Comparison of safety and efficacy of different antiplatelet regimens in minor acute stroke
-
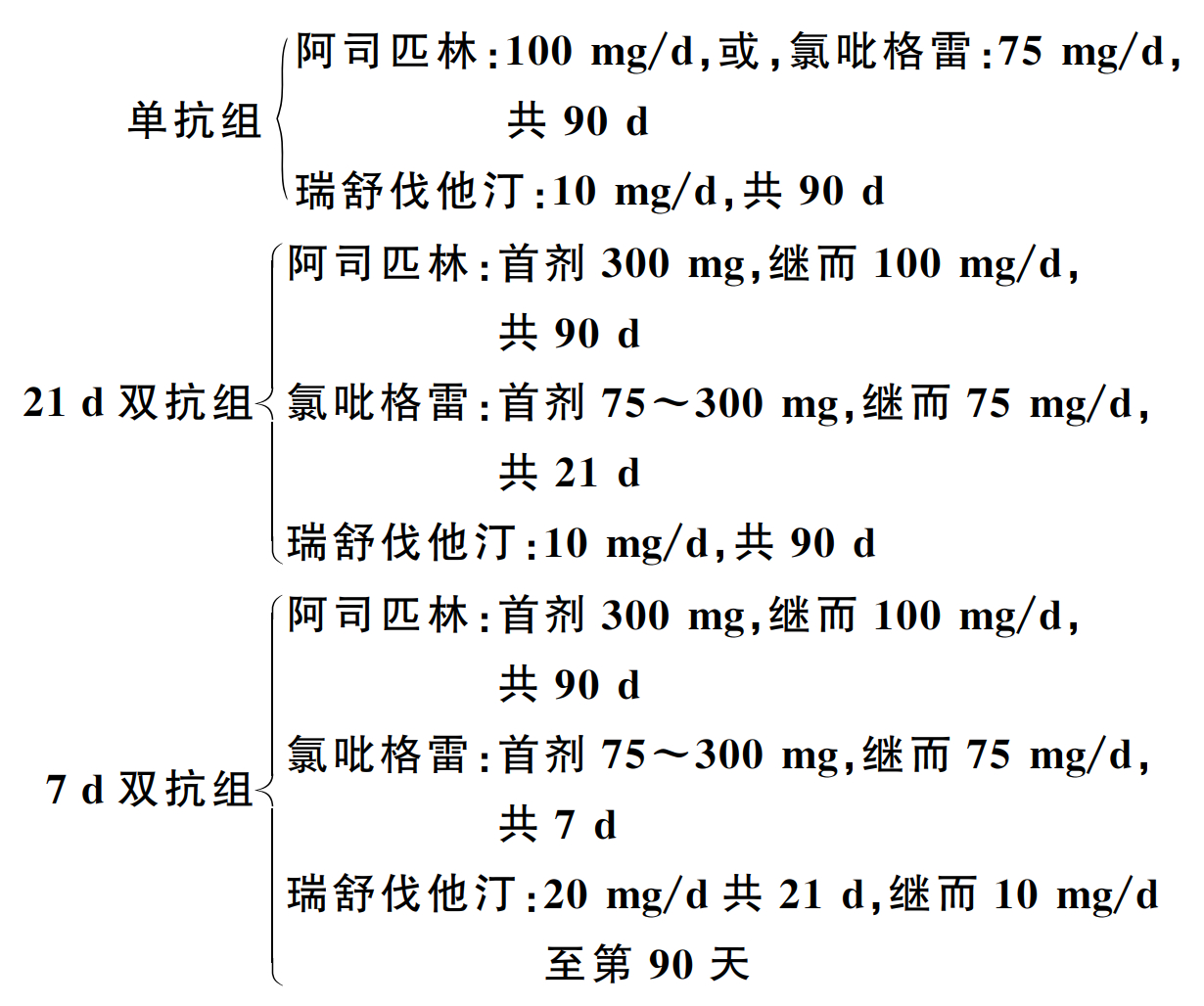
摘要: 目的 探讨3种不同抗血小板方案治疗轻型急性缺血性脑卒中(acute ischemic stroke,AIS)的安全性和有效性,以便对AIS进行更精准的抗血小板治疗。方法 登记2017年1月1日—2019年12月31日期间我院急诊科诊治的轻型AIS患者资料,根据治疗方案不同分为单抗组[单抗血小板治疗(SAPT)+瑞舒伐他汀]、21 d双抗组[21 d双抗血小板治疗(DAPT)+瑞舒伐他汀]和7 d双抗组(7 d DAPT +强化瑞舒伐他汀)。主要观察指标为随访90 d内再发脑梗死事件、出血事件,以及他汀相关性肝损害和他汀相关性肌病(statin-associated myopathy,SAM)。结果 ① 再发脑梗死比较:单抗组26例(20.00%),21 d双抗组4例(5.97%),7 d双抗组7例(8.05%);与单抗组比较,21 d双抗组(HR=0.271,95%CI:0.095~0.776,P=0.015)及7 d双抗组(HR=0.367,95%CI:0.159~0.847,P=0.019)明显降低了再发脑梗死风险;而21 d双抗组与7 d双抗组比较差异无统计学意义(HR=0.737,95%CI:0.216~2.518,P=0.627)。②出血事件比较:单抗组1例(0.77%),21 d双抗组6例(8.96%),7 d双抗组2例(2.30%),3组比较差异有统计学意义(χ2=8.198,P=0.008);21 d双抗组与单抗组比较,差异有统计学意义(P=0.007),7 d双抗组与单抗组比较,差异无统计学意义(P=0.566);尽管21 d双抗组与7 d双抗组比较,差异无统计学意义(P=0.079),但21 d双抗组出血事件发生率(8.96%)明显高于7 d双抗组(2.30%)。③随访期间3组患者中均未发现他汀相关性肝损害和SAM病例。结论 7 d DAPT +强化瑞舒伐他汀是轻型AIS最佳治疗方案,在降低再发脑梗死风险方面与21 d DAPT +瑞舒伐他汀方案具有同等效应,且极少导致出血及他汀相关性肝损害及SAM等不良事件的发生。Abstract: Objective The aim of this study was to evaluate the safety and efficacy of three different antiplatelet regimens in minor acute ischemic stroke(AIS), in order to provide a more accurate antiplatelet therapy for AIS.Methods Patients with minor AIS in the emergency department of our hospital from January 2017 to December 2019 were registered and divided into three groups according to the different therapy regimens: single antiplatelet therapy(SAPT) group(SAPT + rosuvastatin), 21-day dual antiplatelet therapy(DAPT) group(21-day DAPT + rosuvastatin), and 7-day DAPT group(7-day DAPT + intensive rosuvastatin). The primary outcomes were recurrent cerebral infarction, bleeding events, statin-induced liver injury and statin-associated myopathy(SAM) during 90-day follow-up in an intention-to-treat analysis.Results ① Recurrent cerebral infarction: there were 26 cases(20.00%) in the SAPT group, 4 cases(5.97%) in the 21-day DAPT group, and 7 cases(8.05%) in the 7-day DAPT group; Compared to the SAPT group, the risk of recurrent cerebral infarction was significantly reduced in the 21-day DAPT group(hazard ratio[HR], 0.271; 95% confidence interval[CI], 0.095-0.776; P=0.015) and the 7-day DAPT group(HR, 0.367; 95%CI, 0.159-0.847; P=0.019), while there was no significant difference between the 21-day DAPT group and the 7-day DAPT group(HR, 0.737; 95%CI, 0.216-2.518; P=0.627). ②Bleeding events: there was 1 case(0.77%) in the SAPT group, 6 cases(8.96%) in the 21-day DAPT group, and 2 cases(2.30%) in the 7-day DAPT group. There was a significant difference between the three groups(χ2=8.198, P=0.008); There was a statistically significant difference between the 21-day DAPT group and the SAPT group(P=0.007), while there was no significant difference between the 7-day DAPT group and the SAPT group(P=0.566); Although there was no significant difference between the 21-day DAPT group and the 7-day DAPT group(P=0.079), the incidence of bleeding events in the 21-day DAPT group(8.96%) was significantly higher than that in the 7-day DAPT group(2.30%). ③No cases of statin-induced liver injury and SAM were recorded in the three groups during the follow-up.Conclusion 7-day DAPT + intensive rosuvastatin was the best therapy regimen for minor AIS, which had the same effect as the regimen of 21-day DAPT + rosuvastatin in reducing the risk of recurrent cerebral infarction for patients with minor AIS, and rarely leads to bleeding events, statin-induced liver injury and SAM.
-

-
表 1 3组患者基础资料比较
基础资料 总样本
(n=284)单抗组
(n=130)21 d双抗组
(n=67)7 d双抗组
(n=87)P 年龄/岁 67.49±11.85 68.75±12.96 65.93±11.49 66.82±10.22 0.347 女性/例(%) 68(23.94) 34(31.07) 14(16.01) 20(20.79) 0.693 发病时间/h 21.62±1.28 21.21±1.86 20.33±2.48 23.14±2.48 0.513 收缩压/mmHga) 156.68±26.94 156.59±29.65 158.03±28.29 166.78±21.28 0.836 舒张压/mmHg 90.98±17.68 89.99±18.44 90.94±18.57 92.47±15.84 0.317 bNIHSS 3.01±0.95 2.91±0.94 2.07±1.02 3.10±0.90 0.205 治疗前ALT/(U/L) 17.0(12.2,23.0) 16.1(11.7,22.6) 18.5(12.0,28.3) 17.0(12.9,22.4) 0.483 治疗前AST/(U/L) 16.6(13.0,22.5) 17.0(12.9,22.9) 15.4(11.9,20.3) 16.9(14.0,22.0) 0.258 治疗前CK/(U/L) 78.0(55.5,112.0) 78.0(56.0,117.0) 78.0(58.5,114.5) 77.0(54.0,100.5) 0.778 治疗2周后ALT/(U/L) 17.6(12.0,26.2) 16.3(11.2,24.4) 21.3(14.7,28.4) 17.1(12.6,25.6) 0.056 治疗2周后AST/(U/L) 16.7(13.2,21.5) 16.8(13.2,21.2) 16.3(13.0,21.7) 16.9(13.5,21.9) 0.932 治疗2周后CK/(U/L) 69.0(48.5,101.0) 69.0(47.0,99.0) 68.0(48.5,91.5) 71.0(49.0,102.5) 0.806 注:a)1 mmHg=0.133 kPa。 表 2 再发缺血性脑卒中比较
方案 β SE Wald χ2 自由度 P HR 95%CI 下限 上限 3组治疗方案 9.792 2 0.007 21 d双抗组vs. 单抗组 -1.306 0.537 5.913 1 0.015 0.271 0.095 0.776 7 d双抗组vs. 单抗组 -1.001 0.426 5.527 1 0.019 0.367 0.159 0.847 21 d双抗组vs. 7 d双抗组 -0.305 0.627 0.237 1 0.627 0.737 0.216 2.518 表 3 出血事件比较
组别 统计学方法 χ2 Pa) 21 d双抗组vs. 7 d双抗组vs. 单抗组 Fisher's Exact Test 8.198 0.008 21 d双抗组vs. 单抗组 Fisher's Exact Test 0.007 7 d双抗组vs. 单抗组 Fisher's Exact Test 0.566 21 d双抗组vs. 7 d双抗组 Fisher's Exact Test 0.079 注:a)3组列联表拆分成3个四格表,故检验水准校正为α’=0.05/[k(k-1)/2]=0.0167(其中k为组数3);由于存在“最小理论频数可能小于5”,故采用Fisher确切概率法进行分析。 表 4 治疗前与治疗2周后ALT、AST及CK比较
组别 项目 均值 标准差 标准误 95%CI 统计量 P 下限值 上限值 单抗组 ALT -1.382 24.501 2.149 -5.633 2.870 -0.643 0.521 AST 1.062 49.849 4.372 -7.589 9.712 0.243 0.809 CK 51.785 311.767 27.344 -2.316 105.885 1.894 0.060 21 d双抗组 ALT -3.643 15.012 1.834 -7.305 0.018 -1.987 0.051 AST -1.628 11.525 1.408 -4.440 1.183 -1.157 0.252 CK 15.985 50.438 6.162 3.682 28.288 2.594 0.012 7 d双抗组 ALT -1.421 15.572 1.670 -4.740 1.898 -0.851 0.397 AST -0.341 10.550 1.131 -2.590 1.907 -0.302 0.764 CK 6.069 36.149 3.876 -1.635 13.773 1.566 0.121 -
[1] GBD Lifetime Risk of Stroke Collaborators, Feigin VL, Nguyen G, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016[J]. N Engl J Med, 2018, 379(25): 2429-2437. doi: 10.1056/NEJMoa1804492
[2] 王拥军, 李子孝, 谷鸿秋, 等. 中国卒中报告2020(中文版)(1)[J]. 中国卒中杂志, 2022, 17(5): 433-447. doi: 10.3969/j.issn.1673-5765.2022.05.001
[3] Sun T, Chen SY, Wu K, et al. Trends in incidence and mortality of stroke in China from 1990 to 2019[J]. Front Neurol, 2021, 12: 759221. doi: 10.3389/fneur.2021.759221
[4] Zhang Y, Guan YL, Zhang YJ, et al. Recurrence rate and relevant associated factors of stroke among patients with small artery occlusion in Northern China[J]. Sci Rep, 2019, 9(1): 2834. doi: 10.1038/s41598-019-39207-0
[5] 《中国脑卒中防治报告》编写组. 《中国脑卒中防治报告2019》概要[J]. 中国脑血管病杂志, 2020, 17(5): 272-281. doi: 10.3969/j.issn.1672-5921.2020.05.008
[6] 《中国脑卒中防治报告》编写组. 《中国脑卒中防治报告2020》概要[J]. 中国脑血管病杂志, 2022, 19(2): 136-144. doi: 10.3969/j.issn.1672-5921.2022.02.011
[7] Wang YJ, Wang YL, Zhao XQ, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack[J]. N Engl J Med, 2013, 369(1): 11-19. doi: 10.1056/NEJMoa1215340
[8] Johnston SC, Easton JD, Farrant M, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA[J]. N Engl J Med, 2018, 379(3): 215-225. doi: 10.1056/NEJMoa1800410
[9] Wang D, Gui L, Dong Y, et al. Dual antiplatelet therapy may increase the risk of non-intracranial haemorrhage in patients with minor strokes: a subgroup analysis of the CHANCE trial[J]. Stroke Vasc Neurol, 2016, 1(2): 29-36. doi: 10.1136/svn-2016-000008
[10] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2014[J]. 中华神经科杂志, 2015, 48(4): 246-257. doi: 10.3760/cma.j.issn.1006-7876.2015.04.002
[11] Ghandehari K. Challenging comparison of stroke scales[J]. J Res Med Sci, 2013, 18(10): 906-910.
[12] GUSTO Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction[J]. N Engl J Med, 1993, 329(10): 673-682. doi: 10.1056/NEJM199309023291001
[13] 中华医学会, 中华医学会杂志社, 中华医学会全科医学分会, 等. 血脂异常基层诊疗指南(实践版·2019)[J]. 中华全科医师杂志, 2019, 18(5): 417-421. doi: 10.3760/cma.j.issn.1671-7368.2019.05.004
[14] Tournadre A. Statins, myalgia, and rhabdomyolysis[J]. Joint Bone Spine, 2020, 87(1): 37-42. doi: 10.1016/j.jbspin.2019.01.018
[15] Libby P. Mechanisms of acute coronary syndromes and their implications for therapy[J]. N Engl J Med, 2013, 368(21): 2004-2013. doi: 10.1056/NEJMra1216063
[16] Libby P, Pasterkamp G, Crea F, et al. Reassessing the mechanisms of acute coronary syndromes[J]. Circ Res, 2019, 124(1): 150-160. doi: 10.1161/CIRCRESAHA.118.311098
[17] 施仲伟. 阿司匹林在心血管疾病预防中的应用现状[J]. 中华消化杂志, 2020, 40(5): 292-295. doi: 10.3760/cma.j.cn311367-20200323-00166
[18] Campbell CL, Smyth S, Montalescot G, et al. Aspirin dose for the prevention of cardiovascular disease: a systematic review[J]. JAMA, 2007, 297(18): 2018-2024. doi: 10.1001/jama.297.18.2018
[19] Maffrand JP. The story of clopidogrel and its predecessor, ticlopidine: could these major antiplatelet and antithrombotic drugs be discovered and developed today?[J]. Comptes Rendus Chimie, 2012, 15(8): 737-743. doi: 10.1016/j.crci.2012.05.006
[20] 朱雯雯, 李莺, 周小玉. 血栓弹力图评估心脑血管疾病抗血小板药物使用疗效的影响因素[J]. 临床血液学杂志, 2023, 36(4): 225-230. doi: 10.13201/j.issn.1004-2806.2023.04.001
[21] Li Y, Jing QM, Wang B, et al. Extended antiplatelet therapy with clopidogrel alone versus clopidogrel plus aspirin after completion of 9-to 12-month dual antiplatelet therapy for acute coronary syndrome patients with both high bleeding and ischemic risk. Rationale and design of the OPT-BIRISK double-blinded, placebo-controlled randomized trial[J]. Am Heart J, 2020, 228: 1-7. doi: 10.1016/j.ahj.2020.07.005
[22] Ullah W, Zahid S, Sandhyavenu H, et al. Extended, standard, or De-escalation antiplatelet therapy for patients with coronary artery disease undergoing percutaneous coronary intervention?A trial-sequential, bivariate, influential, and network meta-analysis[J]. Eur Heart J Cardiovasc Pharmacother, 2022, 8(7): 717-727. doi: 10.1093/ehjcvp/pvac020
[23] Condello F, Liccardo G, Ferrante G. Clinical effects of dual antiplatelet therapy or aspirin monotherapy after acute minor ischemic stroke or transient ischemic attack, a meta-analysis[J]. Curr Pharm Des, 2021, 27(40): 4140-4146. doi: 10.2174/1381612827666210728102459
[24] Ringler J, Steck M, Shah SP, et al. Indications and evidence for dual antiplatelet therapy after acute ischemic stroke[J]. Crit Care Nurs Q, 2020, 43(2): 122-137. doi: 10.1097/CNQ.0000000000000298
[25] Borén J, Chapman MJ, Krauss RM, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel[J]. Eur Heart J, 2020, 41(24): 2313-2330. doi: 10.1093/eurheartj/ehz962
[26] Mollazadeh H, Tavana E, Fanni G, et al. Effects of statins on mitochondrial pathways[J]. J Cachexia Sarcopenia Muscle, 2021, 12(2): 237-251. doi: 10.1002/jcsm.12654
[27] 姚宇, 王文军, 梁玉灵. 他汀类药物对70例肺栓塞患者预后的影响[J]. 山东大学学报(医学版), 2020, 58(11): 76-80. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYB202011013.htm
[28] Räber L, Taniwaki M, Zaugg S, et al. Effect of high-intensity statin therapy on atherosclerosis in non-infarct-related coronary arteries(IBIS-4): a serial intravascular ultrasonography study[J]. Eur Heart J, 2015, 36(8): 490-500. doi: 10.1093/eurheartj/ehu373
[29] Kilit C, Koçak FE, Paşalı Kilit T. Comparison of the effects of high-dose atorvastatin and high-dose rosuvastatin on oxidative stress in patients with acute myocardial infarction: a pilot study[J]. Turk Kardiyol Dern Ars, 2017, 45(3): 235-243.
[30] Nenna A, Nappi F, Lusini M, et al. Effect of statins on platelet activation and function: from molecular pathways to clinical effects[J]. Biomed Res Int, 2021, 2021: 6661847.
[31] Vavlukis A, Vavlukis M, Dimovski A, et al. Anti-inflammatory and immunomodulatory effects of rosuvastatin in patients with low-to-moderate cardiovascular risk[J]. Acta Pharm, 2022, 72(2): 303-315. doi: 10.2478/acph-2022-0018
[32] Lee SH, Shin HS, Oh I. The protective effects of statins towards vessel wall injury caused by a stent retrieving mechanical thrombectomy device: a histological analysis of the rabbit carotid artery model[J]. J Korean Neurosurg Soc, 2021, 64(5): 693-704. doi: 10.3340/jkns.2020.0303
[33] Christophe B, Karatela M, Sanchez J, et al. Statin therapy in ischemic stroke models: a meta-analysis[J]. Transl Stroke Res, 2020, 11(4): 590-600. doi: 10.1007/s12975-019-00750-7
[34] Cheng ZJ, Dai TM, Shen YY, et al. Atorvastatin pretreatment attenuates ischemic brain edema by suppressing aquaporin 4[J]. J Stroke Cerebrovasc Dis, 2018, 27(11): 3247-3255. doi: 10.1016/j.jstrokecerebrovasdis.2018.07.011
[35] Rodriguez F, Maron DJ, Knowles JW, et al. Association between intensity of statin therapy and mortality in patients with atherosclerotic cardiovascular disease[J]. JAMA Cardiol, 2017, 2(1): 47-54. doi: 10.1001/jamacardio.2016.4052
[36] Amarenco P, Bogousslavsky J, Callahan A 3rd, et al. High-dose atorvastatin after stroke or transient ischemic attack[J]. N Engl J Med, 2006, 355(6): 549-559. doi: 10.1056/NEJMoa061894
[37] Kiortsis DN, Filippatos TD, Mikhailidis DP, et al. Statin-associated adverse effects beyond muscle and liver toxicity[J]. Atherosclerosis, 2007, 195(1): 7-16. doi: 10.1016/j.atherosclerosis.2006.10.001
[38] 吕晓东, 贡联兵. 瑞舒伐他汀[J]. 中国新药杂志, 2002, 11(8): 650-651. doi: 10.3321/j.issn:1003-3734.2002.08.024
-




 下载:
下载:
