores in SAP patients were higher than those in MAP patients before treatment and 24 h after treatment(P < 0.05). TRAF6, NF-κB were positively correlated with APACHEⅡ scores(P < 0.05). There was a positive correlation between TRAF6, NF-κB and APACHEⅡ scores before treatment(P < 0.05). ALI occurred in 34 of 269 patients in the study group(12.65%). The levels of TRAF6 and NF-κB in patients complicated with ALI within 24 h before treatment and 24 h after treatment were higher than those in patients with ALI>24 h(P < 0.05). After adjusting for confounding factors, the elevated expression of TRAF6 and NF-κB before treatment still increased the risk of ALI occurrence in AP patients(P < 0.05). The AUC value of ALI in AP patients assessed by combination of TRAF6 and NF-κB was higher than that assessed by each alone(P < 0.05).Conclusion Serum levels of TRAF6 and NF-κB in AP patients are positively correlated with the severity of the disease, and they have great value in predicting ALI. The higher the level of both, the earlier the time of secondary ALI. -

-
表 1 两组患者血清TRAF6、NF-κB水平比较
X±S 组别 TRAF6/(μg/mL) NF-κB/(pg/mL) 研究组(269例) 治疗前 5.15±1.21 59.29±8.17 治疗24 h 4.06±1.15 38.72±7.41 t 10.289 31.002 P <0.001 <0.001 对照组(269例) 2.78±0.64 11.34±2.21 t1 28.397 92.920 P1 <0.001 <0.001 t2 15.951 58.075 P2 <0.001 <0.001 注:t1、P1为研究组治疗前vs.对照组;t2、P2为研究组治疗24 h vs.对照组。 表 2 MAP、SAP患者血清TRAF6、NF-κB水平及APACHEⅡ评分比较
X±S 组别 例数 TRAF6/(μg/mL) NF-κB/(pg/mL) APACHEⅡ评分/分 MAP 189 治疗前 4.75±1.20 55.91±8.09 5.29±1.14 治疗24 h 3.54±0.91 35.40±5.47 3.28±1.10 t 11.046 28.873 17.443 P <0.001 <0.001 <0.001 SAP 80 治疗前 6.09±1.291) 67.28±9.241) 12.64±3.281) 治疗24 h 5.26±0.621) 46.58±5.131) 10.41±2.981) t 5.187 17.519 4.501 P <0.001 <0.001 <0.001 与MAP患者比较,1)P<0.05。 表 3 不同发生时间的ALI患者TRAF6、NF-κB水平比较
X±S 发生时间 例数 TRAF6/(μg/mL) NF-κB/(pg/mL) 治疗前 治疗24 h 治疗前 治疗24 h ≤24 h 17 6.64±1.21 5.68±1.10 69.92±7.96 49.22±7.61 >24 h 17 5.80±1.04 4.74±1.14 63.82±7.63 42.36±7.30 t 2.171 2.447 2.281 2.682 P 0.038 0.020 0.029 0.012 表 4 研究组是否发生ALI患者临床资料比较
X±S 资料 ALI(34例) 无ALI(235例) 统计值 P 性别/例(%) χ2=0.001 0.978 男 18(52.94) 125(53.19) 女 16(47.06) 110(46.81) 年龄/岁 63.09±5.87 59.97±5.44 t=3.095 0.002 BMI/(kg/m2) 24.92±2.01 24.06±1.95 t=2.394 0.017 吸烟史/例(%) 7(20.59) 94(40.00) χ2=4.773 0.029 饮酒史/例(%) 13(38.24) 85(36.17) χ2=0.055 0.815 病因/例(%) χ2=0.231 0.973 酒精性 6(17.65) 39(16.60) 高脂性 7(20.59) 51(21.70) 胆源性 15(44.12) 110(46.81) 其他 6(17.65) 35(14.89) 胸腔积液/例(%) 20(58.82) 68(28.94) χ2=12.054 0.001 腹腔感染/例(%) 13(38.24) 27(11.49) χ2=16.785 <0.001 入院时血糖/(mmol/L) 10.23±2.39 8.12±2.64 t=4.405 <0.001 入院时舒张压/mmHga) 83.04±8.67 82.11±7.84 t=0.638 0.524 入院时收缩压/mmHg 127.83±13.05 130.57±11.89 t=1.240 0.216 APACHEⅡ评分/分 10.29±3.39 7.07±3.01 t=5.736 <0.001 白细胞计数/(×109/L) 13.62±2.29 12.99±2.08 t=1.630 0.104 C反应蛋白/(mg/L) 190.65±64.62 151.37±57.81 t=3.647 <0.001 降钙素原/(μg/L) 0.64±0.20 0.55±0.18 t=5.671 <0.001 白蛋白/(g/L) 29.98±6.37 33.62±6.74 t=2.963 0.003 钙离子/(mmol/L) 1.62±0.36 1.81±0.38 t=2.742 0.007 血淀粉酶/(U/L) 1568.37±464.05 1396.84±498.33 t=1.892 0.060 尿淀粉酶/(U/L) 8059.24±739.54 7839.85±761.29 t=1.576 0.116 治疗前TRAF6/(μg/mL) 6.22±1.23 5.00±1.21 t=5.484 <0.001 治疗24h TRAF6/(μg/mL) 5.21±1.13 3.89±1.08 t=6.623 <0.001 治疗前NF-κB/(pg/mL) 66.87±8.10 58.19±8.19 t=5.784 <0.001 治疗24h NF-κB/(pg/mL) 45.79±7.28 37.70±7.54 t=5.872 <0.001 注:a)1 mmHg=0.133 kPa。 表 5 分析TRAF6、NF-κB与ALI的独立关系
因素 β SE Wald χ2 P OR 95%CI 模型1 TRAF6 Q1 1 Q2 0.761 0.361 4.443 0.042 2.140 1.263~3.627 Q3 0.917 0.389 5.556 0.033 2.502 1.578~3.966 Q4 1.014 0.345 8.635 0.015 2.756 1.898~4.002 NF-κB Q1 1 Q2 0.787 0.349 5.082 0.039 2.196 1.322~3.649 Q3 0.929 0.346 7.212 0.022 2.532 1.554~4.127 Q4 1.049 0.351 8.927 0.008 2.854 1.855~4.391 模型2 TRAF6 Q1 1 Q2 0.792 0.359 4.865 0.041 2.207 1.298~3.754 Q3 0.930 0.381 5.955 0.029 2.534 1.604~4.003 Q4 1.071 0.350 9.370 0.005 2.919 1.879~4.536 NF-κB Q1 1 Q2 0.815 0.352 5.361 0.036 2.259 1.341~3.806 Q3 0.948 0.321 8.730 0.010 2.582 1.528~4.362 Q4 1.029 0.318 10.469 <0.001 2.798 1.699~4.608 模型3 TRAF6 Q1 1 Q2 0.827 0.349 5.616 0.032 2.287 1.340~3.902 Q3 0.994 0.345 8.295 0.019 2.701 1.726~4.227 Q4 1.102 0.325 11.496 <0.001 3.010 1.903~4.761 NF-κB Q1 1 Q2 0.834 0.340 6.010 0.027 2.301 1.362~3.889 Q3 0.980 0.319 9.435 0.003 2.664 1.574~4.509 Q4 1.331 0.357 13.909 <0.001 3.786 1.832~4.826 注:模型1无调整混杂因素,模型2调整年龄、BMI、吸烟史、胸腔积液、腹腔感染,模型3调整年龄、BMI、吸烟史、白蛋白、钙离子、胸腔积液、腹腔感染、入院时血糖、APACHEⅡ评分、C反应蛋白、降钙素原。 表 6 分析TRAF6、NF-κB对AP患者发生ALI的预测价值
参数 AUC 95%CI Z P cut-off值 灵敏度/% 特异度/% TRAF6 0.763 0.708~0.813 5.611 <0.001 >5.61 μg/mL 73.53 76.60 NF-κB 0.774 0.719~0.822 7.025 <0.001 >63.53 pg/mL 70.59 76.17 TRAF6、NF-κB联合 0.840 0.791~0.882 9.400 <0.001 76.47 80.00 APACHEⅡ评分 0.763 0.708~0.813 5.938 <0.001 >9分 70.59 76.60 C反应蛋白 0.672 0.612~0.728 3.424 <0.001 >145.27 mg/L 79.41 48.51 降钙素原 0.641 0.581~0.699 2.697 <0.001 >0.55 μg/L 76.47 49.79 -
[1] 徐晨, 何精选, 石珍, 等. 急性胰腺炎患者外周血lncRNA H19表达与Th17/Treg平衡的关系[J]. 临床急诊杂志, 2022, 23(5): 316-320+326. https://lcjz.whuhzzs.com/article/doi/10.13201/j.issn.1009-5918.2022.05.004
[2] 中华医学会外科学分会胰腺外科学组. 中国急性胰腺炎诊治指南(2021)[J]. 浙江实用医学, 2021, 26(6): 511-519, 535. doi: 10.16794/j.cnki.cn33-1207/r.2021.06.003
[3] 李涛, 费素娟. 实验室指标对急性胰腺炎发生器官衰竭的预测价值[J]. 中国中西医结合消化杂志, 2021, 29(3): 218-221. doi: 10.3969/j.issn.1671-038X.2021.03.13
[4] Xu C, Zhang J, Liu J, et al. Proteomic analysis reveals the protective effects of emodin on severe acute pancreatitis induced lung injury by inhibiting neutrophil proteases activity[J]. J Proteomics, 2020, 220(1): 103760.
[5] 韦碧薇, 龚雅慧, 苏州, 等. miR-125b参与TRAF6影响的人胰腺导管上皮屏障作用[J]. 基础医学与临床, 2021, 41(9): 1272-1276. doi: 10.16352/j.issn.1001-6325.2021.09.012
[6] 郑传明, 王振杰, 杜召辉, 等. miR-146a靶向TRAF6继而抑制AR42J细胞的增殖及凋亡[J]. 中国处方药, 2022, 20(2): 33-35. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCF202202012.htm
[7] Liu X, Lin Z, Xu Y. Pellino1 promoted inflammation in lung injury model of sepsis by TRAF6/ NF-κB signal pathway[J]. J Inflamm(Lond), 2021, 18(1): 11. doi: 10.1186/s12950-021-00276-6
[8] 中国危重病急救医学. 急性肺损伤/急性呼吸窘迫综合征诊断和治疗指南(2006)[J]. 中国危重病急救医学, 2006, 18(12): 706-710. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHNK200705044.htm
[9] Iyer H, Elhence A, Mittal S, et al. Pulmonary complications of acute pancreatitis[J]. Expert Rev Respir Med, 2020, 14(2): 209-217. doi: 10.1080/17476348.2020.1698951
[10] Yu B, Li J, Li N, et al. Progression to recurrent acute pancreatitis after a first attack of acute pancreatitis in adults[J]. Pancreatology, 2020, 20(7): 1340-1346. doi: 10.1016/j.pan.2020.09.006
[11] 李勋, 王厚清, 许铁. 重症急性胰腺炎患者入院24小时后新发急性呼吸窘迫综合征的危险因素分析[J]. 临床内科杂志, 2022, 39(1): 22-25. https://www.cnki.com.cn/Article/CJFDTOTAL-LCLZ202201008.htm
[12] 景光旭, 梁鸿寅, 黄竹, 等. 重症急性胰腺炎相关肺损伤机制与治疗的研究进展[J]. 中国普通外科杂志, 2022, 31(3): 405-409. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ202203014.htm
[13] 吴浪, 陈升鑫, 张贯军, 等. NMI通过NF-κB信号通路促进急性胰腺炎炎症反应[J]. 现代消化及介入诊疗, 2022, 27(9): 1141-1146. https://www.cnki.com.cn/Article/CJFDTOTAL-XDXH202209012.htm
[14] 陈三洋, 宋耀东, 崔宗朝, 等. 过表达TRIM27通过抑制NFκB/MAPK信号通路减轻小鼠重症急性胰腺炎[J]. 中华急诊医学杂志, 2022, 31(9): 1186-1192.
[15] Wu YC, Hsu SP, Hu MC, et al. PEP-sNASP Peptide Alleviates LPS-Induced Acute Lung Injury Through the TLR4/TRAF6 Axis[J]. Front Med(Lausanne), 2022, 9(1): 832713.
[16] 陈芳荣, 吴栋才, 陈小菊. miR-146a-5p抑制TRAF6/NF-кB信号通路影响滋养细胞的炎症反应[J]. 海南医学院学报, 2021, 27(6): 410-415. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYY202106003.htm
[17] Ge P, Luo Y, Okoye CS, et al. Intestinal barrier damage, systemic inflammatory response syndrome, and acute lung injury: A troublesome trio for acute pancreatitis[J]. Biomed Pharmacother, 2020, 132(1): 110770.
[18] Yang S, Song Y, Wang Q, et al. Daphnetin ameliorates acute lung injury in mice with severe acute pancreatitis by inhibiting the JAK2-STAT3 pathway[J]. Sci Rep, 2021, 11(1): 11491.
[19] 沈琪琦, 童小文, 王伟, 等. 重症急性胰腺炎患者外周血miR-21-3p、miR-22-3p与并发肺损伤的相关性[J]. 西部医学, 2021, 33(7): 987-991. https://www.cnki.com.cn/Article/CJFDTOTAL-XIBU202107010.htm
[20] 董小鹏, 王丽娟, 赵春霖, 等. 血必净注射液对急性胰腺炎大鼠肺损伤及肺组织TLR4、NF-κB、TNF-α表达的影响[J]. 中成药, 2020, 42(11): 3025-3030. https://www.cnki.com.cn/Article/CJFDTOTAL-ZCYA202011039.htm
[21] 万朝辉, 曾良, 周辉, 等. 重楼皂苷Ⅶ通过抑制NF-κB信号通路对重症急性胰腺炎大鼠急性肺损伤的保护作用[J]. 吉林大学学报(医学版), 2022, 48(3): 668-675. https://www.cnki.com.cn/Article/CJFDTOTAL-BQEB202203015.htm
[22] 唐永军, 张红玉, 吴勤奋. 血清miR-98-5p、TRAF6 mRNA表达与脓毒症并发肺损伤的关系[J]. 山东医药, 2022, 62(25): 11-15. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202225003.htm
[23] 唐晋, 周靖, 陈雪梅, 等. miR-98-5p通过靶向调控TRAF6表达促进肺泡巨噬细胞M2表型分化以保护脓毒症引起的急性肺损伤[J]. 免疫学杂志, 2020, 36(8): 645-654. https://www.cnki.com.cn/Article/CJFDTOTAL-MYXZ202008001.htm
[24] 魏焱, 陈炯, 陈秋星. 老年重症急性胰腺炎病人急性肺损伤的危险因素分析[J]. 腹部外科, 2018, 31(1): 52-55. https://www.cnki.com.cn/Article/CJFDTOTAL-FBWK201801012.htm
-




 下载:
下载: